CLINICAL STUDIES / ETUDES CLINIQUES
CRYPTOCOCCAL MENINGITIS ASSOCIATED HIV INFECTION IN THE DONKA NATIONAL HOSPITAL IN CONAKRY (GUINEA)
MENINGITE A CRYPTOCOQUES AU COURS DE L'INFECTION PAR LE VIH A L'HOPITAL NATIONAL DONKA DE CONAKRY (GUINEE)
- Service de maladies infectieuses et tropicales de l’hôpital national Donka
- Laboratoire de parasitologie- mycologie de l’hôpital national Donka
- Service de Pédiatrie de l’hôpital national Donka
- Service de médecine interne de l’hôpital national Donka
- Service de neurologie de l’hôpital national Ignace Deen
- Institute of Tropical Medicine (NEKKEN); Nagasaki University, Japan
E-Mail Contact - CHERIF Mahamoud Sama :
ABSTRACT
Background
Cryptococcal meningitis (CM) is an infection of the brain parenchyma and subarachnoid space by the encapsulated saprophyte yeast organisms such as Cryptococcus neoformans. Over the last twenty years, HIV has created a large and severely immune compromisized population in whom C. neoformans is a dangerous opportunistic infection. In Guinea, the prevalence of CM is unknown. We hypothesized that the occurrence of CM correlates with AIDS/ HIV prevalence.
Method
This retrospective observational study was carried out at the national Hospital of Conakry (Guinea) between 2001 and 2002. We describe here the epidemiological and clinical and biological characteristics of CM disease in our national hospital.
Results
Our data show that, 28.6 % of HIV patients with neurological symptoms had Cryptococcus neoformans in their CSF by using Indian ink staining. The median age was 36±3 years and sex ratio (M/F) was 1.8. The major complaints were fever and cephalgia, giddiness while the major complications were altered consciousness and hemiplegia. CSF was clear with low level of glucose and higher level of albumin. The means of lymphocytes in CSF was 8±2/mm3.
Conclusion
This data therefore becomes relevant in not only focusing of neurological symptoms associated with HIV to be toxoplasmosis but the possibility of C neoformans in these patients; particularly when they present symptoms such as headaches, giddiness and sniff neck etc. This can easily be carried out with Indian ink staining technique.
Keyword: AIDS- Cryptococcal Meningitis – Guinea – HIV
RESUME
Cryptococcose méningée (CM) est une infection du parenchyme cérébral et de l’espace sous arachnoïdien par Cryptococcus neoformans. Durant les vingt dernières années, la CM a connue une flambée grâce à l`avènement du VIH/SIDA, et devenant ainsi, une des infections opportunistes dangereuse chez les immunodéprimés. En Guinée, sa fréquence n’est pas encore connue et elle pourrait être en corrélation avec la séroprévalence du VIH.
Méthode
Cette étude rétrospective a été effectuée à l’Hôpital National de Conakry, portant sur les patients admis entre 2001 et 2002. L’objectif était de décrire les caractéristiques épidémiologiques, cliniques et biologiques de la CM.
Résultats
L’examen direct du liquide céphalorachidien à l’encre de Chine avait montré que, 28.6 % de patients infectés par le VIH admis avec des symptômes neurologiques, avait le C neoformans. L’âge médian était 36±3 ans et le sex ratio (M/F) était 1.8. Les plaintes majeures étaient la fièvre et céphalées et vertiges tandis que les complications majeures étaient le trouble de la conscience (coma) et l’hémiplégie. La majorité des patients avaient le LCR clair avec une basse glycorhachie, une hyperalbuminorhachie et le nombre moyen de lymphocytes dans le LCR était 8±2/mm3.
Conclusion
A la lumière de ces résultats, il apparait utile de rechercher en plus de la toxoplasmose, la présence du C neoformans chez tout patient infecté par le VIH et particulièrement présentant des symptômes neurologiques comme céphalées, vertiges, raideur de la nuque etc. Cette recherche peut être réalisée par la coloration du LCR à l’encre de chine.
