CLINICAL STUDIES / ETUDES CLINIQUES
CLINICAL EXPERIENCE AND OUTCOME OF PITUITARY SURGERY IN KENYAN PATIENTS AT THE KENYATTA NATIONAL HOSPITAL
EXPÉRIENCE ET RÉSULTATS DE LA CHIRURGIE HYPOPHYSAIRE CHEZ DES PATIENTS KENYANS AU KENYATTA NATIONAL HOSPITAL
- Division of Neurosurgery, Department of Surgery, Kenyatta National Hospital, University of Nairobi, Nairobi, Kenya
- Department of Neurosurgery , Kenyatta National Hospital, Nairobi, Kenya
E-Mail Contact - KIBOI Julius Githinji :
ABSTRACT
Introduction
Surgical extirpation of pituitary lesions and can be perfomed by craniotomy or trans-sphenoidal hypophysectomy. This could be for pituitary ablation, excision of pituitary adenomas, craniopharyngiomas, suprasellar meningiomas and other types of tumors of the sellar region. Despite this being a common neurosurgical procedure there is a paucity of data on the local Kenyan experience and outcomes following pituitary surgery.
Study Design and Site
A retrospective study at the Kenyatta National Teaching and Referral Hospital.
Objectives
To evaluate the clinical presentation, management and outcome of patients undergoing surgery for pituitary lesions at the Kenyatta National Hospital.
Patients and Methods
Following ethical approval, patients’ records were retrieved and assessed for clinical and radiologic features of pituitary lesions, surgical treatment and post operative outcome. All the data was coded and analysed using Statistical Package for Social Sciences (SPSS) version 16.0.
Results
Sixty five patients, 39 (60%) female and 26 (40%) male patients were included. The mean age was 36.88 years (+ 14.689). The most common presentation were visual disturbances reported by 57 (87.7%) of the patients having reduction in visual acuity, while 37 (56.9%) had bitemporal hemianopia. Sixty two (95.4%) patients were operated during the study period and of these 28 (45.2%) by the transphenoidal approach as opposed to 34 (54.85%) by craniotomy. The pterional trans-sylvian approach was the most prevalent of transcranial hypohysectomies accounting for 17 (50%) patients, while 15 patients (44.1%) were operated by the subfrontal approach and two patients were operated via midline trans-callosal approach. Majority (96.4%) of trans-sphenoidal hypophysectomies were by sub-labial incision. Fifty (76.9%) of the patients had good functional outcome while 11 (16.9%) and 4 (6.2%) suffered moderate and severe disability respectively. Patients’ age (p=0.0029), duration of symptoms prior to surgery (p=0.0018) and surgical management versus conservative (p=0.001) significantly affected patient outcome. There was no statistically significant difference in outcome between patients of different sex (p=0.058) or the type of operation performed (p=0.191).
Conclusion
Transsphenoidal and trans-cranial approaches are effective and safe treatment strategies for pituitary lesions with low morbidity, mortality and recurrence rates.
Key Words: Pituitary tumors, Trans-sphenoidal, Hypophysectomy, Craniotomy
INTRODUCTION
Pituitary adenomas account for 10 to 15 % of all intracranial tumors and in addition to suprasellar tumors such as craniopharyngiomas, meningiomas, germinomas and low grade gliomas, account for a significant portion of the surgical workload of any neurosurgical practice30. Tumors of the suprasellar region assume importance because of their anatomical proximity to the anterior visual apparatus and neuroendocrine structures (the pituitary gland and hypothalamus) which influences their clinical presentation and progression.
Surgical extirpation is the treatment of choice for pituitary adenomas and other types of tumors of the sellar region and clivus. Pituitary and sellar mass lesions presenting with chiasmatic syndrome, ophthalmoplegia, pituitary apoplexia or endocrine derangement can undergo successful surgical removal34. Access to the pituitary may be achieved by craniotomy via subfrontal, pterional and sub-temporal approaches. In addition, the transsphenoidal route is widely accepted as the approach of choice for intrasellar lesions and some centers have also advocated the transsphenoidal route for tumors with subdiaphragmatic origin and subsequent suprasellar extension9. These subdiaphragmatic lesions are thought to be more easily removed by a transsphenoidal approach because the expanded sella provides a widened aperture to the suprasellar compartment and also diaphragmatic protection from pial invasion26. Further, the transsphenoidal approach has a number of variations, including the sublabial transseptal, transnasal endoscopic, endonasal rhinoseptoplastic, and transnasal septal displacement26, 37.
