CASE REPORT / CAS CLINIQUE
LARGE INTRADIPLOIC EPIDERMOID TUMOR OF THE SKULL: CASE REPORT AND REVIEW OF LITERATURE
TUMEUR ÉPIDERMOÏDE GEANTE, INTRA- DIPLOÏQUE DU CRÂNE. A PROPOS D'UN CAS ET REVUE DE LA LITTÉRATURE
- Department of Neurological Surgery, Mayo Clinic-Scottsdale, 13400 East Shea Blvd, Scottsdale, AZ 85259
- Department of Neurological Surgery, Mount Sinai School of Medicine, One Gustave L. Levy Pl, New York, NY 1002
ABSTRACT
Background
A rare case of a large intradiploic epidermoid tumor of the parietal bone is described and recent literature pertaining to radiological evaluation and the surgical treatment of these lesions is reviewed.
Methods
A 70-year-old female patient was noted to have a painless subcutaneous swelling 15 years ago. She currently presented with complaints of unsteady gait, occasional episodes of vertigo, tinnitus and a constant fear of falling. Evaluation with a Computed Tomographic scan (CT) and Magnetic Resonance Imaging (MRI) revealed an epidural non-enhancing mass in the mid-parietal region, extending into the Sylvian fissure, medially and laterally. The patient underwent a computer-assisted stereotactic craniotomy followed by a total microsurgical resection of the tumor. The large cranial defect produced by the tumor resection was repaired with a titanium wire mesh and methyl methacrylate cranioplasty.
Result
The patient had an uneventful post-operative course and was discharged home in good condition. A review of the literature shows that intradiploic epidermoid tumors of the parietal bone are rare. Complete resection without adjuvant therapy is the mainstay of treatment.
Conclusion
Correct radiological assessment and complete excision of these lesions and their capsules can reduce the risk of recurrence and prevent the lesion from undergoing malignant transformation. Total removal of the tumors is associated with a very good long-term prognosis.
Epidermoid Tumor of the Skull
Key words: Epidermoid cyst, Intradiploic tumor, Skull tumor
RESUME
Un cas exceptionnel de tumeur géante épidermoïde pariétale est décrit associé à une revue de la littérature en insistant sur l’évaluation radiologique et le traitement chirurgical.
Une femme de 70 ans se plaignant d’une tuméfaction crânienne, sous-cutanée indolore évoluant depuis quinze ans a été prise en charge. Elle présentait des troubles de la marche, des épisodes occasionnels de vertiges, d’une peur constante de faire une chute. Le bilan radiologique a comporté un CT-scan, une IRM. Il a été mis en évidence une masse épidurale au niveau de la région pariétale moyenne ne prenant pas les contrastes et s’étendant vers la fissure sylvienne médialement et latéralement.
Une crâniotomie avec l’aide de la neuronavigation, suivi d’une résection microchirurgicale de la tumeur a été réalisée. Le défect osseux a été comblé par une crânioplastie. Les suites opératoires ont été simples.
Une revue de la littérature montre que les tumeurs épidermoïdes intra-diploïques au niveau de l’os pariétal sont rares. Une résection complète sans traitement spécifique complémentaire permet une guérison.
Un bilan radiologique précis et une exérèse complète de ce type de lésion incluant la capsule réduit de manière significative le risque de récidive et prévient l’éventualité d’une transformation maligne.
