TECHNIQUES
TRANS-SINUSAL FRONTAL APPROACH FOR OLFACTORY GROOVE MENINGIOMAS
ABORD TRANS-SINUSIEN FRONTAL DANS LA CHIRURGIE DES MENINGIOMES OLFACTIFS
- Department of neurosurgery, Faculty of medicine of Annaba, Algeria
ABSTRACT
Background
We report on our experience with the trans-sinusal frontal approach in removing olfactory groove meningiomas in the department of neurosurgery of Univesity Hospital Center of Annaba (Algeria).
Methods
Ten tumours were operated on by the trans-sinusal frontal approach, using a bicoronal incision, tree tumours developed on one side, and there were seven bilateral olfactosellar tumours. Our procedure : steotomy of the anterior wall of the frontal sinus was performed with an oscillating saw. The posterior wall of the sinus was resected and the tumour was removed through a real subfrontal route along the plane of the anterior skull base. Ethmoidal blood supply was early controlled at the initial stages of the operation, allowing avascular tumour debulking. Tumour extensions toward the sella and the optic canals were removed without brain retraction.
Results
Seven patients made a good neurologic recovery. Two was dead in the 24 hours after intervention and one four days after. Olfactory nets were preserved on the contralateral side in unilateral tumours.
Conclusions
The trans-sinusal frontal approach represents an excellent way for tumours developed in the central anterior skull base, especially for olfactory groove meningiomas, whatever their size.
KEYWORDS: Anterior skull base, Meningioma, olfactory groove meningioma, Technique, Trans-sinusal frontal approach
RESUME
Introduction
Nous rapportons notre expérience de la chirurgie des méningiomes olfactifs par voie trans-sinusale frontale, dans le service de neurochirurgie du CHU Annaba (Algérie).
Matériel et méthodes
Dix tumeurs ont été opérées par cette approche en utilisant une incision bicoronale. Il s’agit d’une étude rétrospective couvrant la période 2001-2007 sur une période de six ans. Trois tumeurs avaient un développement unilatéral et sept bilatérales olfactosellaires. La technique suivante a été utilsée : ostéotomie de la paroi antérieure du sinus frontal à l’aide de la scie oscillante puis résection de la paroi postérieure. Ablation de la tumeur par abord sous-frontal le long de la partie horizontale médiane de l’étage antérieur. Le contrôle de la vascularisation tumorale se fait très tôt et l’ablation de la tumeur est peu hémorragique. Les parties de la tumeur à extensions vers les nerfs optiques et la région sellaire sont enlevés sans aucune rétraction du cerveau.
Résultat
Sept patients ont présenté une amélioration neurologique et deux patients sont décédés dans les 24 heures. Dans les tumeurs à développement unilatéral nous avons préservé les filets olfactifs controlatéraux.
Conclusion
L’approche trans-sinusale représente une excellente voie pour les tumeurs développées dans la partie centrale de l’étage antérieure de la base du crâne. En particulier les méningiomes olfactifs quelques soit leurs taille.
Mots clés: Abord trans-sinusal frontal, Etage antérieur de la base du crâne, Méningiomes olfactifs, Technique.
INTRODUCTION
The first successful removal of olfactory groove meningioma is attributed to an Italian surgeon, Francesco Durante in 1885. H. Cushing in 1938 reported on a series of 28 cases operated on through a unilateral frontal craniotomy and subfrontal approach (9).
The unilateral or bilateral frontal craniotomy is always preferred by some neurosurgeons (16), sometimes associated with orbital rim osteotomy to decrease brain retraction (3,11,22). The other preferred surgical approach is the pterional route (1,14,15,26).
The trans-sinusal frontal approach has been used for reconstruction of the traumatic lesions of craniofacial borders (4,25). The authors have extended the indications for intradural tumors of the anterior floor of the skull base, in particular olfactory groove and olfactosellar meningiomas (5,12,13).
MATERIALS AND METHODS
Clinical Material
Ten patients, aged between 35 and 71 years old, were operated on using the trans-sinusal frontal approach over a 6 year period, 2001-2007. Seven tumours developed on one side, and there were tree bilateral olfactosellar. Clinical presentation and outcome are summarized in Table 1.
