
|
|
|
CASE REPORT / CAS CLINIQUE
ANEURYSMAL BONE CYST OF THE SPINE
KYSTE ANEUVRISMAL DU RACHIS. A PROPOS D'UN CAS
E-Mail Contact - PATEL Chirag K. :
viragpat@yahoo.com
ABSTRACT Aneurysmal bone cysts of the spine are benign, highly vascular osseous lesions of unknown origin that may present difficult diagnostic and therapeutic challenges. They are expansile lesions containing thin-walled, blood-filled cystic cavities that cause bone destruction and sometimes spinal deformity and neurological compromise. The treatment of aneurysmal bone cysts of the spine remains controversial according to the literature. We describe a case of a fourteen year old girl with back pain and paraspinal swelling of two weeks duration. Radiological studies revealed an aneurysmal bone cyst which was confirmed by biopsy. Treatment included excision and grafting of the defect with cancellous bone and instrumentation of the deformity. Abbreviations used in the paper: ABC = aneurysmal bone cyst, CT = computerized tomography, MR = magnetic resonance RESUME Les kystes anévrysmaux du rachis sont de nature bénigne. Ils sont richement vascularisés et sont d’origine inconnue posant des difficultés diagnostiques et thérapeutiques. Ces lésions expansives contenant des collections kystiques aux fines parois osseuses peuvent entrainer une destruction, parfois une deformation avec un risque neurologique. Le traitement reste controversé. Keywords : Aneurysmal bone cyst, Spine tumor, kyste anévrismal, tumeur, rachis INTRODUCTION Aneurysmal Bone Cyst (ABC) is a rare localized tumor of the long bones and spinal vertebrae. It was first described by Jaffe and Lichtenstein in 1942 (12). This tumor is found at onset in childhood and early adolescence with a slight preponderance to females (2,7) It constitutes 1.4% of all primary bone tumors and 15% of all primary spine tumors (1,6). It commonly involves the metaphyses of long bones (proximal humerus, femur, tibia) and the flat bones of the pelvis. In the spine it commonly involves the neural arch (20). The cyst is occasionally associated with other tumors of the bone, such as osteoblastoma, osteosarcoma, giant cell tumor and fibrous dysplasia (7,14) and has occasionally been reported to occur at a site of previous trauma to the bone (5). There is tendency towards rapid growth with local expansion, which can exert pressure on an adjacent structure (20). ABC in the spine are generally diagnosed within a few months after the onset of clinical symptoms which include local pain, swelling, muscle stiffness and restriction of movement (15). Rarely in advanced cases does the ABC exert pressure on the spinal cord which can lead to neurologic deficits (17,18,19). Here we describe the diagnosis, management and follow-up of an ABC in a 14 yr old girl. CASE REPORT A 14 yr old girl complained of swelling in the left paraspinal region for a period of two weeks. She also had numbness in the left leg. There was no history of pain or trauma. On examination, the girl was in good general condition. There was a single, fluctuant, tender swelling at the level of T12 in the left paraspinal region. The lower thoracic and upper lumber spine was tender without muscle spasm. Muscle power, sensation and deep tendon reflexes of the lower extremities were normal. Rectal and genital examination were also normal. A complete blood count was normal. An X-ray of the thoracolumbar spine showed destruction of the left pedicle of L1 vertebra with associated paravertebral mass. There was also erosion of the L1 vertebral body. Ultrasonography of the mass suggested a superficial lesion of mixed echogenicity with a fluid level. Spinal computed tomography of the thoraco-lumbar spine showed a mass eroding the posterior elements of the vertebrae at the level of L1 with expansion into the vertebral body of L1 on the left. The lesion was multiloculated, entered the spinal canal and was pressing the cord. A tentative diagnosis of Aneurysmal Bone Cyst was made. 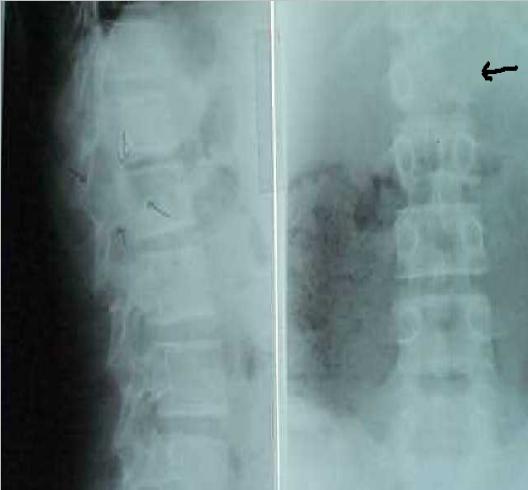 Figure 1 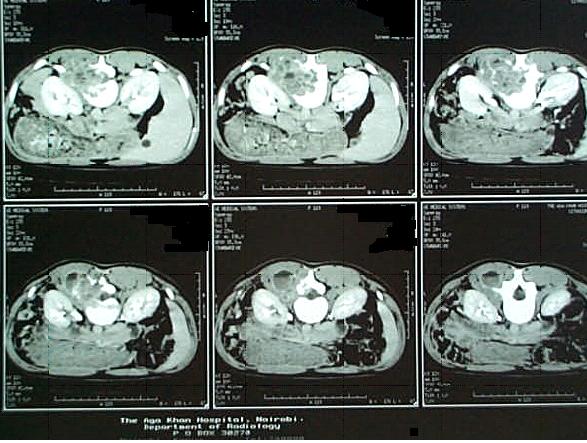 Figure 2
During surgical exploration of the spine at level of T12 and L1, a gray-red fleshy mass 4 cm long with multiple blood filled cysts was found invading the L1 vertebra through the left lamina. The tumor was extradural, attached to the dura but easily separable from it. Cauterization and curettage of the cyst by way of a laminectomy was done. The patient made a good postoperative recovery. Histology of the cyst showed it to be a tumor characterized by spindle cell stroma within which were present a number of dilated blood vessels lined by attenuated epithelium. There were aggregates of giant cells, spicules of osteoid a number of which were calcified. 