INTRODUCTION
Intradiploic epidermoid cysts are fairly uncommon lesions in neurosurgical practice. They are generally slow-growing congenital neoplasms, arising from the ectodermal cells within the neural groove between the 3rd and 5th weeks of embryogenesis at the time of its closure to form the neural tube, and subsequently remain within the cranial bones (1, 2, 6, 7, 13, 15, 31, 30). The more common medial location of many of these tumors is explained by the fact that the neuroectoderm separates dorsally along the midline (31). The inclusion of cell nidi in the secondary vesicles during the fifth week of embryonic life accounts for instances of lateral localization of these lesions (7). Alternatively, transformation of ectodermal cells may occur at a later stage during the development of otic and optic vesicles, leading some authors to postulate that this later inclusion gives rise to the tumors of the diploe and scalp (23). Epidermoid tumors generally account for 0.4 to 1.8% of all intracranial lesions, usually arising in cerebellopontine angle (CPA), parapituitary area, and rhomboid fossa, and often growing extensively before presenting with clinical symptoms (1, 2, 13, 19, 23, 26, 28). Sometimes a palpable lump is the initial symptom, while focal neurological dysfunction may result from compression of adjacent neural structures (15, 21, 24). Additional complications arise after rupture of epidermoid cysts release cholesterol breakdown products into the cerebrospinal fluid possibly causing chemical meningitis, ventriculitis, or tension pneumocephalus (1, 22). It is important to differentiate between epidermoid cysts and cholesterol granulomas when making a diagnosis, especially if the former occupy a more medial position at the petrous apex or clivus (2). Correct diagnostic radiological assessment with MRI followed by total surgical removal is the ideal treatment. We report a case of a large intradiploic epidermoid cyst and analyze the treatment as well as the clinical and radiological features of the lesion in light of the recent literature.
CASE REPORT
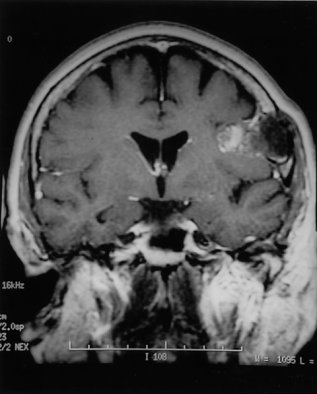
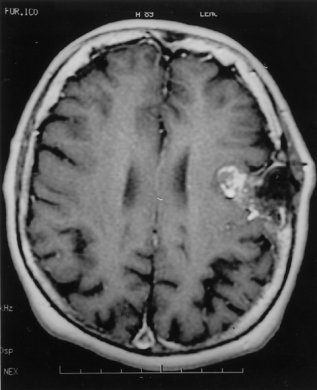
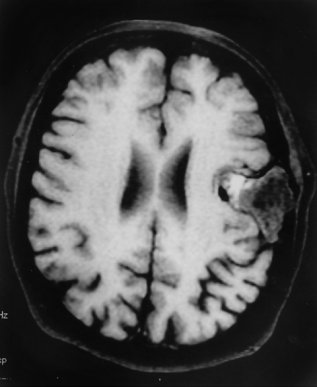
A 70-year-old female had a painless subcutaneous swelling over her left parietal convexity, which was noticed by her hairdresser approximately 15 years ago (Fig. 1). She sought a medical consultation complaining of occasional episodes of vertigo, tinnitus, unsteady gait, and a constant fear of falling. At the time of the work-up for vertigo she reported an absence of headaches and other neurological symptoms. In view of her complaints a comprehensive evaluation was carried out including brainstem evoked responses, and audiometric testing. Multiple MR images of the patient’s brain were obtained including sagittal T1 scans, axial double echo T2 images, as well as additional pre- and post Gadolinium enhanced axial and coronal T1 weighted images. Selected fat suppressed axial T1 weighted images were also obtained. Examination of the scans revealed a lesion measuring 3.6 cm. in anterior-posterior direction x 3.5 cm. in transverse direction x 3 cm. in cephalocaudal dimension (Fig. 2). The lesion appeared benign and was centered in the epidural space. On several images, however, there were noted to be intradural extensions allowing a portion of the tumor to invaginate into the adjacent left Sylvian fissure. (Fig. 3) The lesion had variable fat and fluid contents and produced a signal of heterogeneous intensity. In its medial portion there appeared to be areas of T1, proton and T2 hyperintensity. These hyperintensities appeared to be suppressed on the fat suppression sequences (Fig. 4).