Table 1. Series Characteristics
| Case |
Sex |
Age |
Presentation |
Localisation |
Histology |
Outcome |
| 1 |
F |
44 |
Coma |
bilateral |
Meningothelial |
Normal |
| 2 |
F |
48 |
Epilepsy |
unilateral |
Psammomateux |
Normal |
| 3 |
F |
42 |
Headaches/Visual lost |
bilateral |
Psammomateux |
Normal |
| 4 |
M |
52 |
Headaches |
bilateral |
Meningothelial |
Normal |
| 5 |
F |
60 |
Headaches/Vertigos |
bilateral |
Meningothelial |
Dead |
| 6 |
F |
35 |
Headaches/Visual lost |
bilateral |
Meningothelial |
Normal |
| 7 |
F |
66 |
Headaches |
bilateral |
Meningothelial |
Dead |
| 8 |
F |
71 |
Headaches |
unilateral |
Meningothelial |
Normal |
| 9 |
F |
52 |
Headaches |
unilateral |
Meningothelial |
Normal |
| 10 |
M |
67 |
Headaches/Vertigos |
bilateral |
Meningothelial |
Dead |
Surgical Technique
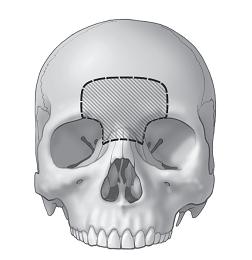
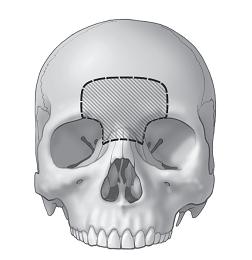
Figure 1
SUPERFICIAL EXPOSURE
The patient was placed in the supine position, with the head fixed in a Mayfield-Kees, the neck extended to angle the head backward toward the floor.
The line of incision with the hair shaved was infiltrated with 2% xylocaine with adrenaline. The skin incision was bicoronal, extending from one tragus to the other.
The scalp was elevated in the plane of cleavage between the frontalis muscle and the periosteum to the upper limits of the frontal sinus. The entire scalp was raised forward to expose the supraorbital ridge bilaterally and the nasal process of the frontal bone up to the fronto-naso-maxillary suture in the midline. A large free fragment of periosteum was taken from the area posterior to the scalp incision.
OSTEOPLASTIC FLAP
The anterior wall of the frontal sinus was cut monobloc with an oscillating saw. The anterior wall was lifted with a periosteal elevator and a chisel inserted as levers above through the bone cut into the frontal sinus. Intersinus septa were broken. For small frontal sinus, bone flap extended beyond the limits of the sinus, including the external layer of the frontal vault cut tangentially. The mucous membranes of the sinus were resected to the frontonasal orifices where they were coagulated. The entire mucosal and inner cortical lining of the anterior and posterior walls of the sinus were removed.
The posterior wall of the sinus was perforated, and the dura mater was dissected from the undersurface of the posterior wall, which was removed. The dura mater was separated from the crista galli, which was removed with rongeurs. The working space included the anterior floor of the skull with the medial orbital walls and orbital roofs laterally on each side, and the anterior aspect of the ethmoid in the center (fig.1).
TUMOR RESECTION
The dura mater was opened in V at the junction between the convexity and the base. The falx with the origin of the superior sagittal sinus was ligated and cut. The olfactory nets, invaded by the tumour, were coagulated during the control of the ethmoidal vessels. The olfactory tracts were protected on the healthy side, when the tumour was developed on one side. We proceeded to hollow the tumour by fragmentation.
At the completion of the debulking, the dural attachment was carefully coagulated.
All these surgical manoeuvres were made without any risk to the frontal lobes detached away from the orbital roofs and ethmoid by gravity. The tumour capsule was loosened back to the sphenoid wing, which served as a landmark to progress medially to the anterior clinoid processes and the optic nerves. The operating microscope was set up.
A plane of arachnoidal dissection was allowed to free the posterior pole of the tumour gradually from the frontal parenchyma, the frontopolar arteries, which were dissected and coagulated, and from the optic nerves in the optic foramina. Tumour fragments overhanging the tuberculum sellae and diving in the direction of the diaphragm sellae were carefully dissected away from the pituitary stalk.
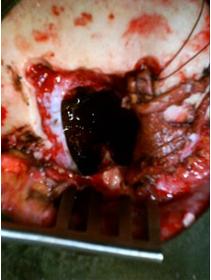
Wide moistened cottons introduced between the posterior pole of the tumour and the brain maintained the frontal lobes at some distance, avoiding any instrumental brain retraction (Fig.2,3,4,5).

