
|
|
|
CASE REPORT / CAS CLINIQUE
NOCARDIA BRAIN ABSCESS – CASE REPORT AND LITERATURE REVIEW
ABCES CEREBRAL A NOCARDIA - A PROPOS D'UN CAS ET REVUE DE LA LITTERATURE
TALI A.
2
E-Mail Contact - EL HYMER Wafae :
wafaeelhymer@hotmail.com
ABSTRACT Background and purpose Methods Case report Conclusion Key words: Brain abscess, Nocardia abscess, surgery, Morocco RESUME Introduction Méthodes Cas clinique Conclusion Mots clés : abcès cérébral, abcès à Nocardia, chirurgie, Maroc INTRODUCTION Nocardiosis is a rare opportunistic infection caused by Nocardia gram-positive aerobic filamentous bacilli, presenting as pulmonary disease in more than 70 % of patients [2]. Dissemination of the disease may be manifest as brain abscess and soft tissue infections [1]. Brain abscess is the more common clinical manifestation of central nervous system infection. Cerebellar and spinal locations are uncommon [5]. Mortality is high especially in immunocompromised hosts [8]. Paucity of clinical and laboratory signs of infection and insidious manifestations makes diagnosis and management difficult [1, 5]. CASE REPORT A 56 year old man was admitted to our institution with a 2 week history of headache and vomiting, dry non productive cough and low grade fever. He had a three day history of gait disturbance. A craniotomy was done in the left posterior cerebellar fossa, and thick green pus was aspirated. Further definitive identification and susceptibility testing identified N. asteroids with susceptibility to timethoprim-sulfamethoxazole, amoxicilline-clavulinique acid, ciprofloxacine, amikacine, imipenam, and resistant to ampicilline, erithromycine, cefotaxime, chloramphenicol. DISCUSSION In order of frequency, the most common pathogenic Nocardia species are N. asteroids, N. brasiliensis and N. Otitidiscaviarum. Others species of Nocaria sush as Nocaria farcinica have rarely been isolated from clinical specimens. Among the etiologic factors of systemic or cerebral Nocardiosis are malignancies, immunodeficiency states, iatrogenic immunosuppression following organ transplantation, diabetes mellitus, renal disease, collagen vascular diseases, alcoholism, tuberculosis, preceding operation, chronic lung disease, trauma or abnormal phagocytic activity [1, 2, 6]. Although CNS nocardiosis is usually a consequence of pulmonary infection no other focus of infection could be found in this patient. Pulmonary sarcoidosis treated by a long term steroids, was probably the predisposing cause in our patient; namely chronic lung disease and immunosuppression. Most of the patients have predisposing factors, but in 15% N.asteroid infection occurs without underlying illness [6]. The portals entry of N.Species is the respiratory tract, surgical or traumatic skin wounds. Nocardial organisms have tendency to disseminate hematogenously from the primary site of infection, usually the lungs, brain, kidney, joints, bones and eyes are frequently secondary sites of infection. Although hematogenous dissemination to the CNS is reported in 20-45% of all nocardial infections [2],CNS nocardiosis is a rare clinical entity, where diagnostic delay often leads to a fatal outcome [3, 8]. The infection can spread hematogenously and progress to a disseminated disease that is defined by