
|
|||
|
CASE REPORT / CAS CLINIQUE
PITUITARY ASPERGILLOSIS ABSCESS IN AN IMMUNOCOMPETENT BLACK WOMAN. A CASE REPORT
ABCÈS ASPERGILLEUX PITUITAIRE CHEZ UNE FEMME NOIRE IMMUNOCOMPETENTE
E-Mail Contact - N’DRI OKA Dominique :
ndriokad@yahoo.fr
ABSTRACT Objective and Importance This article aims to describe a case of pituitary abscess from aspergillosis and discusses its diagnostic problems. Clinical Presentation Treatment Conclusion Keywords: Pituitary Aspergillosis, Pituitary Adenoma, Aspergillosis Abscess INTRODUCTION Pituitary abscess is a rare condition; however, it can be life-threatening in the event of delayed diagnosis or inadequate treatment [1,6,10]. It is often discovered during surgery through the presence of pus in the sella, during resection of a presumed pituitary tumour [2, 5]. In most cases, these abscesses are caused by bacteria [6, 7]. The pituitary abscess of fungal origin is extremely rare. Aspergillus fumigatus is the most encountered pathogen [1]. The contamination of the sella generally follows the infection of para-nasal sinuses by inhaling fungal spores in the air [4]. The spread of aspergillus in the central nervous system is usually fatal in 100% of cases. The objective is to describe a case of pituitary abscess from aspergillosis and discuss its diagnostic problems. CASE REPORT An immunocompetent 26-year-old black woman complained of retro-orbital headache for several years. Neurological examination was normal. Endocrinological examination demonstrated amenorrhea galactorrhea syndrome. She had bilateral galactorrhea through light pressure of the nipple (Figure1). A Head CT scan with and without injection of contrast, focused on the sellar region showed rounded hypodense mass (volume, 1.5 x 2.5x 2.3 cm) with enhancement at the periphery after injection (Figure 2). There was an extension into the sphenoid sinus which density is metallic (Figure 3). So that diagnosis of pituitary adenoma or sphenoid sinus aspergillosis was evoked. Hormonal assessment found a 180 ng / ml hyperprolactinemia (normal value was inferior from 5.18 to 26.53 ng / ml) and anadrenocorticotrophic hormone (ACTH) level slightly decreased to 5.7 ng/ ml. The other hormone levels were normal. The ophthalmological assessment showed no visual field abnormalities associated. Blood electrolytes were normal. Complete blood count revealed red blood cell count 4.170.000cells/mm3,hemoglobin level 10.5 g/dl , hematocrit 26.8 %, platelet count 79.000 platelets/mm3, white blood cell count 5.980 cells / mm3,fibrinogen level was 2.70 g/l (normal value is between 2 and 4 g/l) . The coagulation profile was normal prothrombin 100%, activated chaolin time 13 »6/13 »5, and its international normalized ratio (INR) 1.0. Urea and creatinine rates were respectively 0.13 g / l and 04 mg / l. Hepatic enzyme rate was ASAT 30 IU/l, ALAT 26 IU/l. The sella mass was completely removed via a transsphenoidal approach. At surgery, a pale area with yellow pus was found within the normal pituitary gland. The diagnosis of aspergillosis was confirmed through histopathology; there was a dense thatch of hyphae entangled in a focus of necrosis (Figure 4). As a result, the retroviral serology and the Aspergillus serology performed; both were negative. Amenorrhea galacthorea syndrome dispread one month after surgical excision after the operation, amphotericine-B (25mg/d) and itraconazole (800 mg/d) therapy was started. Amenorrhea galacthorea syndrome dispread one month after surgical excision Hormonal assessment showed a tendency towards normalization of serum prolactin. During a 6-month follow-up, the patient’s headache disappeared. Repeat Head CT scan showed no recurrence after a follow up of one year. Postoperative course was good; no complication was observed DISCUSSION Aspergillus fumigatus is a ubiquitous filamentous fungus that grows on a variety of organic substances [10] The prevalence of sinus location is difficult to assess in our countries especially as requests for histopathology are rare as regards curettage product for chronic sinus sinusitis [3]. Factors predisposing to infection are divided into: – Local factors causing relative anaerobic sinus by chronic hypoventilation related to ostial dysfunction; – General factors such as immunodeficiencies, systemic or neoplastic diseases, diabetes, and corticosteroid therapy; – Environmental factors leading to a multitude of spores which explains the frequency among cereal farmers, pigeon breeders, wigmakers and seed merchants [3, 7, 8]. – The invasive form of aspergillosis with intracranial extension has a poor prognosis [7]. The sphenoid sinus, due to its intimate anatomical relationship with the base of the skull and particularly the sella turcica, is the most common point of entry for aspergillus. Contamination of soft tissues as well as bony structures of the skull base is caused by the penetration of the fungus in the connective tissues; invasion of vascular wall is facilitated by secretion of fibrinolytic and cytotoxic agents causing thrombosis and tissue necrosis and emboli with a risk of colonization by the haematogenous route of orbits and/or the brain [4, 10]. Before surgical excision of sellar mass aspergillus diagnosis is difficult. Clinical similarity with pituitary tumours has been emphasized by most authors [1, 6 7,9]. A clinical picture in both cases is dominated by headache, visual disturbances and endocrine syndrome. The occurrence of diabetes insipidus was the most frequently observed in cases of pituitary abscess [1, 2, 5]. The extent of the severity of symptoms depends on the extent of compression of the pituitary gland by the abscess. [5] The skull radiograph usually shows a widening of the sella tucirca with some erosion of the sellar floor [3, 6, 8]. The CT scan reveals a hypodense spherical lesion with contrast enhancement ring after injection of contrast material [4, 8]. Histopathology resulted, in the diagnosis of aspergillosis after surgical excision of the lesion, as was the case in other series. [1, 3, 4, 7, 10] .The transsphenoidal surgery approach is the preferred treatment of sellar aspergillosis. Craniotomy by sub-frontal approach is not recommended as it could promote the spread of aspergillus in the subarachnoid space with a risk of contamination of the central nervous system [5, 7]. A case of death of a patient by aspergillus meningo-encephalitis was reported by Goldhammer [4] after the removal of a subcutaneous aspergillus abscess by subfrontal approach. The filling of the sella by fatty tissue after excision of the pituitary abscess helps to avoid recurrence, as well as the occurrence of a syndrome of empty sella [7]. The addition of anti-fungal chemotherapy after surgery is recommended [8, 10]. The use in amphotericin B alone or in combination with 5 Fluorocytosine or Itraconazole for 2 months, allows for better healing of aspergillosis [2]. CONCLUSION A pituitary aspergillus abscess should be considered in the differential diagnosis of pituitary tumours. Confirmation of diagnosis is only by histopathology because the clinical and radiological findings are not specific. Surgical excision followed by antifungal medical treatment ensures a therapeutic success.
Figures  Fig.1: bilateral galactorrhea in black woman with pituitary mass  Fig.2 Coronal CT scan showing hyperdensity in sphenoid sinus  Fig.3 Coronal CT scan showing typical image of an intrasellar abscess 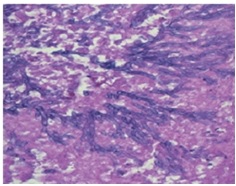 Fig.4 Photomicrograph of the intra sellar mass showing fungal organisms with septate hyphae and dichotomous branching, consistent with Aspergillus. hematoxylin and eosin ×100 REFERENCES
|
© 2002-2018 African Journal of Neurological Sciences.
All rights reserved. Terms of use.
Tous droits réservés. Termes d'Utilisation.
ISSN: 1992-2647