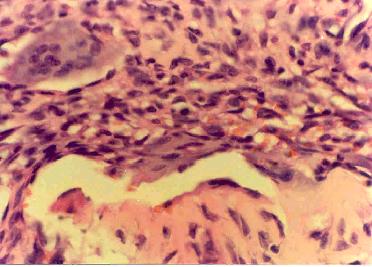 Figure 4 On follow up at six weeks the girl presented in the casualty with complaints of back pain and pins and needles sensation in both legs. Neurologically the tone, power, reflexes and sensation in the lower limbs were normal. A repeat MRI of the spine suggested residual tumor or recurrence. A second exploration was carried out with curettage of the residual mass. The patient recovered well and was discharged home with intact neurology. A rigid thoraco-lumbar orthosis was tailor made, to be worn when out of bed. At 3 months follow up it was noticed that the patient had developed kyphus deformity at the T9 level. Power in the legs was grade 3. Sensation was intact. X-ray revealed vertebral body collapse with reduction in height of L1 vertebrae.  Figure 5 The patient was operated for T12-L3 spinal fusion with Hartshill rectangle with rib bone grafting of L1 vertebrae. A check x-ray done post-operatively was noted to show malalignment. This appears to have set in during the immediate pre-operative period (prior to date of spinal fusion). A check x-ray just before surgery would ideally have picked this up. The patient’s postoperative follow up course was uneventful and she rapidly regained strength in both legs. She continued to be mobilized with a rigid thoraco-lumbar brace. At 1 yr follow up examination the girl has resumed normal daily activities, is pain free and neurologically intact. She has gradually been weaned off the brace. DISCUSSION An ABC is an uncommon expansile osteolytic lesion of bone consisting of a proliferation of vascular tissue that forms a lining around a blood filled cystic lesion. It is clinically important because it is easily mistaken for a malignancy pathologically in its early to mid-phase. In 20 to 30 % of cases, an aneurysmal bone cyst may be associated with an underlying tumor i.e. osteosarcoma, giant cell tumor, chondrosarcoma, fibrous dysplasia etc (7,14,16). It has been suggested that ABC is not a true neoplasm but rather a vascular malformation. These cysts are generally thought of as a secondary vascular phenomenon superimposed on a preexisting lesion, which presumably initiates a periosteal or intraosseous arteriovenous malformation (1,3,9). The resultant haemodynamic forces generated by high-pressure vascular channels rapidly erode the osseous trabeculae into a cystic cavity. Clinically the patient usually presents with pain and stiffness of the spine. Palpable mass is seen in only 6% of cases. On radiographs the lesion demonstrates loss of pedicle of involved vertebrae (1). The preferred method for evaluation of an ABC is magnetic resonance imaging which can provide as much or more information than a CT scan (4). The differential diagnosis of back pain in children are other tumors of bone such as osteoblastoma, osteoid osteoma, giant cell tumor and fibrous dysplasia. Non-neoplastic causes are osteomyelitis, juvenile rheumatoid arthritis, SLE, Scheuermann disease (16). In our patient the lesion was diagnosed earlier because of presence of localised swelling. However in patients presenting with just low back pain without neurological manifestations or external signs, a high index of suspicion for bony lesion is required and earlier examination, including CT or MRI, should be done. The optimal treatment of aneurysmal bone cysts of the spine remains a subject of controversy. Treatment options for aneurysmal bone cysts have included simple curettage with or without bone grafting, complete excision, embolisation, radiation therapy or a combination of these modalities (20,21). Treatment of ABC with simple curettage can result in obliteration of the cyst (20). Curettage and bone graft has a 20 % recurrence rate, which can be managed with more aggressive curettage or excision (21). If postoperative deformity develops surgical stabilization is indicated (20). The clinical course of aneurysmal bone cysts is sometimes unpredictable and local recurrences have been described after various types of treatments (2). Radiotherapy can also be used effectively in patients who are resistant to surgical treatment or are at high risk for surgery (13). However, possibility of complications such as sarcomatous change, myelopathy, deformation of vertebrae make this mode of treatment less desirable (10). Selective embolisation of the tumor is possible in large tumors that have high risk of bleeding and in places where curettage would be difficult (8). Intra-lesional injection of sclerosing agents is also an effective method for treatment of ABC. Overall cure rates of 87% have been achieved (11). The prognosis of ABC in children is good although there is a high recurrence rate mainly in the 1st year after operation and in patients who undergo partial resection of the tumor (1,2). Therefore these children require careful follow-up and might need additional treatment. REFERENCES
|
© 2002-2018 African Journal of Neurological Sciences.
All rights reserved. Terms of use.
Tous droits réservés. Termes d'Utilisation.
ISSN: 1992-2647