However, despite the major advances, reported success rates and low morbidity and mortality, there is a paucity of local data regarding the Kenyan experience and outcomes of this popular procedure. Kenyatta National Hospital is a teaching and referral hospital with a bed capacity of over 2000 patients. Through this centre the majority of neurosurgical referrals are managed. We reviewed the records of patients who were treated for pituitary tumors in the neurosurgical unit.
METHODS
Following ethical approval, the records of patients who presented to the Kenyatta National Hospital and underwent surgery for pituitary lesions from June 2000 to June 2010 were retrieved and reviewed. Patient biodata, type and duration of symptoms, hormonal profile and management modalities were recorded in a pre-formed questionnaire. A data entry interface was created through which codified data was entered and data analysis carried out using Statistical Package for Social Sciences (SPSS) version 16.0.
Frequencies and means were computed for description of the various variables and presented in prose form and as pie charts and graphs. The association between categorical variables was calculated using Chi-square test while comparison of mean values was performed using the one-way analysis of variance test (ANOVA).
RESULTS
Biodata and Clinical Presentation
A total of 65 patients fit the inclusion criteria during the study period and their files were retrieved and reviewed. There were 39 (60%) female as compared to 26 (40%) male patients (Figure 1).
The mean age was 36.88 (+ 14.689) with a range from 2 years and 6 months to 72 years. Majority of the patients (55%) were aged between 26 and 45 years whereas pediatric patients (aged less than 13 years) and elderly patients (over 61 years) accounted for 5% each (Figure 2).
The most common presentation were visual disturbances reported with 57 (87.7%) of the patients having reduction in visual acuity, while 37 (56.9%) had bitemporal hemianopia on confrontational and formal perimetry. Fundoscopy findings were reported for 39 patients with 24 (61.5%) of these being normal and optic atrophy and papilledema being reported for 29% and 9.5% respectively. The right and left eyes were each affected in 8 cases (12.3%) with bilateral involvement in 41 (63.1%) and 8 patients had no ocular involvement. Forty eight patients (73.8%) reported headaches while only 6% and 5% reported vomiting or convulsion respectively.
Amenorrhea and primary infertility were the presenting complaint of 11 (16.9%) patients while 14 (21.5%) and 8 (12.3%) had galactorrhea and gynecomastia respectively. Ten patients (15.4%) had acromegalic features of hypergnathia and enlarged hands and feet. In addition, 9 (13.8%) patients had erectile dysfunction, while 4 (6.2%) had atrophic testes with gynoid habitus and female hair distribution (Figure 3).
One patient aged two years and six months presented with features of precocious puberty. She had progressive breast development since eight months of age and at presentation was at tanner stage IV with growth of pubic hair from 11 months of age. In addition she experienced monthly mensrual-like flow from 1 year of age and had a post-pubertal uterus on ultrasound. She was however reported to have a normal growth rate.
Admission blood pressures were measured and recorded for all the patients and were classified using the World Health Organisation-International Society of Hypertension guidelines. Majority of the patients (65%) had optimal blood pressures while 7.5% and 5% had moderate and severe hypertension (figure 4). Also recorded were admission random blood sugars, of which 49 (75%) were normoglycemic and 12.5% each were gucose intolerant and within diabetic range each (Figure 5).
Data of the hormonal profile was also retrieved where available. Prolactin levels were recorded for 47 patients with 22 (46.8%) of them having hyperprolactinemia as compared to 21 (44.7%) and 4 (8.5%) having normal and low levels respectively. Majority of the patients were euthyroid (72.4%) while 10.3% and 17.3% were hyperthyroid and hypothyroid respectively. Cortisol levels were recorded for 41 patients of whom 4 had hypercortisolemia levels and 9 had normal with 8 patients having low levels (Table 1).
