
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
NEUROEPIDEMIOLOGY / NEUROEPIDEMIOLOGIE
AUDIT OF THE DEMOGRAPHIC PATTERNS OF NEUROSURGICAL CASES IN A TERTIARY HEALTH INSTITUTION: THE NEED TO RELATE SERVICE DELIVERY TO DISEASE PROFILE IN DWINDLING RESOURCES AND MANPOWER SHORTAGE
CONFIGURATIONS DÉMOGRAPHIQUES DES CAS NEUROCHIRURGICAUX DANS UNE INSTITUTION DE SANTÉ TERTIAIRE : NÉCESSITÉ D'ASSOCIER LA PRESTATION AU PROFIL DE LA MALADIE INTEREGRANT LES RESSOURCES ET LE MANQUE DE PERSONNEL
E-Mail Contact - EMEJULU Jude-Kennedy C. :
judekenny2003@yahoo.com
ABSTRACT Objective Methodology Results Conclusion Key Words: Audit, Demographic Patterns, Epidemiology, hydrocephalus, Manpower, Nigeria, road traffic, trauma RESUME Objectif Methodes Resultats Conclusion Mots clés : Epidémiologie, Hydrocéphalie, Nigéria, Traumatologie. INTRODUCTION Nnamdi Azikiwe University Teaching Hospital (NAUTH), Nnewi, Nigeria was formerly a State General Hospital but in December 1988 when it was acquired for medical training by the State University, it became the Anambra State University Teaching Hospital (ASUTECH) under the Anambra State Government. In 1991 however, it was re-named after the 1st President of the Federal Republic of Nigeria, the Rt. Hon. Dr. Nnamdi Azikiwe, and by September 1992, it was upgraded to a facility of the Federal Government and subsequently, joined the ranks of Federal Teaching Hospitals in Nigeria [16]. It is a tertiary health facility that receives referrals from private, primary, secondary and tertiary centres in and around the South East Zone of Nigeria. Nnewi, is located in Nnewi North Local Government Area of Anambra State, one of the five States that make up the South East zone. It is located on the map between latitude 60 11 0” North and longitude 60 551 0”East, and is a sub-urban town with dilapidated internal road networks that necessitate the predominant use of motorcycles as an easier, faster and cheaper mode of intra-city commuting than motor vehicles [5]. It is a sub-urban town populated mainly by civil/public servants, students from the few schools around, road transport operators, and traders of machine parts and house wares, and the town has minimally available recreational facilities. Nigeria, with a population, according to the 2006 national census, of more than 140 million, is composed of 36 States grouped unevenly into six geopolitical zones – South East, South West, South South, North Central, North East and North West. Anambra State has a total population of 4,182,032 (males 2,174,641; females 2,007,391) going by the 2006 National Census. The other four States in the same South East zone are Abia State 2,833,999; Ebonyi State 2,173,501; Enugu State 3,257,298 and Imo State 3,934,899. Our new centre has a potential catchment area spread over some parts of three of the six zones viz. South East (11.7% of Nigeria’s population), South South (15% of the population) and North Central (13.5%) – more than a third of the country’s population. It is a 350-bed tertiary facility that provides services in the various specialties of Medicine, with accreditation for undergraduate training as well as postgraduate medical training in different specialties. Neurosurgical services were commenced for the first time in the institution on 20th April, 2006 and before then, there had not been any formal neurosurgical service in the hospital, neither was neurosurgery taught in its medical school. We do not have facilities for Computerized Tomography (CT) presently, but we use the services of two private centres with the facilities. There is a 7-bed Intensive Care Unit (ICU) in our hospital for the care of critically ill patients. MATERIALS AND METHODS Data collection was done using the Neurosurgery Unit’s admission records and patients’ folders in the hospital over a 30-month period (1st July, 2006 – 31st December, 2008). The data were retrieved using Microsoft Excel broadsheet, and variables collated were age, sex and diagnosis of the patient, date of presentation, source of referral/presentation, date of admission, date of discharge/referral and clinical condition at discharge. Data analysis was done using Epi Info 3.5.1 to determine the distribution of these variables and pattern of neurosurgical patient presentations and admissions, and the findings were then compared with those of other published reports, and some recommendations were made. RESULTS From July 2006 to December 2008, a total of 1255 