Figure 2

Figure 3
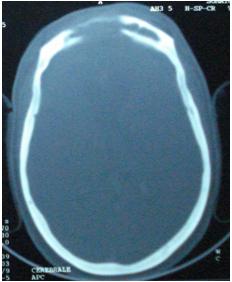
Figure 4
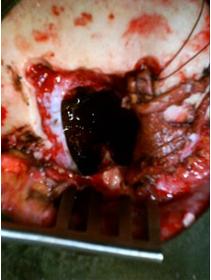
Figure 5
CLOSURE
Osseous reconstruction of the skull base with bone was unnecessary. Frontonasal ducts were occluded by means of osseous fragments and periosteum. The dura mater was reconstructed with a periosteum graft sutured as watertight as possible. A wide fragment of periosteum was affixed within the deadspace between the frontobasal dura mater and the anterior wall of the sinus. The frontal curve was reconstituted by repositioning the anterior wall of the frontal sinus, so that the bevelled bone edges were in good approximation, maintained by two transosseous sutures and covered with the periosteum sutured to the temporal fascia laterally. The scalp was closed in the usual manner.
RESULTS
Eight patients made a good neurologic recovery; intellectual impairment disappeared within 1 month, and visual acuity normalized within 4 weeks. Two was dead in the 24 hours after intervention. Olfactory nets were preserved on the contralateral side in unilateral tumours. Postoperative head CT scan did not show any abnormality. Cosmetic result was correct in all patients.
ILLUSTRATIVE CASES
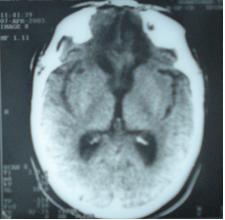
1st case
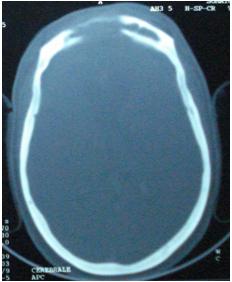
A 42-year-old woman was referred to the ophthalmologist for visual loss. Papilledema was present on both sides. A head CT scan was immediately performed (Fig. 6). It showed an enhancing tumour developed in the olfactosellar region on both sides. The patient had a history of severe headaches 8-year’s duration.
Neurologic examination showed anosmia, and the visual loss.
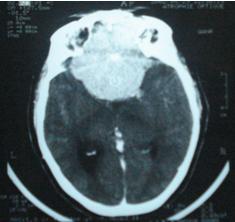
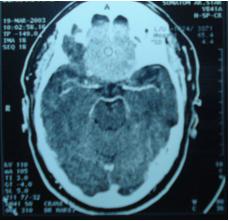
The trans-sinusal approach was used to remove the olfactosellar meningioma. Total tumour removal was possible without any brain retraction, in particular at the level of the optic canals. There was no blood loss. Postoperative course was uneventful. Control head CT scan showed no complications (Fig. 7). Visual acuity went from 0/10 to 6/10 in both eyes within 4 weeks. At 6-year follow-up, the result has been maintained.
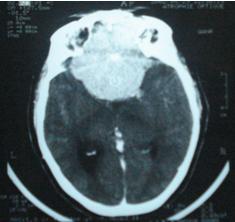
Figure 6
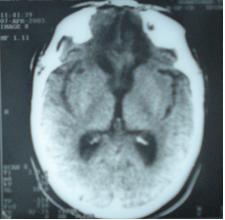
Figure 7
2nd case
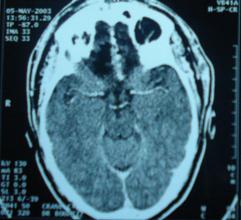
A 52-year-old man was referred to the ophthalmologist for visual loss. Papilledema was present on both sides. He reported one episode of epilepsy crisis two month before, a head CT scan was immediately performed (Fig. 8). It showed an enhancing tumour developed in the olfactosellar region on both sides.
Neurologic examination showed a visual loss.
The trans-sinusal approach was used to remove the olfactosellar meningioma. Total tumour removal was possible without any brain retraction, there was no blood loss. Postoperative course was uneventful. Control head CT scan showed no complications (Fig. 9). Visual acuity went from 2/10 to 6/10 within 7 weeks. At 5-year follow-up, the result has been maintained.
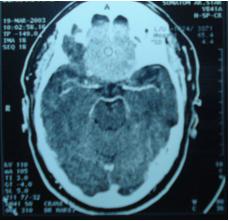
Figure 8
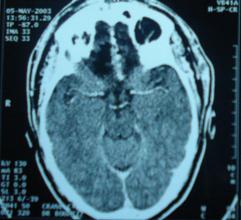
Figure 9
DISCUSSION
The trans-sinusal frontal approach has several advantages. Bone osteotomy and flap replacement are rapid. The time of intervention is reduced, with regard to large bifrontal approaches (17,24). Realization of the osteoplastic flap is facilitated by the width of the sinus; nevertheless, for small frontal sinus, real tangential cut including part of the external layer of the frontal vault gives the same exposure.