With regards to imaging, all the patients included in the study had a CT scan done while a further 8 (12%) and 5 (7.7%) had an MRI and 4-vessel angiography done respectively. The location of the lesion was described as completely intrasellar 15 (23.1%), sellar with suprasellar extension 40 (61.5%), suprasellar 5 (7.7%) or sellar with supra-, infra- and parasellar extension 5 (7.7%) (Figure 6).
Sixty two (95.4%) patients were operated during the study period, of these 28 (45.2%) by the transsphenoidal approach as opposed to 34 (54.85%) by craniotomy. In addition, there were 2 patients who had initially undergone transsphenoidal hypohysectomy who were re-operated transcranially for recurrences at 2 years and 4 years. The three patients who were not operated are included in the table below:
The pterional trans-sylvian approach was the most frequent of transcranial hypohysectomies accounting for 17 (50%) of these operations. Further, 15 patients (44.1%) were operated by the subfrontal approach with frontal lobe retraction and two patients were operated via midline trans-callosal approach. With regards to the 28 patients operated trans-sphenoidally, majority 27 (96.4%) were by sub-labial incision with blunt dissection up to the maxilla and nasal crest. Septal mucosa was then stripped up to the vomer which was excised. The ostia of the sphenoid were then identified, the body of sphenoid nibbled and the floor of the sella turcica opened. The tumor was then exposed, biopsied and removed by curette and suction.
One 37 year old patient who developed progressive blindness, erectile dysfunction and general weakness for 2 years had a pituitary tumor on CT and MRI with a sellar component, suprasellar extension, sphenoid bone erosion obliterating the sphenoid sinus and extension to both cavernous sinuses. He was scheduled for endonasal endoscopic biopsy as he was a poor anaesthetic risk for general anaesthesia due to persistent hypotension secondary to adrenocortical insufficiency.
Fifty (76.9%) of the patients in this series had good functional outcome with marked improvement in visual function, normalised post-operative hormone levels and regression of symptoms while 11 (16.9%) and 4 (6.2%) suffered moderate and severe disability respectively. There was no early post-operative mortality among this cohort. There was no statistically significant difference in outcome between patients of different sex (p=0.058). However, patients’ age was a significant indicator of outcome. Pediatric patients in this series had good functional outcome in comparison to patients above 61 years who developed severe disability (p=0.0029). In addition, the duration of symptoms prior to surgery significantly affected patient outcome (p=0.0018). Majority of the patients (24) who presented within 6 months had good outcome compared to none of the patients who presented after 5 years of symptoms. Findings on fundoscopy had a significant on visual outcome as patients in whom optic atrophy was reported had a higher incidence of blindness and thus severe disability in comparison with those in whom the fundoscopy was normal. Patients who were operated had a higher incidence of good functional outcome as compared to those managed conservatively (p=0.001) irrespective of the type of operation performed (p=0.191).
Transient fluid-electrolyte imbalance and diabetes insipidus (DI) was the most common postoperative complication (7.7% of the patients) in the present series. Hypothyroidism occurred in 6.2% of the patients as the second most common complication. In addition 2 patients has recurrences of tumor with clinical and radiological evidence at 2 and 4 years and had to undergo craniotomy and excision. Post-operative rhinorrhea was reported in 6.2% of the patients and was managed conservatively.
DISCUSSION
Although pituitary tumors are the most commonly encountered intracranial neoplasms, their true incidence has not been established with certainty. In literature, the prevalence of these tumors in autopsy series is reported to be 5-20%7, 27, 32 while most recent series estimate the prevalence of clinically apparent pituitary lesions to comprise approximately 10-15 % of all intracranial lesions10, 18. Improvement in radiographic imaging, biochemical detection of hormonal abnormalities, and microsurgical techniques have raised the number of surgical procedures, and in some series pituitary adenomas represent approximately 25% of surgically resected intracranial neoplasms; however, this may reflect a bias that reflects the interests of the surgeon or institution.