patients were treated by the Neurosurgery Unit, and 892(71.1%) were males, see figure 1. The age distribution was <1year 162(12.9%), 1-10years 189(15.1%), 11-20years 155(12.4%), 21-30years 254(19.9%), 31-40years 172(13.7%), 41-50years 125(10.0%), 51-60years 88(7.0%] and >60years 110(8.8%), see table 1. The cases that presented through the Accident and Emergency Unit were 799(63.7%), while those that came through the Out-Patient Clinic and other NAUTH units were 456(36.3%). Congenital factors accounted for 206(16.4%), whereas acquired factors were 1049(83.3%), and a breakdown of the latter showed that trauma accounted for 860(82%), neoplasms 81(6.45%), degenerative lesions 76(6.05%) and infections 32(2.55%), see figure 2. Neoplasms were both primary and metastatic; unfortunately, we could not get the histological diagnoses on most of them as they signed for discharge against medical advice, were referred on request to other facilities or absconded from our service after radiologic diagnoses and were not therefore, operated on. Other indications for presentation included acquired hydrocephalus (post-traumatic/ex vacuo) 27(2.2%), microcephaly 11(0.88%), spondylosis 8(0.64%), headache 7(0.56%), craniofacial dysmorphism [Crouzon’s syndrome] 5(0.4%), dementia 2(0.16%), and others, including infections/spinal neoplasms, peripheral neuropathy/neuralgias, etc; accounted for 69[5.5%]. Some patients had more than one disease condition, each. The cases admitted for in-patient treatment were 567(45.2%), out of which 55(4.4%) stayed <1 day on observation, 295(23.5%) stayed 1-7 days, 125(9.96%) 2-4 weeks, 11(0.88%) 1-2 months and 4(0.32%) >3months on admission, whereas 77(13.5%) had unspecified duration/incomplete discharge records, see table 3. The cases treated and discharged to the outpatient clinic without admission in the hospital were 596(47.5%), those referred to other facilities were 43(3.42%) and those that signed to be discharged against medical advice were 41(3.27%); while 8(0.64%) absconded from the hospital. Mortality was 111, representing 13.9% of case admissions or 8.8% of all case presentations viz. deaths from head injury 86(6.85%), spinal injury 10(0.8%), neoplasm 9(0.72%), infections 5(0.40%) and congenital diseases 1(0.12%). Most of them, 72 of 111(64.9%), occurred within 72 hours. DISCUSSION Our new Unit treated all types of neurosurgical diseases both congenital and acquired, though the acquired cases, especially from trauma, were in the majority. It is, therefore, explicable that the young age preponderance in our cases is reflective of the historical pattern of trauma, since most of them are in the 20-40year age group [2,3,5,7,9,13]. This, most likely, explains the male gender preponderance as well, since it is known that trauma is the leading cause of neurosurgical diseases in this gender-age group. Expectedly, more infants presented with congenital diseases than any other age group, whereas neoplasms were most common beyond 60years of age (figure 4). Also, noteworthy is the female preponderance at the extremes of age in all disease conditions including trauma, and in all other disease presentations at all ages, except for trauma (figures 5 and 6). This implies that if trauma is excluded from the disease profile, more females than males would be expected to present with neurosurgical diseases, in our service. Of particular note is the pre-eminence of hydrocephalus over the other diseases including spinal injuries and infections, as the second most common indication for seeking neurosurgical consultation in our centre. In a situation such as ours, in a developing country with trauma as the main indication for presentations, the expectation would be that infections rather than hydrocephalus would closely come after trauma; but this was not the case. A low incidence of infective diseases could be understood as a healthy development if the real reason for this is that the incidence of infective neurosurgical cases is low in our practice, possibly reflecting improving standards of living in our country. However, on the other hand, the question may be asked, whether this curious finding was a result of the indiscriminate use of antibiotics in our environment, non-recognition of such cases by other clinicians as requiring neurosurgical attention, or death of such patients before orthodox medical attention could be sought. In this study, despite the fact that all disease patterns were reflected