Lateral extensions of olfactory groove meningiomas are not the rule, making it unnecessary to enlarge laterally the flap to the frontal zygomatic processes. However, the flap has to exceed the limits of the sinus so as to obtain a harmonious arc of a circle. Cosmetically, postoperative result was very satisfactory, as the scalp incision was buried within the scalp. At the forehead level no osseous defect related to the burr holes is observed (8,19).
Real subfrontal access to the skull abolishes any need of brain retraction (10,18), especially because the frontal lobes fall toward the back because of gravity.
The bottom of the frontal sinus falls at the level of the base; it seems logical to use the most direct angle of attack according to the axis of the base. The absence of brain retraction contributes to the decrease in postoperative oedema, postoperative contusional haemorrhages or even brain ischemia favoured by the compression and/or the sacrifice of the frontal bridging veins (2). Also, to avoid brain damage, en bloc removal of the tumour is usually not recommended. Interruption of ethmoid arterial supply is done either by intracranial or by intraorbital approach (26). Safe devascularisation of the tumour by coagulating and resecting the basal dural attachment allows a dry operative field and facilitates the dissection of the posterior pole of the tumour. Tumour removal was total (grade I and II of Simpson) (23) in nine meningiomas: tree unilateral, and six bilateral olfactosellar.
Olfactory impairment was often an early symptom, but the diagnosis was rarely made before the tumour attained sufficient size to cause visual loss (20). Anosmia was not reversible because the olfactory nets were invaded and distended by the tumour and because they were removed during the operation. Preservation of the contralateral olfactory filaments permits conservation of some olfactory sense for tumours that have developed unilaterally, as we observed in tree cases.
The complications associated with the trans-sinusal frontal approach are twofold: infection and postoperative Cerebrospinal fluid fistulas. Infectious complications resulting from the penetration of the frontal sinus can be prevented by cranialization of the frontal sinus with total exenterating of the mucous membranes, and obturation of the frontonasal ducts isolating the cranial cavity from the paranasal sinuses; and watertight dural closure with a periosteum graft, reinforced by a free periosteum graft introduced on the dural defect.
The dural closure avoids Cerebrospinal fluid leaks. When the dura mater cannot be closed at the skull base, insertion of several periosteum fragments between the dural and the bone avoids the development of a fistula trajectory and permits spontaneous sealing of leaks. Furthermore, suppression of the deadspace by periosteum is factor acting against the development of infections.
Closure and reconstruction could not be achieved with a transciliary subfrontal craniotomy, (21) which does not justify taking large periosteum grafts.
The length of the scalp incision may be of concern. The bicoronal incision is long and may dispose to profuse bleeding. However, besides the excellent cosmetic result it allows, the bicoronal incision permits accurate fashioning of the bone flap without retracting soft tissues for exposure of the anterior wall of the sinus. To reduce operative time, blood loss, especially in case of hairline recession, deep forehead creases may be used to tailor the scalp incision (7).
CONCLUSIONS
The trans-sinusal frontal approach was used for removal of ten olfactory groove meningiomas, without any brain retraction or damage. The technique is easy to perform; it gives a direct subfrontal view of the base along its anterior floor, allows devascularisation of the tumour at the initial stages allows us to remove the tumour with a greater visibility. Reconstruction of the dural and the osseous skull base is permitted by the width of the working exposure. Cosmetic result is perfect.
The indications of the trans-sinusal frontal approach can be spread to all tumours of the anterior floor of the skull base.
