
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
CLINICAL STUDIES / ETUDES CLINIQUES
OPHTHALMIC MANIFESTATIONS IN PATIENTS WITH INTRACRANIAL TUMOURS
MANIFESTATIONS OPHTALMIQUES LORS DE TUMEURS INTRACRÂNIENNES
E-Mail Contact - ONAKPOYA Oluwatoyin Helen :
ufuoma@oauife.edu.ng
ABSTRACT Background Method Results Conclusion Keywords: Manifestation, Intracranial Tumours, Blindness, Ophthalmic, Nigeria RESUME Introduction Méthode Résultat Conclusion INTRODUCTION Primary brain tumours constitute a major reason for seeking neurological consultations worldwide1-3. The location and type of tumour influences the clinical Intracranial tumors affect almost any tissue in the brain leading to different spectrum of brain tumours. In a study of patients with brain tumours in New York, Snyder at al reported malignant astrocytoma as the most frequent tumor 14. Pisarev et al reported gliomas as the commonest brain tumor in the Volgograd region where it represented 51.9% of all intracranial tumors13; while in Iran and Thailand, meningiomas were the commonest representing 26% and 45% of all brain tumors respectively 1,10. Patients from developing countries tend to present late with larger masses and this may affect the prevalence and pattern of ophthalmic manifestations at presentation. The purpose of this paper is to document the ophthalmic manifestations of METHODOLOGY Setting The neurosurgical unit of the Obafemi Awolowo University Teaching Hospital, (OAUTHC) Ile-Ife is a referral unit for patients with neurosurgery diseases. The unit comanages Study design A 5-year retrospective descriptive review of in-patients managed for intracranial tumors from January 2003 to December 2007 was conducted. Patients with intracranial space occupying inflammatory or vascular lesions were excluded. Preoperative diagnosis was made based on the clinical presentation and radiological investigations. Histological diagnosis was made post operatively. Presenting visual acuity was recorded using the Snellen’s chart or illiterate E chart; this was further classified using the World Health Organizations classification into normal, visual impairment, severe visual impairment or Out of a total of 94 patients managed for intracranial tumours, 88 with complete records Socio-demographic distribution There were 53 [60.2%] males and 35 [39.8%] females with a male to female ratio of 1.5:1. The mean age was 36.2±20.1years; 43.2% were within the 36-55 years age group while 19.3% belonged to the peadiatric age group (≤ 15 years). Male preponderance was noted across all age groups except in children aged five years and below in whom a male to female ratio of 1:1.8 was recorded. Figure I shows the age and sex distribution of patients managed for brain tumours. Most of the patients 36 (40.9%) resided within the state of location of the neurosurgical facility (Osun State) or 41 (46.6%) within the same zone (southwest). [Table I] Pattern of referral Referral was mainly from private hospitals 36(40.9%) while referrals from public hospitals were largely from the general outpatient department and emergency rooms of within the same institution 24(27.4%). [Table I] Patients had sought previous neurologist 9(10.2%), ophthalmologist 14 (15.9%) and paediatrician 10 (10.4%) consultation before presentation. Duration of symptoms prior to neurosurgical attention ranged from 1 to 484 weeks with a mean of 63.1±107.8 weeks. (52.7%) presented for neurosurgical care more than twelve weeks from the onset of symptoms related to the intracranial tumour. [Table I] Ocular status 59 (67%) had eye complains at presentation while 29(33%) made no complains referable