Mots clés: Cryptococcose méningée – Cryptococcus neoformans – Guinée – SIDA- VIH
INTRODUCTION
Cryptococcal meningitis (CM) is a common opportunistic infection in acquired immune deficiency syndrome (AIDS) patients, particularly in Southeast Asia and Africa[6,10,11,15]. It is AIDS defining illness in patients with late-stage Human Immunodeficiency Virus (HIV) infection, particularly in Southeast Asia and Southern and East Africa.[16,17,26]. Over the last 20 years, HIV infection pandemic has created a large and severely immune compromized population, with cryptococcal meningitis also occurring in patients with immunosupression. In parts of sub-Saharan Africa with the highest HIV prevalence, cryptococcal meningitis is now the leading cause of community-acquired meningitis, ahead of Streptococcus pneumoniae and Neisseria meningitidis[ 4,12,14,26]. Frequency of CM associated HIV infections varies from 2 to 35% according to the areas [9]. In the USA, about 7% [4,9]has been reported. In France, 88% of CM cases was associated with HIV infection [8,13]. While in Africa the range of frequency varies between 13 and 35% [5,8,11], 5.4% in Tunisia [18,19], 3,25% in Burkina Faso [21] and 5,4% in Ivory Coast [3]. In Uganda, the incidence of cryptococcal disease in patients with CD4 counts <200 cells/ml was estimated at 10.3 cases per 100 person years of follow-up [9]. In Thailand, cryptococcosis accounted for 19% of AIDS-defining illnesses between 1994 and 1998[19]. It seems most likely the high incidence of cryptococcal meningitis in parts of Africa and Asia reflects differences in exposure rather than host susceptibility or cryptococcal strain virulence, although no studies have addressed this issue [5,6,8,20]. Meningitis is the most frequent manifestation of cryptococcosis. Infection of the subarachnoid space is accompanied by involvement of the brain parenchyma, and therefore the term meningo-encephalitis may be more appropriate [11, 17,26].
Mortality from HIV associated cryptococcal meningitis remains high (10-30%), even in developed countries, because of the inadequacy of current antifungal drugs. In cohorts of HIV-infected patients from sub-Saharan Africa, cryptococcal meningitis has accounted for 13-44% of all deaths[26].
In Guinea, HIV prevalence increase from 1.7% in 1995, to 2.8% in 2002 [23] and the burden of CM is not yet clearly documented. We hypothesized that the frequency of CM associated HIV infection is correlated to HIV prevalence. In this study we describe the epidemiological characteristic, clinical presentation and CSF findings of CM in the national hospital of Conakry.
MATERIALS AND METHODS
This retrospective observational study was carried out at the national Hospital of Conakry (Guinea) between 2001 and 2002. Seventy (70) HIV-infected patients were enrolled in the study. These patients underwent lumbar puncture as part of the routine work-up for a suspected neurological disease. The specimens of cerebrospinal fluid (CSF) from adult Human Immunodeficiency Virus-positive were taken for further mycological study.
Cryptococcal meningitis was diagnosed based on one of the following: (i) a positive India ink CSF result only, (ii) a specific cryptococcal CSF antigen test, (iii) or a positive CSF culture for Cryptococcus neoformans, has not realized.
Patients’ demographic data and clinical symptoms were collated from interviews of the patients. Physical findings, CSF examination (parameters such as glucose, albumin) outcome were analyzed. Informed consent was obtained from the patients enrolled in the study after ethical approval by the national ethics committee
Statistical analysis: Statistical analysis was done using the statistical software ‘EPI info version 0.6’ (CDC Atlanta, USA). Descriptive analysis consisted of mean with standard deviation and range for various parameters. Frequency of various clinical and laboratory findings are expressed as percentage.
RESULTS
Seventy (70) complete files from HIV patient hospitalized in Tropical and infectious diseases service of Donka national hospital, between 2001 and 2002 were recorded. Out of these seventy HIV patients, 28.6% had C. neoformans highlighted in their CSF after lumbar puncture using Indian ink staining (figure 1). Patients were categorized in age groups with a constant interval of 10. The majority of patients with CM associated HIV infection were in the group of 25-34 and 35-44 years of 40 and 45% respectively. Almost 15% of patients were > 45 years (Table 1). The mean age was 36±3 years. The majority of patient was in the range from 25 and 44 years. Distribution of patients according to sex show that the majority were male (figure 2).