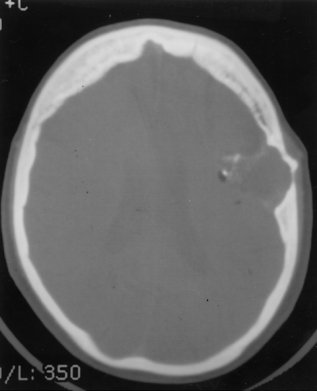
For correlative purposes, CT scans were obtained with pre- and post intravenous administration of nonionic contrast media, which likewise demonstrated an extra-axial lesion in the left fronto-temporal region. Further examination of the image demonstrated areas of calcification, fat and fluid within the tumor. There was no enhancement following intravenous administration of contrast media (Fig. 5). The lesion appeared to be centered in the epidural space and had intradural extensions into the left Sylvian fissure medially and laterally. Additionally, there was benign-appearing bony remodeling of the lesion in the inner and outer tables of the skull. The lesion also appeared to be breaking through the cortex into the subcutaneous tissue in the region of the left coronal suture (Fig. 6).
In view of these findings, the patient was referred for a neurosurgical consultation. Her comprehensive neurological assessment was within normal limits and it was agreed to proceed with a complete surgical resection of the lesion. The patient was taken to the neurosurgical operating suite and a Stealth stereotactic-guided craniotomy was performed.
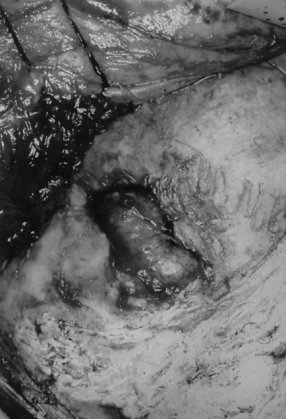
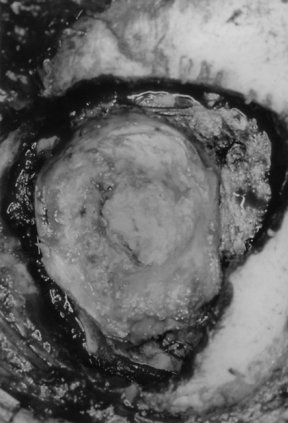
As the incision was carried through the temporalis muscle and pericranium, the tumor came immediately into view (Fig. 7). During the subsequent craniotomy the bone was removed in a piece-meal fashion as the tumor was found to be invading through the bone. The tumor appeared to have a distinct capsule. The most medial aspect of the tumor was found to be encapsulated by a pseudodura. The dura was then opened in a circumferential fashion and the medial aspect of the tumor capsule/dura was resected. A gross total resection of the pearly white tumor was achieved (Fig. 8). Within the tumor were multiple pieces of hair. The bone flap and other pieces of tumor were sent for a pathological evaluation that confirmed the diagnosis of an epidermoid cyst. Due to the fact that the tumor had produced a large bone defect, a cranioplasty was performed utilizing titanium wire mesh and methyl methacrylate. The postoperative course was uneventful, and the patient was discharged home several days later.
DISCUSSION
Epidermoid tumors are benign in nature and possess a characteristic thin capsule of stratified, keratinized squamous epithelium, covered by associated connective tissue. It is this very feature that allows for their histological differentiation from dermoid lesions (1). Their method of growth involves desquamation of epithelial cells with their eventual breakdown into keratin and cholesterol (21, 28). The growth of epidermoids at a slow, linear rate, approximating that of normal skin, allows the nervous system to adapt to their presence until a point is reached at which further compensation is no longer possible (21, 31, 35). Malignant change of epidermoid cysts is extremely rare, with Yanai (37) reporting 13 cases in the literature. In view of the unfavorable prognosis once the lesions progress to malignancy, the ideal treatment for the majority of the benign tumors is early detection and complete excision.
Intradiploic epidermoids are less frequent than the intradural variety, and commonly occur in the frontal, parietal and occipital bones of the skull. Their slow course allows them to attain considerable size, often presenting as a painless subcutaneous swelling and occasionally associated with a palpable bone defect (9, 10, 13, 15, 17, 35). Headache and focal epileptic seizures are among the most frequent symptoms. The differential diagnosis of intradiploic epidermoid cysts includes dermoid cyst, haemangioma, eosinophilic granuloma and, in the orbitofrontal region, cholesterol granuloma (3). Intradiploic epidermoids do not appear to be age-specific and may occur at any stage of life, with a mean age of 32 to 38 years (4, 8). Prevalence of these tumors seems to be equal among males and females, accentuating their difference from other epidermoids, which have a preference for males (8, 14, 28).