REFERENCES
- AL MEFTY 0. Surgical technique for the juxta-sellar area. In: Surgery of the Cranial Base. Boston: Kluwer Academic Publishers; 1989:73-89
- AUQUE J, CIVIT TH. Les dangers du sacrifice du sinus longitudinal supérieur dans son tiers antérieur lors de la chirurgie des méningiomes olfactifs. Neurochirurgie 1996; 42(suppl 1):84-87
- BABU R, BARTON A, KASOFF SS. Resection of olfactory groove meningiomas: technical note revisited. Surg Neurol 1995; 44:567-572
- BEZIAT JL, PIERLUCA P. Les lesions traumatiques des confins cranio-faciaux. Démarche diagnostique et indications thérapeutiques. Lyon Chir 1984;80:333-336
- BONNAL J, SEDAN R, PAILLAS JE. Problèmes cliniques, évolutifs et thérapeutiques soulevés par les méningiomes envahissants de la base du crane. Neurochirurgie 1961;2:108-117
- BRET P, TREPSAT F, MASSINI B, et al. Exclusion d’une malformation arterio-veineuse de la gouttiere olfactive gauche par ligature endo-orbitaire des artères ethmoïdales. Neurochirurgie 1986;32:440-447
- CHENEY ML, GLIKLICH R, LI KK, et al. Midforehead incision. An approach to the frontal sinus and upper face. J Craniofac Surg 1995;6:408-411
- COPHIGNON J, GEORGE B, MARCHAC D, ROUX F. Voie transbasale élargie par mobilisation du bandeau fronto-orbitaire median. Neurochirurgie 1983;29:407-410
- CUSHING H, EISENHARDT L. The olfactory groove meningiomas with primary anosmia. In: Meningiomas: Their Classification, Regional Behavior, Life History and Surgical End Results. Springfield, IL: Charles C Thomas,1938:250-273
- DARROUZET V, SAN-GALLI F, PORTMANN D, et al. La voie trans-fronto-nasale. Evolution de la chirurgie par voie mixte des tumeurs ethmoïdales. Expérience de 12 cas. Rev Laryngol 1993;114:217-220
- DELFINI R, LANNETTI G, BELLI E, et al. Cranio-facial approaches for tumors involving the anterior half of the skull base. Acta Neurochir (Wien) 1993;124:53-60
- FOX D, KHURANA VG, SPETZLER RF. Olfactory Groove/Planum Sphenoidale Meningiomas. -Meningiomas- J.H Lee editior- Springer 2008:327-354
- HALLACQ P, MOREAU JJM, FISCHER G, BEZIAT JL. Voie trans-sinusienne frontale pour les méningiomes de la gouttière olfactive. Note technique. Neurochirurgie 1999;45:329-337
- HASSLER W, ZENTNER J. Pterional approach for surgical treatment of olfactory groove meningiomas. Neurosurgery 1989;25:942-947
- KEMPE LG. Olfactory groove meningioma. In: Operative Neurosurgery. Vol 1. New York: Springer-Verlag; 1968:104-108
- MAYFRANK L, GILSBACH JM. Interhemispheric approach for microsurgical removal of olfactory groove meningiomas. Br J Neurosurg 1996;10:541-545
- OJEMANN RG. Meningiomas of the basal parapituitary region: technical considerations. Clin Neurosurg 1980;233-262
- RAVEH J, LAEDRACH K, SPEISER M, et al. The subcranial approach for fronto-orbital and anteroposterior skull-base tumors. Arch Otolaryngol Head Neck Surg 1993;119:385-393
- ROUX FX, DEVAUX B, NATAF F, et al. Tumeurs malignes de la région ethmoïdale. Techniques neurochirurgicales. Neurochirurgie 1997;43:92-99
- SAMII M, DRAF W. Surgery of the Skull Base. An Interdisciplinary Approach. Berlin: Springer-Verlag; 1989
- SANCHEZ-VASQUEZ MA, BARRERA-CALATAYUD P, MEIJA-VILLELA M, et al. Transciliary subfrontal craniotomy for anterior skull base lesions. Technical note. J Neurosurg 1999;91: 892-896
- SEN C, SEKHAR LN. An extended subfrontal approach to the skull base. In: Rengachary SS, Wilkins RH, eds. Neurosurgical Operative Atlas. Vol 2. Baltimore: Williams & Wilkins, 1992:97-106
- SIMPSON D. The recurrence of intracranial meningiomas. J Neurol Neurosurg Psychiatry 1957;20:22-39
- SNYDERMAN CH, COSTANTINO PD, SEKHAR LN. Anterior approaches to the cranial base. In: Apuzzo MLJ, ed. Brain Surgery: Complication Avoidance and Management. New York: Churchill Livingstone, 1993:2265-2281
- VILLETTE L, LEPOUTRE F, LESOIN F, et al. Traitement des brèches osteo-durales de l’étage antérieur de la base du crane par voie trans-1esionnelle. A propos de 25 cas opérés en double équipe neurochirurgicale et maxillo-faciale. Rev Stomatol Chir Maxillofac 1989;90:73-78
- YASARGIL MG. Microneurosurgery of CNS Tumors. Vol IVB. New York: Thieme, 1996:140-141