According to their occupation, we found that one -third of the entire patients were drivers or apprentice drivers (30%), housewives and farmers (20%), workmen (20%), civil servants and others (15%) (Figure 3).
Analysis of residence of the patients showed that majority were from the urban areas (townsmen) (75%) and 25% from suburban areas (figure 4). The low number from suburban regions maybe due to their poor accessibility to the health care facility such as those in Donka National Hospital. However, information on other risk factors such as place of work, contact with pigeon, malnutrition, smoking, hepatitis C, etc were not collected.
Clinical feature of Cryptococcal meningitis
Cryptococcal meningitis presents a variety of symptoms and clinical signs; in this study we used the most frequent ones observed among all patients. The clinical presentation was almost the same of all the patients with few exceptions. Fever (100%), headache (56%) giddiness (65%), stiff neck (20%), tremor of the ends (20%), insomnia (50%), coma stage II (25%), Ptosis for both or one eyelid (20%) , deafness (20%) and hemiplegia by brain focal lesion (20%) (Table 2) are examples of the clinical presentations.
Cerebrospinal Fluid (CSF) characteristics
Visual observation of the collected CSF after the lumbar puncture was clear for most of the patients (95%) and in the other case the CSF was contaminated with blood. The red blood cells in the CSF was due to the procedural error during the lumbar puncture.
The biochemical analysis showed that 56% of patients had a lower glucose average CSF of glucorrhchia and, glucorrhchia average was about 0.40±0.1 g/l.
Our data showed that 75% of patients had higher protein average in CSF. The proteinorrhchia average was about (113±5 mg / dl).
The lymphocyte count in CSF showed that 70% of patients had high number of lymphocytes, and the mean of lymphocytes was 8±2/mm3.
DISCUSSION
Cryptococcosis is a major opportunistic mycosis which has meningitis as its most frequent clinical presentation and can be fatal in the absence of antifungal therapy [1]. Cryptococcal meningitis is the most frequent nervous system disease after cerebral toxoplasmosis in HIV infection [15]. In this study the proportion of patients with CM using Indian ink staining was about 28.6% (Fig 1), which is consistent with the range observed in African countries between 10 to 35% [16]. The high frequency of CM in this study was due to the fact we included HIV patients with neurological symptoms. As a consequence of the increase in HIV-associated cryptococcosis, there has been a shift in the epidemiology of meningitis with cryptococcal meningitis now the leading cause of community-acquired meningitis, ahead of tuberculosis and bacterial meningitis which accounts for 20-45% of laboratory-confirmed cases in Southern Africa[ 15]. In Southeast Asia and Africa, cryptococcosis appears to be relatively more common as an AIDS-related infection than it ever was in Europe or North America [11]. In Burkina Faso, according to Millogo et al., real prevalence of this disease remains to be determined and could be still under estimated [21].
Mean age of the patients with CM associated HIV was 36±3 years. Our data showed that the highest frequencies were from ages 35 to 44 (45%) and 25 to 34 years (40%), (Table I). This can be explained by the fact that these ranges of age were affected by HIV infection [23], which constitutes the main risk factor of CM because of their active sexual life [5;8;11;16 and17]. In Tunisia, Kalthoum et al., reported in their study that the mean age was about 33 years [18]. In Senegal, Sow et al., also reported an average of 37 years with the range between 21 to 56 years [2], while in France, Dromer F et al., [8] found an age group between 26 and 35 years old for HIV-positive patients and more than 46 years old for HIV-negative patients [8]. Most of the indian patients were in the age group 25-49 years and males dominated the study group [24]. In this study, the sex distribution showed that the male dominated in the group (13 men and 7 women) giving a sex ratio (M/F) of 1.8 (figure 2). The male domination has been reported in others studies [20;21]. This could imply that male are becoming more active sexually than their female counter parts. In this study, professional distribution of the CM patients showed that the drivers were more affected than other professions (figure 3). Previously it was shown that drivers, prostitutes, and soldiers were high risk professions for HIV infection and also at risk for CM. Our results confirm an early report according to HIV prevalence study in 2002 [23]. It appears the nature of their profession makes them have high contact with sexual prostitute. We, however, did not find the other occupations with high risk for HIV infection like the girls prostitutes. This study revealed, HIV infection was a risk factor for Cryptococcal Meningitis. We did not have information about other risk factors like the use of antitumor drugs, malnutrition, home and work place with pigeon or immunosuppressive treatment.