The radiological pattern of intradiploic epidermoids was first described by Cushing in 1922, who stated that these tumors involved an area of bone destruction, of lower density than the surrounding bone, with smooth sclerotic margins (11). Radiological findings commonly demonstrate that these tumors involve the inner table more than the outer, with the edges of the bony defect showing a dense clear-cut margin (7). The outstanding and differentiating feature of the cranial defect, however, is the sharply defined, dense, white, scalloped margin, which is not found in any other condition. Most other erosive lesions produce a defect in which the margin is less clearly defined (12).
Computed tomography provides a fairly characteristic appearance for intradiploic epidermoids, demonstrating a nonenhancing lesion with irregular margins (23, 24, 32). Zones of calcifications, as well as thinning of gaps between the tables are also easily seen. CT scans clearly delineate the site, size and status of bony table erosion. Intradiploic epidermoids usually appear hypodense compared with the brain on CT. While these lesions do not typically enhance following administration of intravenous contrast, a rim of contrast enhancement may be occasionally observed following enhancement of the fibrous capsule (22). Importantly, contrast enhancement is also an important finding of epidermoid carcinomas and its presence signals the possibility of the lesion having undergone malignant transformation (34). The level of bony detail seen on a CT scan serves as an advantage over other imaging modalities, allowing for better assessment of both skull involvement and intracranial extension of the lesion (3, 5, 6, 12, 25).
In recent years, MR imaging, with its superior delineation of anatomic detail and its ability to provide a more precise definition of a lesion’s irregular margins, extent, and relationship to the surrounding vascular and neural structures, has become a superior radiologic tool in the neurosurgeon’s arsenal for the investigation of intradiploic epidermoids. Particular advantages of MRI are demonstrated by the lack of skull base artifacts that are seen on many CT studies, as well as its superiority in distinguishing lesions in contact with the subarachanoid space and with the brainstem (23). Intradiploic epidermoid cysts have always been reported as giving a high signal on T2-weighted images, with variable signal on T1-weighted images (6). In a series by Kallmes, (20) reviewing MR images of 23 retrospective cases of intracranial epidermoid tumors, most of the epidermoids demonstrated a heterogeneous signal intensity slightly hyperintense to CSF on T1-weighted images, hyperintense to CSF on proton density-weighted images, and iso- or hyperintense to CSF in T2-weighted images. The ease with which signal difference between CSF and cyst content can be seen also allows the exclusion of an arachnoid cyst from the differential diagnosis, and it is especially useful for planning the surgical approach (25). Additionally, spectroscopic correlation suggest that lesions demonstrating T1 shortening have a high lipid content of mixed triglycerides with unsaturated fatty acid residues (18).
A possible complications that can arise as a result of intradiploic epidermoid tumors is the rare occurrence of spontaneous cyst rupture with subsequent discharge of the cholesterol content into the subarachnoid space, resulting in recurrent aseptic meningitis and frequently leading to chronic granulomatous arachnoiditis. Additional injury may be caused by the inflammatory reaction secondary to spillage of tumor cholesterol contents, with resulting fibrosis and further neurologic deficit, including trigeminal neuralgia (1, 31). The presence of chemical meningitis due to cholesterol spilling is a well-recognized complication of partial tumor removal and this risk can be greatly reduced with complete tumor excision. Further reduction in risk of postoperative chemical meningitis can be obtained with perioperative administration of steroids, as well as proper intraoperative irrigation of keratinaceous debris (31, 36).
The goal of surgery for epidermoid tumors is the complete removal of the tumor together with its capsule. The capsule is the only living and growing part of the neoplasm and must be carefully dissected from the bone and dura mater as well as the adjacent cortex (11). Several authors also emphasize the need to direct special attention to the inner table, as the tumor may often extend beneath it through various small defects in the bone and come to lie between the cranium and the dura. Exploration of the epidural space is required to assure the complete removal of the cyst wall (22).
