
|
|
|
CASE REPORT / CAS CLINIQUE
HYPOMELANOSIS OF ITO: A CASE REPORT FROM EAST AFRICA
HYPOMELANOSIS D'ITO . A PROPOS D'UN CAS OBSERVE EN AFRIQUE DE L'EST
E-Mail Contact - MWANIKI .K. Michael :
michael.kivkiv@gmail.com
ABSTRACT Hypomelanosis of Ito (HI) is the third most common neurocutaneous disorder. HI is thought to be more common in non-white/pigmented population. However only one case seems to have been reported from Africa and no case has been reported from East or Central Africa. We describe a case of a 12 years old girl seen at our centre with hypo-pigmented whorls over most of her trunk and limbs following the lines of blaschko typical of HI. She had learning disability and musculo-skeletal anomalies. Key words: Hypomelanosis of Ito, Neurocutaneous disease. RESUME Hypomelanosis d’Ito (HI) est le tiers la plupart de désordre neurocutaneous commun. SALUT est pensé pour être plus commun dans la population de non-white/pigmented. De quelque manière que seulement un cas semble avoir été rapporté d’Afrique et aucun cas n’a été rapporté d’Afrique centrale est ou. Nous décrivons un cas d’une fille âgée de 12 ans vue à notre centre avec les spirales hypo-pigmentées plus de la plupart de son tronc et membres après les lignes du blaschko typiques du HI. Elle a eu l’incapacité d’étude et les anomalies musculo-squelettiques Mots clés : Hypomelanosis d’Ito, la maladie de Neurocutaneous. INTRODUCTION Hypomelanosis of Ito (HI) is thought to be the third most common neurocutaneous disorder after neurofibromatosis type1 and tuberous sclerosis. Recent literature suggests that this condition may be under reported. It is thought to be more common in people with pigmented skins, but there is only one case report from Africa. Whether this is due to low prevalence or under recognition and underreporting of this condition in the region remains unclear. CASE REPORT A 12-year-old girl who presented to Kilifi District Hospital on the Kenyan coast with a history of seizures and bizarre behaviour. “Fits” were described as episodes of suddenly falling down from undisturbed sitting position, which often recurred. These episodes were brief, followed by rapid and complete recovery within a minute. No post- ictal activity was reported. The bizarre behaviour was described as lack of sleep with the child remaining awake during the night, making unintelligible sounds and crying inconsolably. These complaints had been present for the last year. Past medical history revealed that the child had previously been hospitalised with a similar complaint. The pregnancy and birth history was uneventful. The child was born at home and at term. She is the fifth born. Developmental history revealed marked delay in achieving all her milestones: head control was not achieved till about the age of 7 months, the child did not sit till almost the age of 2 years, and took even longer to walk. This was achieved well passed the 5th birthday of the child. A sibling born two years following this child walked before her. Physiotherapy was commenced on account of delayed walking but was later discontinued. She is not toilet trained and has not acquired speech. No such illness has been seen in the family as a far as the guardian could recall and no one in the family suffers from epilepsy or any other familial disorder. Examination findings On clinical examination she did not appear wasted, however she weight 24.7kg (below 3rd percentile) for her age and sex. Her head circumference was 54.6cm (above 97th percentile for age and sex). She had hypo-pigmented whorls over most trunk and the limbs following the blaschko lines (Figure 1). These skin lesions according to the mother were present since when the child was about one year of age. The mother did not have these whorls and did not recall of any other relatives with similar skin features. The child had a contracture of the right ankle joint, which was held in fixed planter flexion. Examination of the respiratory and cardiovascular systems revealed no abnormalities. The child appeared to have global developmental delay, could not follow commands and showed little evidence of social interaction. She lacked expressive speech and only made guttural noises. The vision appeared normal in that the child would grasp an object placed in front of her, but the visual acuity could not be assessed. It was also not possible to fully assess the auditory function, however free field-audio testing suggested that the child could hear. She had exaggerated knee jerk reflexes and bilateral ankle clonus. The plantar reflex was equivocal bilaterally. She could stand with support using mainly the left leg but could not walk. There were no anomalies noted on the head and spine. The rest of the examination was normal. Diagnostic evaluation A full blood count and electrolytes were normal. An electro encephalograph (EEG) revealed slow waves distributed globally with frontal spikes (Figure 2). Computerized Tomography scan of the brain showed normal cerebral and cerebellar hemispheres, normal ventricular system and no space-occupying lesion. DISCUSSION Ito first described Hypomelanosis of Ito (HI) in 1952. The characteristic feature are the cutaneous zone of hypo-pigmentation following the lines of blaschko with varied clinical presentation. The most common complications reported are developmental delay and epilepsy. Infantile spasms in the first year of life and autistic behaviour as also been documented. Other reported anomalies include ocular, musculoskeletal, oral and urogenital malformations. No universally accepted diagnostic criteria for HI exist. One suggestion was that the criteria should include dermatological lesions plus non-dermatological abnormalities especially of the central nervous system (CNS) and skeletal or chromosomal abnormalities. These criteria exclude cases with only dermatological manifestations. Skin lesions suggestive of HI have been described without or with variable degree of systemic manifestation and this complicates the establishment of a diagnostic criteria. Numerous complications have been associated with this condition involving the central nervous system, ocular, musculoskeletal oral alteration and urogenital malformation. Many chromosomal abnormalities have been reported in association with HI and the presence of two genetically different cell lines is thought to be a common factor. Though the condition is thought to be more frequent in dark skinned races very few cases have been reported in Africa. We could only identify only one case from West Africa from a Medline search , but none from East or Central Africa. This may be due to a low prevalence or underreporting, but since this condition is easily recognizable in Africans, more attempts should be made to report such cases.  Figure 1: Hypopigmented whorls on anterior trunk. 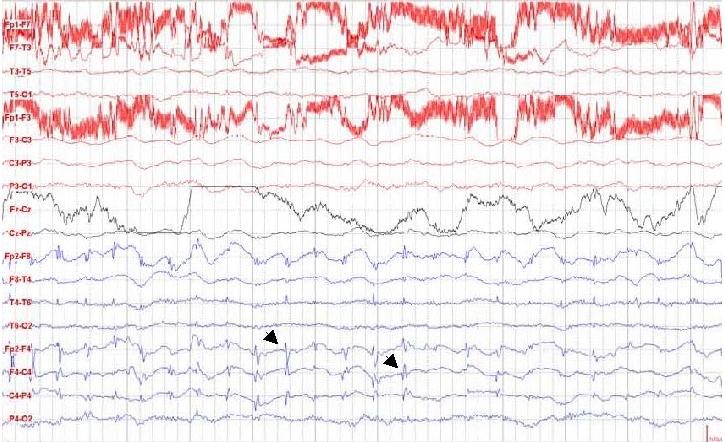 Figure 2: EEG showing spikes in the frontal area. (See arrows) REFERENCES
|
© 2002-2018 African Journal of Neurological Sciences.
All rights reserved. Terms of use.
Tous droits réservés. Termes d'Utilisation.
ISSN: 1992-2647