Meningeal inflammation produced by Cryptococcus neoformans, an encapsulated yeast that tends to infect individuals with Acquired Immunodeficiency Syndrome (AIDS) and other immunocompromised states [6,10,11,15]. The organism enters the body through the respiratory tract, but symptomatic infections are usually limited to the lungs and nervous system [6,10,11,15]. Infection of the subarachnoid space is accompanied by involvement of the brain parenchyma, and therefore the term meningoencephalitis may be more appropriate [26]. Clinically, the course is sub-acute and may feature headache; nausea; photophobia; focal neurologic deficits; seizures; cranial neuropathies; and hydrocephalus [23]. In this study, all the patients manifested fever as complaint (20/20), headache (13/20) and giddiness (13/20) over several weeks. (Table 2)
Our results agree with the previously reported clinical features. In Senegal, Sow et al. [24], reported headache and vomiting among all patients and stiff neck among 4 patients out of 7 cases with coma. The major complication was hemiplegia [24]. Contrary to Anna’s results [1], Millogo et al. [21], reported that hemiplegia, stiff neck and sensory loss were not significant.
Cryptococcal meningitis is a serious infection of the brain and spinal cord that can occur in people living with HIV. Many authors reported that the presence of CN in the brain and the CSF maybe responsible for the changes in CSF composition such as glucose, proteins and white cell number [6,10,11,15,17]. CSF protein was elevated for 75% of patients in this study; the protein average was about 1.13±0.5 g/l. Fifty-six percent (56%) had low mean CSF glucose of 0.40±0.1 g/L. In India, Susheel et al., reported low glucorrhachia of 75% [25]. An increase of white blood cells indicates infection (include encephalitis), inflammation, or bleeding into the cerebrospinal fluid. Our data showed that 70% had higher lymphocyte count. Lymphocyte average was about 8±2cells /micro liter.
Untreated cryptococcal meningitis is uniformly fatal, although survival can range from years in those without apparent immunocompromise to only a few weeks in HIV-associated infection [26]. In our study, the majority of patients were not receiving antifungical treatment and antiretroviral treatment, because they are very expensive for the majority of patients. Furthermore, drug acquisition costs are high for antifungal therapies as they are administered for 6-12 months. The Anti retroviral Treatment (ART) was not accessible to everybody because it was not free at the time study was done. This low accessibility to ART and antifungical drugs was reported by many authors [3, 18,24). This study was relevant in that until now only a few case reports have been documented concerning the knowledge of this disease in Guinean patients. Thus to combat and minimize the scourge of the disease, ART need to be made accessible to the majority of patients. National hospitals and pharmacies should be supplied with them (ART) and the antifungical drugs too.
In conclusion, this data therefore become relevant in not only focusing neurological symptoms associated with HIV to be due to toxoplasmosis but the possibility of C neoformans in these patients; particularly when they present symptoms such as headaches, giddiness and sniff neck etc. This can easily be carried out with Indian ink staining technique.
| Acknowledgements: |
| We also appreciated the assistance of Doctors CAMARA Lansana Mady; CAMARA Sine, Benourou DIABATE, Alpha KONE, Moumie BARRY and CONDE Namoudou; Prof CISSE Mohamed, and Mr. Boamah Daniel, for criticisms and suggestions to improve the contents of this work. |
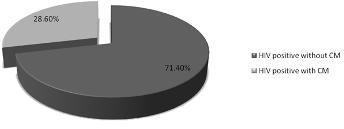
Figure 1
Table 1: Distribution of patient according to age.
| Age group(years) |
Frequency |
% |
| 25-34 |
8 |
40 |
| 35-44 |
9 |
45 |
| 45-54 |
2 |
10 |
| 55 -64 |
1 |
5 |
| Total |
20 |
100 |
This data represents 28.6% (20) of the seventy (70) HIV positive patients with neurological symptoms and positivity for C neoformans analysis in their cerebro spinal fluid (CSF). C neoformans analysis was done via Indian ink staining.