In his series of 43 intracranial epidermoids, Yasargil also emphasized the need for complete surgical resection of these lesions in view of their lack of radiosensitivity and their tendency to recur if partially removed (38). Taking into account the growth rate of epidermoids, it is thought that the period of time required for the tumor to grow back to its original dimensions and become symptomatic would be equal to the patient’s age years at the time of surgical excision plus 9 months (31, 38). While it may be difficult to excise the tumor completely without increasing neurologic deficit, due to its common tendency to engulf surrounding cranial nerves and blood vessels with a moderately adherent capsule, an aggressive approach that results in the excision of the majority of the lesion is often associated with good results (2). However, partial resection of intradiploic epidermoids can lead to tumor recurrence and/or malignant transformation of the lesion. Repeat surgical resection is often required (3, 37). It is therefore important to attempt to achieve a total excision of an intradiploic epidermoid before it reaches the size that makes complete removal impossible (22). Additionally, when the removal of the tumor requires extensive excision of bone, cranioplasty with titanium mesh and methyl methacrylate may be necessary to repair the cranial defect (8, 10).
CONCLUSION
Intradiploic epidermoid tumors are benign, slow growing lesions that should be completely excised, providing a good long-term prognosis for the patient. Complete resection of the cyst lining cannot be overemphasized, as incomplete removal predisposes the patient to the risks of recurrence, inflammation and possibility of malignant transformation (37). Correct radiological assessment of these lesions with MRI and CT and complete removal of the tumor and its capsule are essential for adequate surgical treatment, allowing an excellent chance for a cure.
 Figure 1 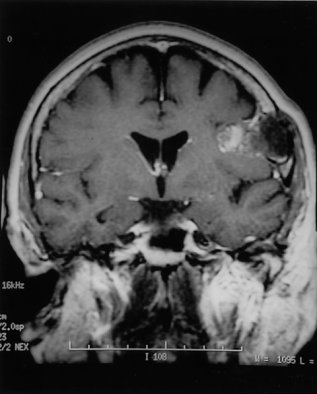 Figure 2 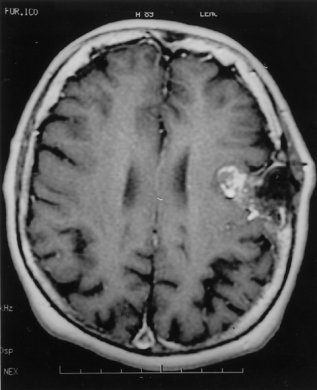 Figure 3 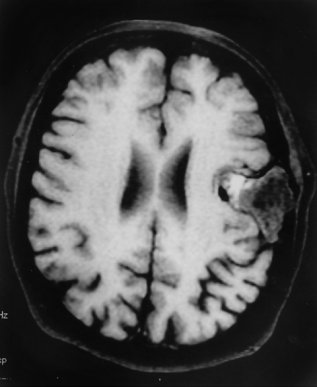 Figure 4  Figure 5 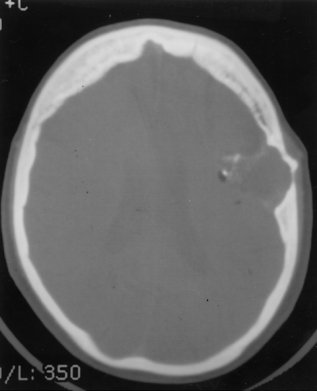 Figure 6 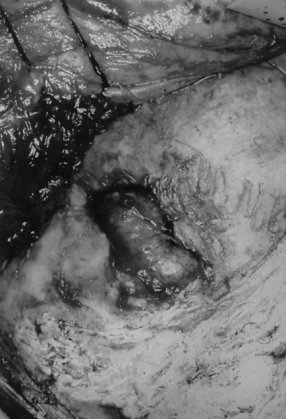 Figure 7 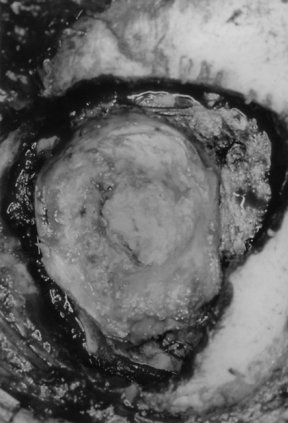 Figure 8
REFERENCES
- ABRAMSON RC, MORAWETZ RB, SCHLITT M: Multiple complications from an intracranial epidermoid cyst: Case report and literature review. Neurosurgery 24(4): 574-578, 1989.
