
|
|
|
CASE REPORT / CAS CLINIQUE
A CASE OF ISCHAEMIC STROKE FOLLOWING CERASTES CERASTES SNAKE BITE IN LIBYA
UN CAS RARE D’ACCIDENT VASCULAIRE CEREBRAL ISCHEMIQUE APRES MORSURE DE SERPENT CERASTES CERASTES EN LIBYE
E-Mail Contact - OZEN Selin :
selinhassan@hotmail.com
ABSTRACT Background: Cerastes cerastes is a venomous species of viper native to the deserts of northern Africa and parts of the Middle East. Reported cases of ischaemic stroke following a Cerastes cerastes bite are extremely few. Here we describe a case of ischaemic stroke occurring four days after envenomation by C.cerastes. Case presentation: A 26-year-old male was admitted to our rehabilitation unit with a history of ischaemic stroke and right sided hemiplegia. Four months previously he had been bitten by a C.cerastes viper in Libya. Four days after envenomation the patient developed sudden onset of aphasia and right sided weakness. Brain magnetic resonance imaging (MRI) revealed ischaemia in the territory of the left middle cerebral artery. On admission to our hospital, routine blood tests, coagulopathy and vasculitis screening was normal. Colour doppler ultrasound imaging of the carotid and vertebral arteries, MR angiography, transthoracic and transoesophageal echocardiography and Holter electrocardiogram were normal. A daily dose of aspirin 100 mg and physical therapy program was commenced. Conclusion: Only three cases of ischaemic stroke following C.cerastes bite have been reported in the literature. Hypotension, endothelial injury, hypercoagulability and vasculitis have been suggested as possible mechanisms for its occurrence. This probable case of stroke due to envenomation shows that stroke may occur as late as four days after the snake bit and highlights the importance of early administration of antivenom. Patient education on this subject maybe considered an important public health issue in areas of Africa and Asia in which viper bites occur. Keywords: C.cerastes, hemiplegia, ischaemia, snake, stroke, INTRODUCTION Cerastes cerastes, also known as the horned desert viper, is a venomous species of viper native to the deserts of northern Africa and parts of the Middle East which has also been sighted in the Indian subcontinent (9,4). A handful of cases of ischaemic stroke occurring after viper envenomation have been reported in the literature (6,13,15). However, reported cases of ischaemic stroke following a C.cerastes bite are extremely few. Here we describe a case of ischaemic stroke ensuing four days after envenomation which highlights the importance of administering antivenom as soon as possible, even if the patient is initially asymptomatic, in order to reduce the risk of development of rare but significant neurological sequelae. CASE PRESENTATION A twenty-six-year-old male was admitted to our rehabilitation unit with a history of ischaemic stroke and right sided hemiplegia. Four months previously he had been working in a desert in western Libya when he was bitten on the medial aspect of his left foot by a horned desert viper. Four days later, the patient experienced sudden onset of right sided weakness with difficulty in speaking and was admitted to hospital. Brain magnetic resonance imaging (MRI) revealed ischaemia in the territory of the left middle cerebral artery (Figure 1). The patient was treated in the intensive care unit. Details of the patient’s initial investigatory findings and the treatment applied were unobtainable. The patient had no significant past medical history. On admission to our clinic, examination revealed a motor aphasia with a right sided hemiplegia. According to the Brunnstrom recovery stages (3), the motor function of the right upper extremity was stage 2, right hand stage 2 and right lower extremity stage 3. According to the modified Ashworth scale (2), there was grade two spasticity of the right elbow flexors and extensors, grade 1 spasticity of the right finger flexors and grade 2 spasticity of the ankle plantar flexors. The patient was able to walk unaided with right sided foot drop. Routine blood tests were normal. Ferritin, vitamin B12 and homocysteine levels were within the normal range. Coagulation screening including prothrombin time, fibrinogen levels, factor V, VIII, anti thrombin III, protein C and S levels were within the normal range. Active protein C resistance ratio was slightly above the normal limit at 1.24 (normal range 0.8-1.2). The patient had a borderline positive anti-nuclear antibody test (1/100 nucleolar +), and was negative for rheumatoid factor and anti-cyclic citrullinated peptide antibodies. Anti-extractable nuclear antigen antibodies (anti Sjögren syndrome A [Ro], Anti Sjögren