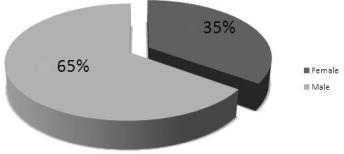
Figure 2
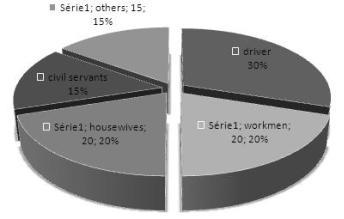
Figure 3
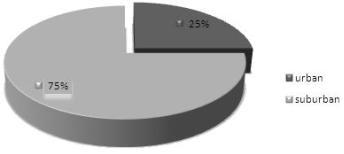
Figure 4
Table 2: Distribution according to symptoms evoked and signs observed
| Symptoms and Signs |
Frequency/20* |
Percentage (%) |
| Fever |
20 |
100 |
| Céphalgia or headache |
13 |
65 |
| Giddiness |
13 |
65 |
| Insomnia |
10 |
50 |
| Hypoesthesia |
9 |
45 |
| coma stage II |
5 |
25 |
| Stiff neck |
4 |
20 |
| Tremors of the ends |
4 |
20 |
| Amnesia |
4 |
20 |
| Ptosis of eyelid |
4 |
20 |
| Deafness |
4 |
20 |
| Hemiplegia |
1 |
5 |
*Total of the twenty (20) patients (out of the total seventy (70) HIV cases) who were positive for C. neoformans in their cerebrospinal fluid (CSF). Cryptococcal meningitis presents a variety of symptoms and clinical signs; we collected in this study the ones frequently evoked or observed among patients. Multiple signs were present in some patients.
REFERENCES
- ADAMS RD, VICTOR MR, ALLAN H, DAROFF RB. Principles of Neurology, 7 th ed. New York 1997; 721-722.
- ANNA LL, JOSIANE F, ALEXANDRE MF, JULIANO TB, MARIA CB, MARILENE HV. Epidemiological Profile of Cryptococcal Meningitis Patients in Rio Grande do Sul. Brazil Mycopathologia. 2008;166:71-75.
- BISSANGNENE E, SYLLA KDF, COULIBALY M, AOUSSI E, KACOU A, MOREAU J, ODEHOURI K, KADIO A. Méningite à cryptocoques chez les malades atteints de SIDA en Côte d’Ivoire. Problèmes diagnostiques, thérapeutiques et pronostiques à propos de 13 observations. Med Afr Nre. 36.1989;36; 849-854.
- BOGAERTS J, ROUVROY D, TAELMAN H, KAGAMÉ A, AZIZ AM, SWUINE D, VERHAEGEN J. Aids-associated cryptococcal meningitis in Rwanda (1983-1992). Epidemiologic and diagnostic feature. Journal of the Infection: 1999; (32) : 32-37.
- BOUREE P, THULLIEZ P, LEBRAS P, ELLORT A, PALLAZZO L, Quillard J, Caquet R and Drouet E. Cryptococcose diffuse chez un Zaïrois atteint de SIDA, Bull Soc Fr Mycol Med. 1984; (12):195-199.
- BOUREE P, THULLIRZ P. Cryptococcose- Encyclopédie-Médico-Chirurgicale ed. Paris-France 8127A10;6 1985. 5P
- CHARIYALERTSAK S, SIRISANTHANA T, SAENGWONLOEY O, NELSON K. Clinical presentation and risk behaviors of patients with acquired immunodeficiency syndrome in Thailand, 1994-1998: Regional variation and temporal trends. Clin Infect Dis, 32, 955-962.
- FRANCOISE D. Cryptococcose. La Revue du Praticien. 2001; (51):738-741.
- FRENCH N, GRAY K, WATREA C. Cryptococcal infection in a cohort of HIV-1 infected Ugandan adults. AIDS. 2002; 16:1031-1038.