In the current study, there is a slight majority of 39 (60%) female as compared to 26 (40%) male patients. Previous studies report that pituitary tumors tend to afflict both sexes equally3, 5, 18. In addition, the mean age was 36.88 years (+ 14.689) with most of the patients (55%) were aged between 26 and 45 years and fewer patients at both extremes of age. There is a wide range of reported mean ages in literature ranging from 39.8 years40 to 50.4 years10. Reported incidence rates demonstrate an increase with age for both clinically apparent and autopsy diagnosis of pituitary tumors. In this regard, autopsy analyses and imaging studies report that more than 30% of people 50 – 60 yr of age harbor clinically undetected tumors 5, 7, 28, 31. Further, it is widely reported that pituitary adenomas are infrequent in childhood accounting for only about 3.5- 8.5% of pituitary adenomas which are diagnosed before the age of 20 yr 23, 33. Childhood tumors exhibit a female preponderance, and it has been suggested that they are smaller, less invasive, and less aggressive than tumors of adults23.
Patients with pituitary tumors present with signs and symptoms related to mechanical effects of an expanding tumor within the sella turcica (headaches, visual disturbances and cranial nerve palsies), excessive or impaired hormone production3. The most common presentation in this series, were visual disturbances reported by 57 (87.7%) of the patients with reduction in visual acuity. Chang10 reported that in an American population, over one half of patients presented with visual disturbance while other studies have reported a prevalence rate of up to 90%19, 39. The classic bitemporal field loss is found in chiasmatic compression and was described by 37 (56.9%) of the patients. These patients frequently complain of bumping into objects on one or both sides of the contracted visual field, reflecting both unilateral and bitemporal field loss. However, early compression may lead to upper quadrantic defects secondary to inferior chiasmal fiber compression.
Central vision may be affected by direct compression of the intracranial optic nerve. This may present as a blurring of vision or scotomatous central field defects. This is more common in individuals with a “post-fixed” chiasm – an anatomical variation where the chiasm is situated further back, thus exposing more optic nerve to the compressive effects of an expanding adenoma 25. If compression has been longstanding, fundoscopy may reveal optic atrophy which was observed in 10% of the current population. In our study, 50 (87.7%) the patients had improved visual function following surgery. The reported results in literature of visual outcome after surgical management of pituitary and sellar tumors vary considerably among studies, with improvement rates ranging from 36 to 80% 2, 4, 20, 21, 24, 25.
Hypertension is an important complication of pituitary tumors and contributes to the increased morbidity and mortality of this condition. In the current study, 12.5% of the patients had moderate and severe hypertension. Bondanelli6 reported that the prevalence of hypertension in acromegalic patients is about 35%, ranging from 18 to 60% in different clinical series, while Chanson11 reported a range of 20% to 50% of patients. The exact mechanisms underlying the development of hypertension in pituitary lesions are still not clear but may include several factors including chronic hypervolemia (the plasma volume is 10% to 40% above normal due to increased renal sodium reabsorption at the distal tubule level) 12, 22. In addition, hypertension can also result from endothelial dysfunction29 and it has been postulated that insulin resistance and diabetes may also play a role in the onset of hypertension13. Recent studies indicate that an increased sympathetic tone could play an important role in development and maintenance of elevated blood pressure6.
With regards to surgical approaches, 28 (45.2%) patients were operated by the transsphenoidal approach as opposed to 17 (45.83%). 15 (37.5%) and 2 patients by pterional, subfrontal and midline trans-callosal approaches respectively. However, as the current study was retrospective in nature the indications for choice of approach were not accurately captured in data. When analysed over time, more of the recent surgeries were increasingly via of the transsphenoidal route. This not-withstanding, there was gradual shift towards the transsphenoidal route likely guided by an increase in proficiency and the reported lower morbidity in other populations.
The choice for transphenoidal approach as opposed to craniotomy is determined by a number of factors including degree of suprasellar extension, cavernous sinus invasion, tumor consistency, brain invasion and cerebral edema as well as encasement of the optic apparatus41. Tumors with significant suprasellar extension, especially through the plane of the hypothalamus and floor of the third ventricle, have been correlated with significantly worse postoperative outcomes 14, 35. As such, particular features of suprasellar extension that mandate additional consideration prior to an operation are intraventricular extension, displacement or edema of the hypothalamus, displacement/compression of the proximal branches of the ACA, and involvement of the perforating arteries off the ICA and ACA1, 15, 17, 38.