syndrome B [La], anti-double stranded deoxyribonucleic acid, anti-Smith, anti-ribonucleoprotein) and human leukocyte antigen B27 surface antigen were also negative. Antineutrophil cytoplasmic antibody (cANCA, pANCA) titres were low and anticardiolipin IgG and IgM antibodies and lupus anticoagulant screening was negative. Following consultation with the Neurology department, colour doppler ultrasound imaging of the carotid and vertebral arteries, echocardiography (echo) and twenty-four hour Holter electrocardiogram were performed, all of which were normal. A transoesophageal echocardiogram was also performed to clearly view the posterior cardiac structures and rule out the presence of a patent foramen ovale. A brain MRI revealed findings consistent with chronic ischaemia in the territory of the left middle cerebral artery (Fig.1). A daily dose of aspirin 100 mg was commenced. The patient commenced a physical therapy program of range of motion, strengthening and stretching exercises alongside robotic gait training. DISCUSSION Taxonomically, C.cerastes belongs to the family of Viperidae and inhabits North Africa from Morocco in the northwest through Libya to Egypt in the northeast and parts of the Arabian Peninsula. Human envenomation by Viperidae resulting in haemorrhagic stroke has been widely described in the literature and is thought to occur due to disturbances in coagulation (1,16). In a study on the incidence of Bothrops Viperidae envenomation and stroke, 2.3% of bitten patients developed haemorrhagic stroke (1). However, in the same study only 0.3% of patients developed ischaemic stroke. Furthermore, only three cases of stroke following C.Cerastes Viperidae envenomation have been reported in the literature (17). Not only is ischaemic stroke following viper envenomation rare, but the onset of stroke is mostly not within the first eight hours of the bite (1). In the patient presented here, ischaemic stroke developed as long as four days after envenomation. Hypotension, endothelial injury, hypercoagulability and vasculitis have been suggested as possible mechanisms for stroke occurrence (14,15), however this topic is still under debate (7,11). In this case, the presence of large vessel infarct is more suggestive of venom induced thrombosis rather than hypotension or vasculitis. Metalloproteinases present in snake venom activate factor X and serine proteases which are prothrombin activators. Snake venom C-type lectins can also have procoagulant properties and may trigger platelet aggregation (5). Despite the onset of stroke occurring after envenomation, we must acknowledge that the detailed investigation into stroke aetiology took place four months’ post stroke. Therefore, despite the normal laboratory findings, coagulopathy and vasculitis following envenomation cannot be ruled out as possible mechanisms for stroke occurrence. In addition, even though the chronology of events suggests that the most likely cause of stroke is envenomation, as the detailed investigatory work up was delayed, and in the absence of cerebral angiography, other stroke aetiologies such as cerebral artery stenosis, transient arrhythmias and meningovasculitis cannot be ruled out (8,18,12). CONCLUSION This probable case of stroke secondary to envenomation highlights that ischaemic stroke may occur even days after a C.cerastes bite in an otherwise healthy individual and underlines the importance of early administration of antivenom. Patient education on this subject maybe considered an important public health issue in areas of Africa and Asia in which vipers and viper bites are rife. Further work into the pathophysiology of stroke onset is necessary in order to develop better drug treatment. Acknowledgment We would like to acknowledge the Baskent University Faculty of Medicine Department of Physical and Rehabilitation Medicine Authors’ consent All authors read and approved the manuscript for publication. Ethıcs approval and consent to partıcıpate Authors’ institution does not require ethical approval for publication of a single case report. Written informed consent was obtained from the patient. Consent for publıcatıon Written informed consent for publication of clinical details and images was obtained from the patient. Competıng ınterests The authors declare that they have no competing interests.
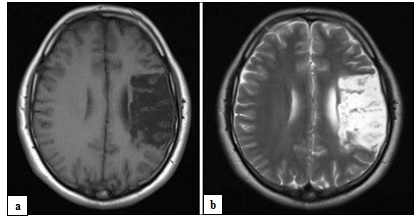 Fig. 1 T1 (a) and T2 (b) weighted magnetic resonance images of the brain showing a chronic infarct in the territory of the left middle cerebral artery REFERENCES
|
© 2002-2018 African Journal of Neurological Sciences.
All rights reserved. Terms of use.
Tous droits réservés. Termes d'Utilisation.
ISSN: 1992-2647