to the eyes. Poor vision (46.6%) and double vision (12.5%) were the commonest ocular symptoms. Ocular findings were normal in 45 (51.3%) patients while optic atrophy was the commonest ocular sign (23.9%). [Table III] Ocular nerve palsy was present in 16(18.2%) out of which 9(56.3%) involved the sixth nerve, 5(31.3%) the third nerve and 2(12.4%) were multiple nerve palsies. Unilateral blindness was present in 3(3.4%) and unilateral visual impairment in 6(6.8%); bilateral blindness was present at presentation in 46 (52%) [Figure II]. Patients with visual impairment and blindness were more likely to have eye complains at presentation (88.3%) compared with 50% amongst patients with normal vision using the WHO classification (P=0.003). Spectrum of intracranial tumours Radiological investigations conducted were cranial CT scan in 84 [95.5%], MRI in 1[1.1%], and skull X-rays in 3[3.4%]. Supra-tentorial tumours were more common 77 [87.5%]. Meningiomas(36.4%), Craniopharyngioma(13.6%) and gliomas(9.1%) were the commonest brain tumours encountered (Table III). DISCUSSION The mean age of 36.2 years of patients with brain tumour recorded in this study is younger than the 42.8 years and 50.76 years reported in New York and Romania respectively; it however compares favourably with the 33.9 and 37 years reported from Iran and Kenya1,7,14,15. This is obviously a disease affecting mainly young adults and middle aged- the economically and physically active subset in any society. Children constituted 19.3% of the patients with brain tumours in this study similar to the 20.1% reported by Mehrazin et al1; brain tumors are the most common solid tumour entity in childhood .13 The male preponderance may be related to hospital biased design as male utilization of health care facility in sub-saharan African is generally reported to be higher than females. The reason for the female predominance in the pediatric age group may require further epidemiological studies as the reason for this is not known. The signs and symptoms of intracranial tumours are usually none specific and may be slowly evolving; this may be responsible for the previous consultations before final referral to the neurosurgical unit. Moreover, Cranial Tomography scan is not commonly available or affordable by many patients in our environment hence the delay in appropriate diagnosis and referral. The location, size and involvement of the visual pathway and ocular nerves determine to a large extent the degree of involvement of the eyes in brain tumours. In this study, about two-thirds (67%) of patients with intracranial tumours had ophthalmic symptoms at presentation. This is similar to the slightly higher value of 72% reported by Marco et al in Kenya where poor referral network and poverty leading to delayed presentation for neurosurgical care were implicated 15. Anderson et al reported a much lower rate of 30% among patients with meningiomas 16. Poor vision as the most common ophthalmic symptom in this series is similar to previous reports; however, while this symptom was reported in 52% of our patients, much higher frequency of 88.6% and 86% were reported 10,11. The difference may be related to the difference in the pattern of brain tumours studied; meningiomas and parasellar tumors (pituitary adenoma and craniopharyngioma) constituted 84.6% of all brain tumours studied as compared to 55.6% in the present study. The anatomical location of these tumours predisposes them to more frequent mass-compression effect on the optic nerve, optic chiasma and optic tract; hence more frequent involvement of the vision. Ocular cranial nerve involvement is responsible