Firm tumor consistency creates an inherent limitation in the ability to completely deliver the suprasellar tumor component via any transsphenoidal approach. Tumor consistency remains one of the most important, yet elusive, factors in the consideration of an trans-sphenoidal versus open craniotomy for skull base tumors. If a tumor’s consistency is known to be fibrotic ahead of time (as in some cases of reoperation), thus making it less amenable to suction, dissection and gross total resection, this should provide added support for consideration of an open approach. On the contrary, a primarily cystic or hemorrhagic appearance on MR imaging, especially a fluid-fluid level, can often lend support to selecting a less invasive approach for sellar region tumors 16. In the future, a priori knowledge of tumor consistency may lend major support to the selection of a skull base approach from above versus below and warrants further research.
Although cavernous sinus invasion is by no means a contraindication to selecting a transsphenoidal approach, its presence is known to limit the extent of tumor resection 42. In addition, the anatomical relationship of the tumor to the optic chiasm, the degree of circumferential encasement of the optic nerve, and invasion of the optic foramina each require careful preoperative consideration. In the majority of suprasellar pituitary adenomas, the plane between the tumor pseudocapsule and arachnoid membrane is preserved, and the tumor can be safely debulked or removed in its entirety from below. If visual loss is the major indication for surgery, the surgeon must be satisfied that the transsphenoidal approach can safely and effectively decompress the optic nerve and chiasm. Otherwise, the patient may be better served by an open craniotomy with direct visualization of these structures, such as a frontoorbital or supraorbital subfrontal eyebrow craniotomy 36.
CONCLUSION
In conclusion, key advances have been made to improve the ability to safely treat patients with larger and increasingly complex tumors of the anterior and middle skull base since the re-emergence of the transsphenoidal approach. Nevertheless, patient selection remains of paramount importance in guiding the decision to perform a particular surgical approach for a given tumor, and it remains clear that, for the time being, some patients with large sellar and parasellar region tumors are better served by performing one of many variations of an open craniotomy (such as a pterional, frontoorbital, subfrontal, or interhemispheric approach)8. This study highlights the experience and outcomes following pituitary surgery in a Kenyan referral hospital. It demonstrates that good surgical outcomes can be achieved by both the trans-sphenoidal and craniotomy approaches based on the indications and tumor characteristics. There is a need to carry out a prospective study with closer assessment of hormonal profile and response to surgery as well as perioperative management and longer follow-up for outcome. It however, demonstrates the current clinical status and lays a foundation for further inquiry of this subject that is central to neurosurgical practice.
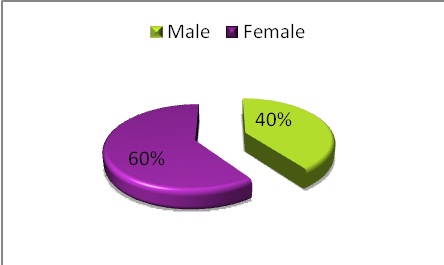
Figure 1: Illustration of the patient distribution by sex
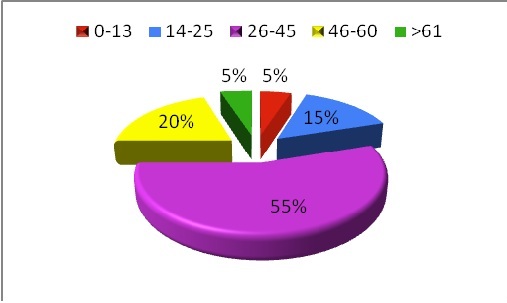
Figure 2: A pie chart demonstrating the distribution by age of patients with pituitary tumors managed at the neurosurgical unit. The majority of the patients were aged between 26-45 years.