- GENTILLINI M. Cryptococcose. Médecine Tropicale. 1993; Paris Flammarion P 277; 453-454; 600
- GENTILLINI M. Pathologies cérébro-meningées. Médecine Tropicale. Paris Flammarion.1993:599
- GORDON SB, WALSH AL, CHAPONDA M. Bacterial meningitis in Malawian adults: pneumococcal disease is common, severe, and seasonal. Clin Infect Dis. 2000;31: 53-57
- GRAY F, GHERALDI R, SCARAVILL I. Les mycoses du système nerveux central. Encyclopédie Médico-chirurgicale. Paris : Masson 1987; 8.
- HAKIM JG, GANGAIDZO IT, HEYDERMAN RS. Impact of HIV infection on meningitis in Harare: a prospective study of 406 predominantly adult patients. AIDS. 2000;14(10):1401-7.
- HALLOUA B, PRAZUCK. T. Cryptococcose. L’infection à VIH, de la clinique au traitement. Faculté de médecine Créteil – Université Paris XII; Premier Trimestre 1993: 125
- HOVETTE P, SOKO TO, RAPHENON G, CAMARA P, BURGEL PR, GRARAUD O. Cryptococcal meningitis in AIDS patients: An emerging opportunistic infection in Senegal. Transactions of the Royal Society of Tropical Medicine and Hygiene. 1999; (93) : 368.
- JEANDEL P, AUBRY P. La cryptococcose en 1988 ; Population et Santé Tropicales. Institut de Médecine tropicale du Pharo. 1989 ;36: 1-3.
- KALTHOUM K, HOUDA M, SLAH B, NAOUFEL B, BADREDDINE K, FAIÇAl Z, HELA BA, AHMED Z, EMNA C. La cryptococcose neuroméningée: Méningite du sujet immunodéprimé. La Tunisie Médicale. 1999;77:45-49.
- KILANI B, GOUBONTINI A, GASTLI M, TIOURI H, BELHAJ S, BEN CT, ZOUITEN F. Cryptococcose neuroméningée et infection par le VIH : Expérience tunisienne à propos de 6 cas. Journal de Mycologie Médicale 1997;7:97-99.
- LAROCHE R. TOUZE J F : Cryptococcoses associées au SIDA en Afrique. In : Dumas M, Giordano C, Gentilini M, Chieze F Neurologie tropicale. Paris : AUPELF-UREF; JOHN EIBBEY EUROTEXTE. 1993 ;183-184
- MILLOGO A, KI-ZERBO GA, ANDONABA JB, LANKOANDÉ D, SAWADOGO A, YAMÉOGO I, SAWADOGO AB. La cryptococcose neuroméningée au cours de l’infection par le VIH au centre hospitalier de Bobo Dioulasso (Burkina Faso). Bull Soc Pathol Exot, 2004 ;97 :2 : 119-121.
- MICHAEL SS, RICHARD JG, ROBERT AL, PETER GP, JOHN RP, William G, Powderly JDS, William E D. Practice Guidelines for the Management of Cryptococcal Disease, Clinical Infectious Diseases 2000;30:710-8.
- MINISTERE DE LA SANTE PUBLIQUE; PROGRAMME NATIONAL DE PRISE EN CHARGE SANITAIRE ET PREVENTION IST/VIH/SIDA; STATVIEW. Enquête nationale sur la séroprévalence du VIH/SIDA en Guinée (ESSIDAGUI) 2002. Rapport final juillet 2002.
- SOW PS, DIOP BM, DIENG YNM, SEYDI M, DIENG T, BADIANE S, SECK AM et al. Cryptococcose Neuroméningée au cours de l’infection à VIH à Dakar. Médecine et Maladies Infectieuses. 1998; 28 :511-515.
- SUSHEEL K, AJAY W, ARUNALOKE C, AMAN S, PRADEEP B, SURJIT S. Cryptococcal Meningitis in HIV infected, Experience from North Indian tertiary center. Neurology India. 2008;56:444-449.
- TIHANA B, THOMAS S. Cryptococcal meningitis. British Medical Bulletin. 2004; 72: 99-118.