- ALTSHULER EM, JUNGREIS CA, SEKHAR LN, JANNETTA PJ, SHEPTAK PE: Operative treatment of intracranial epidermoid cysts and cholesterol granulomas: Report of 21 cases. Neurosurgery 26(4): 606-614, 1990.
- ARANA E, LATORRE FF, REVERT A, MENOR F, RIESFO P, LIANO F, DIAZ C: Intradiploic epidermoid cysts. Neuroradiology 28(4): 306-311.
- BAXTER JW, NETSKY MG: Epidermoid and dermoid tumors: Pathology; in Wilkins RH, Rengachery SS (editors). Neurosurgery, Volume I. McGraw-Hill 1990 pp 655-661.
- BEJANARO PA, BRODERICK DF, GADO MH: Infected epidermoid cyst of the sphenoid bone. American Journal of Neuro-Radiology 14(3): 771-773, 1993.
- BOYKO OB, SCOTT JA, MULLER J: Intradiploic epidermoid cyst of the skull: Case report. Neuroradiology 36(3): 226-227, 1994.
- CANALE DJ, CLARKE HA, PAK YH, BURTON WD: Giant primary intradiploic epidermoid tumor of the skull: Case report. Surgical Neurology 2(1): 51-54, 1974.
- CIAPPETTA P, ARTICO M, SALVATI M, RACO A, GAGLIARDI FM: Intradiploic epidermoid cysts of the skull: Report 10 cases and review of the literature. Acta Neurochirurgia (Wien) 102(1-2): 33-37, 1990.
- CONLEY FK: Epidermoid and dermoid tumors: Clinical features and surgical managements; in Wilkins RH, Rengachery SS (editors). Neurosurgery, Volume I. McGraw-Hill 1990 pp 668-673.
- CONSTANS JP, MEDER LF, DIVITIS ED, DONZELLI R, MAURI F: Giant intradiploic epidermoid cyst of the skull: Report of two cases. Journal of Neurosurgery 62(3): 445-448, 1985.
- CUSHING H: A large epidermal cholesteatoma of the parietotemporal region deforming the left hemisphere without cerebral symptoms. Surgical Gynecoligical Obstetrics 34: 557-566, 1922.
- DIAS SP, MAY PL, JAKUBOWSKI J: Giant epidermoid cysts of the skull. British Journal of Neurosurgery 3(1): 51-58, 1989.
- DORAN SE, GEBARSKI SS, HOFF TT: Tumors of the skull; in Youmans JR (ed): Neurological Surgery, Volume 4. WB Saunders Company, 1996, pp 2999-3023.
- GUIDETTI G, GAGLIARDI FM: Epidermoid and dermoid cysts: Clinical evaluation and late surgical results. Journal of Neurosurgery 47(1): 12-18, 1977.
- GURIDI J, OLLIER J, AGUILERA F: Giant intradiploic epidermoid tumor of the occipital bone: Case report. Neurosurgery 27(6): 978-981, 1990.
- HASEGAWA H, BITOH S, NAHATA M, FUJIWARA M, YASUDA H: Intracranial epidermoid mimicking meningioma. Surgical Neurology 15(5): 272-274, 1981.
- HOLTHUSEN W, LASSRICH MA, STEINER C: Epidermoid and dermoids of the calvarian bones in early childhood: Their behaviour in the growing skull. Pediatric Radiology 13(4): 189-194, 1983.
- HOROWITZ BL, CHARI MV, JAMES R, BRYAN RN: MR of intracranial epidermoid tumors: correlation of in vivo imaging with in vitro 13C spectroscopy. American Journal of Neuroradiology 11(2): 299-302, 1990
- ISHIKAWA M, KIKUCHI H, ASATO R: Magnetic resonance imaging of the intracranial epidermoid. Acta Neurochirurgica Wien 101(3-4): 108-111, 1989.
- KALLMES DF, PROVENZALE JM, CLOFT HJ, MCCLENDON RE: Typical and atypical MR imaging features of intracranial epidermoid tumors. American Journal of Roentgenology 169(3): 883-887, 1997.