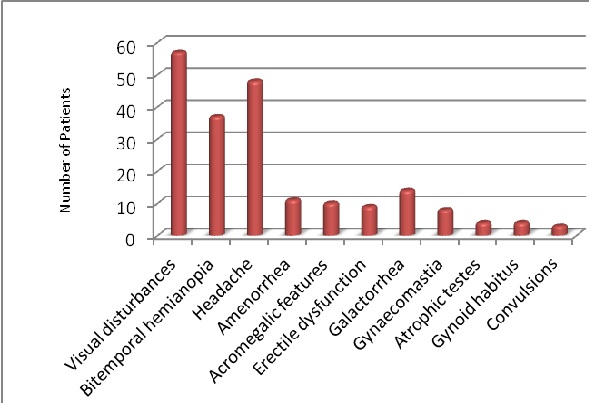
Figure 3: A bar graph showing the frequency of common presentations of patients with pituitary lesions
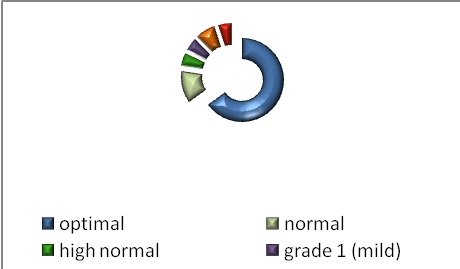
Figure 4: An illustration of the distribution of admission Blood Pressure accoring to the World Health Organisation-International Society of Hypertension guidelines. Grades 1, 2 and 3 refer to the severity of hypertension
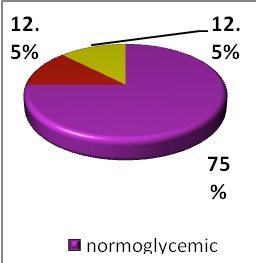
Figure 5: A pie chart representing the proportions of with the various blood sugar levels. Where normoglycemic refers to random blood sugars ¡Ü6.9mmol/L, glucose intolerance (7-11 mmol/L) and diabetes (¡Ý11.1 mmol/L).
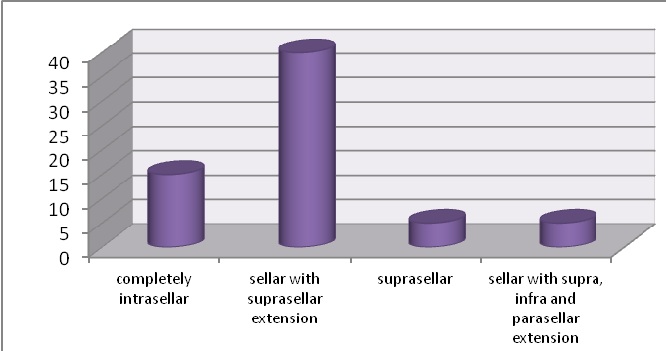
Figure 6: Location of pituitary lesions as seen on CT scan

REFERENCES
- ALLEYNE CH JR, BARROW DL, OYESIKU NM. Combined transsphenoidal and pterional craniotomy approach to giant pituitary tumors. Surg Neurol 2002;57:380-390
- ANDREWS BT, WILSON CB. Suprasellar meningiomas: the effect of tumor location on postoperative visual outcome. J Neurosurg 1988;69:523-528
- ARAFAH B M, NASRALLAH M P. Pituitary tumors: pathophysiology, clinical manifestations and management. Endocrine-Related Cancer 2001;8:287-305
- ARAI H, SATO K, OKUDA, MIYAJIMA M, HISHII M, NAKANISHI H. Transcranial transsphenoidal approach for tuberculum sellae meningiomas. Acta Neurochir (Wien) 2000;142:751-757
- ASA AND EZZAT ELSTER AD. Modern imaging of the pituitary. Radiology 1993;187:1-14
6-# BONDANELLI M, AMBROSIO MR, UBERTI EC. Pathogenesis and Prevalence of Hypertension in Acromegaly. Pituitary 2010;4;239-249
- BURROWS GN, WORTZMAN G, REWCASTLE NB, HOLGATE RC, KOVACS K. Microadenomas of the pituitary and abnormal sellar tomograms in unselected autopsy series. New England Journal of Medicine 1981;304 156-158
- CAPPABIANCA P, KELLY DF, LAWS ER JR. Endoscopic transnasal versus open transcranial cranial base surgery: the need for a serene assessment. Neurosurgery 2008;63:240-243
- CHAKRABARTI I, AMAR AP,COULDWELL W,WEISS MH. Long-term neurological, visual, and endocrine outcomes following transnasal resection of craniopharyngioma. J Neurosurg 2005;102:650-657
- CHANG EF, SUGHRUE ME, ZADA G, WILSON CB, BLEVINS LS, KUNWAR S. Long term outcome following repeat transsphenoidal surgery for recurrent endocrine-inactive pituitary adenomas. Pituitary 2010; 13:223-229
- CHANSON P, SALENAVE S. Acromegaly. Orphanet Journ of Rar Dis 2008;3:17-22
- CHANSON P, TIMSIT J, MASQUET C, WARNET A, GUILLAUSSEAU PJ, BIRMAN P, HARRIS AG, LUBETZKI J. Cardiovascular effects of the somatostatin analog octreotide in acromegaly. Ann Intern Med 1990; 113:921-5