for double vision which was found in 12.5% of patients studied; this is within range although slightly higher than the 10% reported in Kenya 15. The frequency of double vision as a symptom may not represent all the cases of ocular deviations and cranial nerve involvement as patients with severe visual impairment and blindness may not experience double vision. Moreover, young children are not articulate enough to complain of double vision ref. Although 18.2% of the patients with intracranial tumours on examination had ocular deviation due to involvement of ocular cranial nerves, only 12.5% complained of double vision. Ocular nerves can be affected by intracranial tumour due to their mass effect or infiltration by the tumour. Although, the third cranial nerve is the commonest palsy accompanying pituitary tumours, the sixth cranial nerve is frequently affected by the resultant raised intracranial pressure from intracranial tumours; this is a possible explanation for its commoner occurrence compared to the third and fourth nerves in this study. Over half of our patients were blind at presentation for neurosurgical care; this compares favourable with the 59% of blindness recorded in Thailand amongst patients with intracranial tumours 10. In a similar study in New York, total percentage of visual deficit reported was 19.8%. The higher percentage of blindness in developing countries as opposed to developed country may be related to late presentation for neurosurgical care with larger tumour and in advanced disease in the former. During the period of study, about 59.1% of the patients were referred from outside the state of location of the neurosurgical centre. In a developing country setting like ours, the adverse effects of poor socio-economic status on health care viz-a- viz utilization and late presentation comes to play more when health care facility is located far from the patient. Optic nerve head changes, that is, optic atrophy and papilloedema were present in 44.4% patients with brain tumor in this study. The importance of ophthalmoscopy as part of required neurological examination for early diagnosis of intracranial space occupying lesions is further justified. Papilloedema was reported in 27.7% and 46.8% of patients with intracranial tumours in New York and Romania respectively 7,14. Anteriorly located intracranial tumours have a higher propensity to compress the optic pathway and hence present earlier with optic nerve compressive changes seen at ophthalmoscopic examinations 15. Visual field defects were the commonest ophthalmic sign and were seen in 80.5% of patients with intracranial tumour 12 while Marco et al also reported non-specific field pattern (34%) as the most common visual field changes in patients with intracranial tumours15. In the present study, this sign was not objectively assessed as visual field analyzer was not available in the study centre and its immediate environs. In conclusion, ophthalmic clinical features form a major part of presentation of patients with intracranial tumours. Complete neuro-ophthalmic evaluation seeking for the signs and symptoms enumerated is essential for diagnosis. Table I: Characteristic of patients with brain tumours
Table II: Eye symptoms and signs in patients with intracranial tumours
# – multiple signs were present in some patients Table III: Spectrum of intracranial tumours
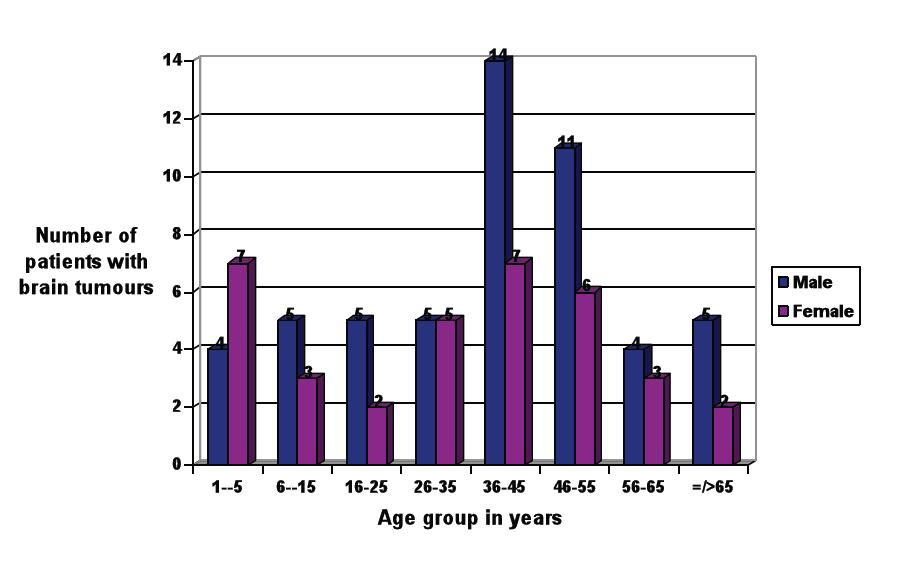 Figure 1 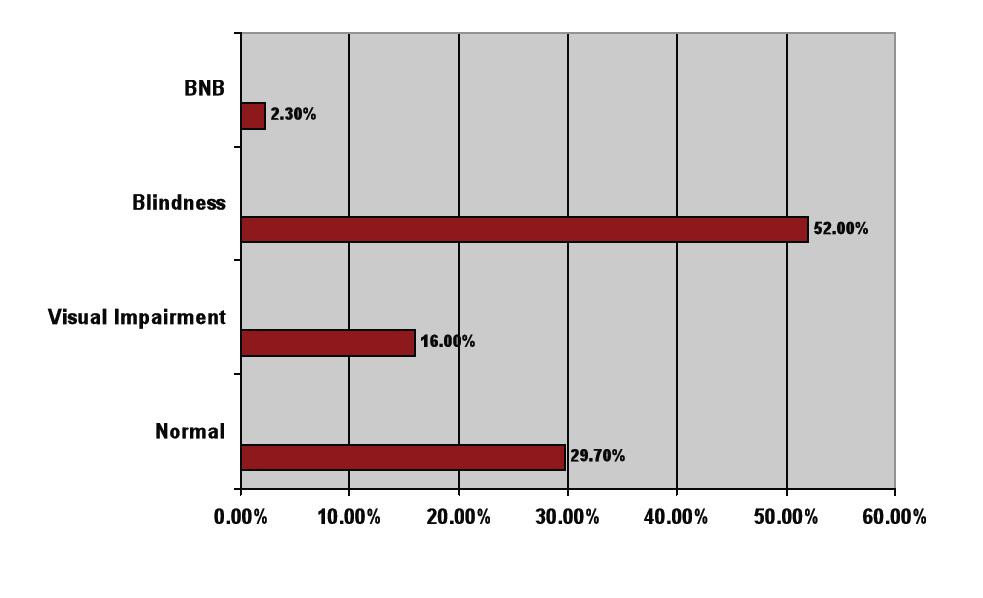 Figure 2 REFERENCES
|
© 2002-2018 African Journal of Neurological Sciences.
All rights reserved. Terms of use.
Tous droits réservés. Termes d'Utilisation.
ISSN: 1992-2647