- LUNARDI P, MISSORI P, GAGLIARDI FM, FORTUNA A: Supratentorial epidermoid cysts. Neurochirurgia-Stuttg 35(1): 14-17, 1992.
- MILLER PJ, HOFFMAN R, HOLLIDAY R: Intradiploic epidermoid of the temporal bone: Case history and literature review. Otolaryngology-Head and Neck Surgery 111(6): 827-831, 1994.
- OLSON JJ, BECK DW, STEPHEN CC, MENEZES AH: Comparative evaluation of intracranial epidermoid tumors with computed tomography and magnetic resonance imaging. Neurosurgery 21(3): 357-360, 1987.
- OSBORNE DR: Epidermoid and dermoid tumors: Radiology; in Wilkins RH, Rengachery SS (editors). Neurosurgery, Volume I. McGraw-Hill, 1990, pp 662-667.
- PANAGOPOULOS KP, EL-AZOUZI M, CHISHOLM HL, JOLESZ FA, BLACK PM: Intracranial epidermoid tumors: A continuous diagnostic challenge. Archives of Neurology 47(7): 813-816, 1990.
- RENGACHARY S, KISHORE PRS, WATANABE I: Intradiploic epidermoid cyst of the occipital bone with torcular obstruction. Journal of Neurosurgery 48(3): 475-478, 1978.
- ROOSEN N, SPRICK CU: Completely reversible, severe acute neurological deterioration with an otherwise asymptomatic, huge intradiploic calvarian epidermal cyst. Surgical Neurology 25: 169-172, 1986.
- RUBIN G, SCIENZA R, PASQUALIN A, ROSTA L, PIAN RD: Craniocerebral epidermoids and dermoids. Acta Neurochirurgia (Wien) 97(1-2): 1-16, 1989.
- RUGE JR, TOMITA T, NAIDICH TP, HAHN YS, MCLONE DG: Scalp and calvarian masses of infants and children. Neurosurgery 22: 1037-1042, 1988.
- RUSSELL DS, RUBENSTEIN LJ: Pathology of tumors of the nervous system; 5th edition. Baltimore, Williams &Wilkins (1989) pgs.693-694.
- SABIN HI, BORDI LT, SYMON L: Epidermoid cysts and cholesterol granulomas centered on the posterior fossa: Twenty years of diagnosis and management. Neurosurgery 21(6): 798-805, 1987.
- SAVADER SJ, MURTACH R, SAVADER BL, MARTINEZ CR: Magnetic resonance imaging of intracranial epidermoid tumours. Clinical Radiology 40(3): 282-285, 1989
- SKANDALAKIS JE, GODWIN JT, MABON RF: Epidermoid cyst of the skull: Report of four cases and review of the literature. Surgery 43: 990-1001, 1958.
- UCHINO A, HASUO K, MATSUMOTO S, UDA K, MORIGUCHI M, NISHIO T, FUKUI M, MASUDA K: Intracranial epidermoid carcinoma: CT and MRI. Neuroradiology 37(2): 155-158, 1995.
- WHITE AK, JENKINS HA, COKER NJ: Intradiploic epidermoid cyst of the sphenoid wing. Archives of Otolaryngology and Head and Neck Surgery 113(9): 995-999, 1987.
- YAMAKAWA K, SHITARA N, GENKA S, MANAKA S, TAKAKURA K: Clinical course and surgical prognosis of 33 cases of intracranial epidermoid tumors. Neurosurgery 24(4): 568-573, 1989.
- YANAI Y, TSUJI R, OSHMORI SW, TAATRA N, KUBOTA S, NAGASHIMA C: Malignant change in an intradiploic epidermoid: Report of a case and review of the literature. Neurosurgery 16(2): 252-256, 1985.
- YAŞARGIL MG, ABERNATHEY CD, SARIOĞLU AÇ: Microneurosurgical treatment of intracranial dermoid and epidermoid tumors. Neurosurgery 24(4): 561-567, 1989.
- ZHOU LF: Intracranial epidermoid tumours: Thirty-seven years of diagnosis and treatment. British Journal of Neurosurgery 4(3): 211-216, 1990.
|
|