- COLAO A, BALDELLI R, MARZULLO P, FERRETTI E, FERONE D, GARGIULO P, PETRETTA M, TAMBURRANO G, LOMBARDI G, LIUZZI A. Systemic hypertension and impaired glucose tolerance are independently correlated to the severity of the acromegalic cardiomyopathy. J Clin Endocrinol Metab 2000;85:193-9.
- DECKER RE, CHALIF DJ. Progressive coma after the transsphenoidal decompression of a pituitary adenoma with marked suprasellar extension: report of two cases. Neurosurgery 1991;28:154-158
- GOEL A, NADKARNI T, MUZUMDAR D, DESAI K, PHALKE U, SHARMA P. Giant pituitary tumors: a study based on surgical treatment of 118 cases. Surg Neurol 2004;61:436-446
- GOEL A, SHAH A, JHAWAR SS, GOEL NK. Fluid-fluid level in pituitary tumors: analysis of management of 106 cases. J Neurosurg 2010;112:1341-1346.
- GREENFIELD JP, LENG LZ, CHAUDHRY U, BROWN S, ANAND VK, SOUWEIDANE MM. Combined simultaneous endoscopic transsphenoidal and endoscopic transventricular resection of a giant pituitary macroadenoma. Minim Invasive Neurosurg 2008;51:306-309
- GSPONER J, DETRIBOLET N, JANZER R, USKE A, MIRIMANOFF RO, PEYMOND MJ, REY F, TEMLER E, GAILLARD RC , GOMEZ F. Diagnosis, treatment and outcome of pituitary tumors and other abnormal intrasellar masses. Retrospective analysis of 353 patients. Medicine 1999;78:236-269.
- ISMAILOV S, GROSSMAN A, POWELL M, KHALIMOVA Z, URMANOVA Y, MAKHKAMOV K, NARIMOVA G, AKBUTAEV A. Incidence and dynamics of visual disturbances in hypothalamus and pituitary mass lesions after transphenoidal surgery in the Republic of Uzbekistan. Endocr Abstr 2010;22: 580
- JANE JA JR, THAPAR K, KAPTAIN GJ, MAARTENS N, LAWS ER JR. Pituitary surgery: transsphenoidal approach. Neurosurgery 2002;51:435-444.
- JHO HD, CARRAU RL. Endoscopic endonasal transsphenoidal surgery: experience with 50 patients. J Neurosurg 1997;87:44-51
- KAMENICKY P, VIENGCHAREUN S, BLANCHARD A, MEDURI G, ZIZZARI P, IMBERT-TEBOUL M, DOUCET A, CHANSON P, LOMBES M. Epithelial Sodium Channel Is a Key Mediator of Growth Hormone-Induced Sodium Retention in Acromegaly. Endocrinology 2008;53:112-116
- KANE LA, LEINUNG MC, SCHEITHAUER BW, BERGSTRALH EJ, LAWS JR ER, GROOVER RV, KOVACS K, HORVATH E, ZIMMERMAN D. Pituitary adenomas in childhood and adolescence. J Clin Endocrinol Metab 1994;79:1135-1140
- KATO T, SAWAMURA Y, ABE H, NAGASHIMA M. Transsphenoidal transtuberculum sellae approach for supradiaphragmatic tumors: technical note. Acta Neurochir (Wien) 1998;140:715-719.