the presence of two or more foci of nocardiosis.. An increasing number of cases are being reported in immunocompetent individuals without predisposing factors. Cerebral nocardiosis is an uncommon clinical entity, representing only 2% of all cerebral abscesses [5, 7]. As our case the cerebellar and spinal locations are uncommon [5]. Most common presentation is with evidence of progressively expanding intracerebral mass lesion which can be multiple or single [9]. Nocardial brain abscesses are often misdiagnosed as malignant brain tumours and a definitive diagnosis may not be possible without detecting bacteria from the lesion. Infection of the brain by nocardia is often insidious in onset, difficult to diagnose and treat successfully [8]. It was also associated with a high mortality rate, which has been considerably reduced with advent of the CT scan [4]. There was no difference in the mortality rates of immunocompromised and non immunocompromised patients treated before CT was available; since the advent of CT, however, the mortality rate has been significantly worse in immunocompromised patients ( 55 % VS 20 %, P (0.005) [7]. Nocardial brain abscesses are frequently solitary (54 %). The mortality rate in patients with multiple abcesses is twice of that among patients with solitary abscesses (66% vs.33 %). The mortality rate also rises if the diagnostic procedures are delayed or the detected microorganism is highly resistant to the current antibiotics [6]. Stereotactic aspiration or open craniotomy for radical excision is indicated for patients who worsen neurologically or show enlargement of the intracerebral lesion. In fact the mortality rate among patients undergoing craniotomy (24%) is less than half of that among patients undergoing aspiration or drainage alone (50%), and is also lower than that among patients undergoing nonoperative therapy (30%) [6]. Treatment consists of surgical management which includes abscess drainage and institution of appropriate antimicrobials after culture confirmation [8]. Cotrimoxazole remains the antibiotic of choice and duration of treatment varies from six weeks to one year because of the high relapse rates after apparent cure, and in the immunodeficiency states [4]. Amikacin, imepenem, minocycline, ciprofloxacin and third generation cephalosporines are second line agents. Although resistance is not widespread, National Committee for Clinical Laboratory Standards NCCLS (now clinical and laboratory standard institute CLSI) recommends drug sensitivity for refractory cases [8]. Carbapenems, aminoglycosides, and linezolid have been found to very effective in many clinical situations [4, 5, 8]. CONCLUSION Nocardiosis is a clinical entity which should be kept in the differential diagnosis of any brain abscess, even in apparently immunocompetent patients. Once diagnosed, empirically based drug treatment and surgical intervention must be applied for achieving significant improvement. 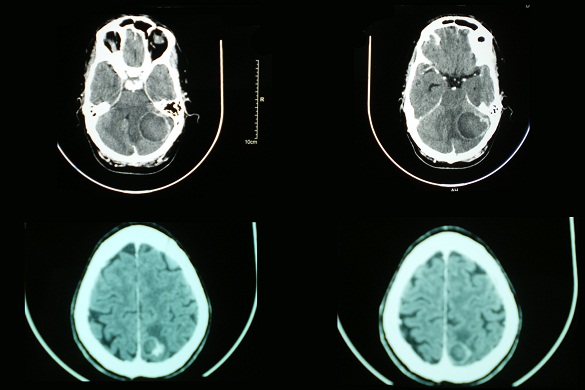 Figure 1 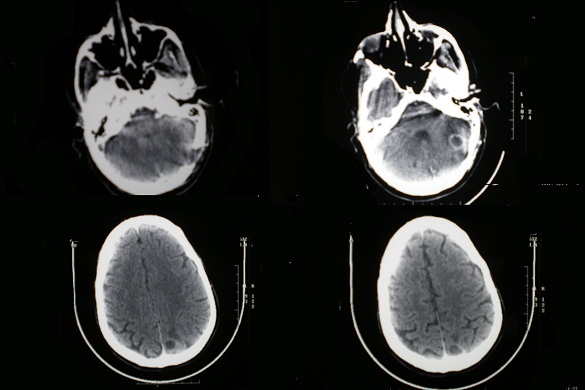 Figure 2 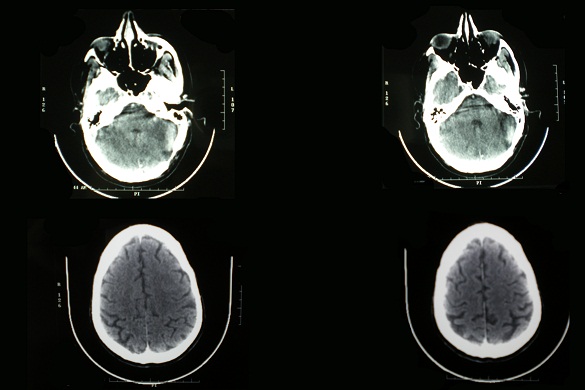 Figure 3 REFERENCES
|
© 2002-2018 African Journal of Neurological Sciences.
All rights reserved. Terms of use.
Tous droits réservés. Termes d'Utilisation.
ISSN: 1992-2647