
|
|
|
CASE REPORT / CAS CLINIQUE
A CASE OF POST BEE STING ENCEPHALITIS
ENCÉPHALITE SECONDAIRE A UNE PIQÛRE D'ABEILLE. A PROPOS D'UN CAS
E-Mail Contact - ATTILI Suresh Venkata Satya :
sureshattili@yahoo.com
ABSTRACT Bee Sting in most of the situations is potentially serious. The spectrum of bee sting disease ranges from mild local reaction to death. The literature regarding the bee sting disease from India is sparse. The rare manifestations of the disease include encephalitis, polyneuritis, myocardial infarction, pulmonary edema, bleeding manifestations and renal failure. Here we are reporting a rare case of encephalitis developing 3 days following the bee sting. Key Words: Bee sting, encephalitis, Hymenoptera. Mots Clés : Piqûre d’abeille, Encéphalite, hymenoptère INTRODUCTION The severity and duration of a bee sting reaction can vary from one person to another and at different occurrences in the same individual [1]. These reactions were encountered in only 5% of the patients. Two kinds of reactions are usually associated with bee stings and those of other stinging insects as well: local or systemic. The systemic manifestations are rare and include encephalitis, polyneuritis, bleeding manifestations and renal failure. Here we are discussing a case of encephalitis developing after bee sting. CASE REPORT A 20 year male presented to the emergency department in altered sensorium. The history revealed that he got multiple bee stings while he was working in the field. Following the bee sting he received antihistaminic, and analgesics in the local hospital. The patient remained asymptomatic for the next three days and on the fourth day the attendants noticed irrelevant speech and gradually decreasing level of sensorium. They also noticed continuous rhythmic involuntary movements of the left upper limb. However there was no history of fall, head injury, fever, and prior headache. Systemic review revealed no other positive history. Examination of the patient showed a pulse of 90/ min, blood pressure of 110/70 mm Hg, and patient was afebrile. Nervous system examination showed a Glasgow Coma Scale of 12/15 (E4 V3 M5) bilateral pupils were of normal size and reacting to light. Neck rigidity and kerning’s sign were negative, so as Trousseau’s and Chvostek’s signs and plantar were bilaterally up going. Continuous focal seizures were noted in the left upper limb. Deep tendon reflexes were normal so as the muscle tone. Owing to the mental status rest of the neurological examination was not performed. Investigations revealed hemoglobin, 11gm% Total Leukocyte Count 8000 / mm3 Differential count of N 75, L 25, and platelet count of 2, 80,000 / mm3. Serum chemistry showed sugar 100mg/dl, urea 15 mg/dl, creatinine 0.9 mg/dl, bilurubin of 1.0 mg/dl, SGOT/SGPT 24/18 IU/L, Alkp 110 IU/L, calcium 8.2 mg/dl, Phosphate 3.8 mg/dl, Sodium 140 meq/dl, potassium 4.2 meq/dl. Arterial blood gas analysis was within normal range. His CSF routine microscopy showed 40 cells, sugar of 60 mg/dl with corresponding blood sugar of 100 mg/dl, and protein of 65 mg/dl. MRI of the patient showed a hypo intense lesion on T1 image in the right temporal region which was hyper intense on T2 image and is suggestive of focal encephalitis (fig 1). EEG done after three days was normal. The patient was given methyl prednisalone1 mg/day and phenytoin 100 mg tds. He regained complete consciousness in 12 hours following treatment with complete resolution of all symptoms and signs next 36 hours and was discharged home. DISCUSSION The venom of winged Hymenoptera contains over 30 individual compounds. These include biogenic amines (eg, acetylcholine, dopamine, histamine, norepinephrine, serotonin), polypeptides or protein toxins (eg, apamin, melittin, kinins), and enzymes (eg, hyaluronidase, phospholipases). There fore the bee venom is being used since many centuries in the treatment of various diseases [2]. Though widely studied in western and African countries regarding various allergic reactions of bee sting, the literature from India is sparse and most of the cases were single case reports [7]. Epidemiologists found the peak incidence in months of august and systemic allergic reaction were encountered in only 5% of the patients. Two kinds of reactions are usually associated with bee stings and those of other stinging insects as well: local or systemic. A local reaction is generally characterized by: pain, swelling, redness, itching and a wheal surrounding the wound made by the stinging apparatus, principally type 1 anaphylactic reaction mediated by mast cells. Occurrence of life threatening wheezing, laryngeal edema, or anaphylactic shock in stings, produced by a substance called precipitin. They are considered extremely rare [9]. Arthus type of reaction becomes apparent 8-12 hours after a sting and could persist for two to three days. Serum sickness type of reaction is more likely after an episode of multiple stings (malaise, fever, joint pains, skin rashes, swelling of lymph glands, kidney disturbances) and may develop three to ten days after a sting. Finally, very rare medical disorders such as encephalitis, polyneuritis and renal failure have followed insect stings [3,5]. The life threatening complications of the disease according to Rubenstein et al included atherosclerosis, sepsis, cerebral edema, defibrination syndrome, hemorrhages, emboli and neuro-encephalomyelitis variants [10]. The review regarding various neurological manifestations revealed that several syndromes, presumed to be immune-mediated, are associated with late complications of Hymenoptera envenomation, including Guillain-Barre syndrome, multiple sclerosis, optic neuritis, Parkinsonism, and transverse myelitis [8]. The possible mechanisms of the CNS involvement include, immunologically mediated damage resulting to GB syndrome and various other forms of encephalomyelitis, or the direct affection of the apamin receptors by the venom [4] (n.b. the venom contains apamin, acetyl choline and various other neurotransmitters substances.) In the present case symptoms of hippocampus area involvement are prominent as the concentration of the apamin receptors is more in this region. However the unilateral involvement of the brain parenchyma (right sided encephalitis) could not be explained. Regarding the treatment of the acute episode, antihistaminic along with the analgesics besides the supportive care is enough. But systemic involvement warrants the use of steroids [6]. so we used methyl prednisolone in the present case and the patient responded to therapy very promptly. 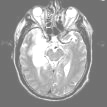 Figure 1 REFERENCES
|
© 2002-2018 African Journal of Neurological Sciences.
All rights reserved. Terms of use.
Tous droits réservés. Termes d'Utilisation.
ISSN: 1992-2647