- KITANO M, TANEDA M, NAKAO Y. Postoperative improvement in visual function in patients with tuberculum sellae meningiomas: results of the extended transsphenoidal and transcranial approaches J Neurosurg 2007;107:337-346
- KITANO M, TANEDA M. Extended transsphenoidal surgery for suprasellar craniopharyngiomas: infrachiasmatic radical resection combined with or without a suprachiasmatic translamina terminalis approach. Surg Neurol 2009;71:290-298
- KONTOGEORGOS G, KOVACS K, HORVATH E, SHEITHAUER BW. Multiple adenomas of the human pituitary: a retrospective autopsy study with clinical implications. J Neurosurg 1991;74:243-7.
- KOVACS K, RYAN N, HORVATH E, SINGER W, EZRIN C. Pituitary adenomas in old age. J Gerontol 1980;35:16 -22
- MAISON P, DEMOLIS P, YOUNG J, SCHAISON G, GIUDICELLI JF, CHANSON P. Vascular reactivity in acromegalic patients: preliminary evidence for regional endothelial dysfunction and increased sympathetic vasoconstriction. Clin Endocrinol (Oxf) 2000,53:445-51
- MATSUYAMA J, KAWASE T, YOSHIDA K, HASEGAWA M, HIROSE Y, NAGAHISA S, WATANABE S, SANO H. Management of large and giant pituitary adenomas with suprasellar extensions. Asian J Neurosurg 2010;5:48-53
- MCCOMB DJ, RYAN N, HORVATH E, KOVACS K. Subclinical adenomas of the human pituitary. New light on old problems. Arch Pathol Lab Med 1983;107:488 – 491
- MOLITCH ME, RUSSELL EJ. The pituitary incidentaloma. Annals of Internal Medicine 1990;112:925-931.
- MUKAI K, SELJESKOG EL, DEHNER LP. Pituitary adenomas in patients under 20 years old. A clinicopathological study of 12 cases. J Neurooncol 1986;4:79 – 89
- ORUCKAPTAN HH, SENMEVSIM O, OZCAN OE. Pituitary adenomas: Results of 684 surgically treated patients and review of the literature. Surg Neurol 2000;53:211-219
- PUGET S, GARNETT M, WRAY A, GRILL J, HABRAND JL, BODAERT N. Pediatric craniopharyngiomas: classification and treatment according to the degree of hypothalamic involvement. J Neurosurg 2007;106:3-12
- REISCH R, PERNECZKY A. Ten-year experience with the supraorbital subfrontal approach through an eyebrow skin incision. Neurosurg 2005;57:242-255
- ROSS DA, WILSON CB. Results of transsphenoidal microsurgery for growth hormone-secreting pituitary adenoma in a series of 214 patients. J Neurosurg 1998;68(6):854-867
- SAITO K, KUWAYAMA A, YAMAMOTO N, SUGITA K. The transsphenoidal removal of nonfunctioning pituitary adenomas with suprasellar extensions: the open sella method and intentionally staged operation. Neurosurgery 1995;36:668-676.
- THOMAS R, SHENOY K, SESHADRI MS, MULIYIL J, RAO A, PAUL P. Visual field defects in non-functioning pituitary adenomas. Indian Journal of Ophthalmology 2002; 50: 127-130.
- UYGUR ER, GURSES L, CEM S, DENIZ B, MURAD B. Sublabial Transseptal Approach to Pituitary Adenomas with Special Emphasis on Rhinological Complications. Turkish Neurosurgery 2008; 18: 425-430
- ZADA G, DU ROSE, LAWS RE. Defining the “edge of the envelope”: patient selection in treating complex sellar-based neoplasms via transsphenoidal versus open craniotomy. J Neurosurg 2011; 114: 286-300.
- ZADA G, KELLY DF, COHAN P, WANG C, SWERDLOFF R. Endonasal transsphenoidal approach for pituitary adenomas and other sellar lesions: an assessment of efficacy, safety, and patient impressions. J Neurosurg 2003;98:350-358