in the presentations, the 3:1 ratio of trauma against all other disease conditions put together, calls for a more pragmatic and pro-active approach towards the reduction of the burden of trauma in our environment by the relevant organs of government concerned with appropriate and effective policy formulation and implementation. In a 2006 study of the status of Neurosurgery in Nigeria, we reported that there was an appalling ratio of 1 neurosurgeon to 10mllion Nigerians (10,000,000) [6]. Even though this situation has improved marginally in the past 3years, it is still a far cry from the ideal ratio of 1:81,000 reported for North America. Worse still, the Human Poverty Index-1 (HPI-1) value was put at 40.6, ranking Nigeria 76th among 102 developing countries for which the Index had been calculated, and 160th out of 172 countries’ probability of not surviving past the age of 40years [21]. The HPI-1 measures severe deprivation in health by the proportion of people who are not expected to survive age 40 and represents a multi-dimensional alternative to the $1 a day World Health Organization (WHO) poverty measure. It also focuses on the proportion of people below a threshold level in the same dimensions of human development as the Human Development Index – living a long and healthy life, having access to education and a decent standard of living [21]. With these stark realities staring our developing nation in the face, something more realistic than the routine protocols needs to be employed in order to make neurosurgical care more readily available to the greatest number of our population. And the earlier this is employed the better and safer for all concerned. Since trauma is a largely preventable disease, policy makers need to elevate the priority level of safe road use beyond its present rating to make a positive impact on our health care delivery. It gives great hope, looking at previous results from other countries like Italy and United States of America, that if we intensify our efforts towards reducing the incidence of trauma, most of our youths, the most active and productive age group, and the future leaders of our country, would be spared, and of course, our abysmally low average life expectancy of 43.4years could improve for the better [18,20]. Our findings also make a point for the re-prioritization of our service delivery and resource disbursement to pay more focused and effective attention to the patients requiring trauma care whose numbers are massive and prognosis mostly good, and then pay relatively less attention to the less frequently encountered neuro-pathological conditions like neoplasms, craniofacial dysmorphisms, etc. This suggestion does not in the least imply that these other disease conditions should be ignored; rather, that their priority rating in terms of service delivery, in situations where human and material resources for specialist care are severely limited, should be properly re-positioned. Under such circumstances, it may be wiser to install computed tomography facilities in all neurosurgical centres, which would be optimally satisfactory for trauma care, cheaper to maintain and ensure a more equitable distribution, while confining the installation of the more tasking and expensive magnetic resonance imaging to fewer designated centres in order to efficiently re-distribute available scarce resources. We may best be left with the option of referring the rare “once-in-a-while” cases to these designated centres where the incidence rates are higher and service expertise (which usually gets better with regularity of exposure to such cases), would be optimal. This would be the ultimate prelude to sub-specialization by both the neurosurgeons and the neurosurgical centres in our country. Closely related to this is the urgent need to train more neurosurgeons and ancillary paramedical Staff to combat the challenge of trauma in our tertiary health facilities. More neurotrauma specialists, nurses, anaesthetists, intensivists, radiographers and interventionsts should be trained, and also, more trauma units and centres and better ambulance services with efficient communication and response co-ordination should be put in place to ensure the optimum care of these trauma cases and reduction of the mortality rate. Opportunities for fellowship training in neurotrauma should be sought and sponsored in reputable centres round the world to improve the knowledge base and management skills of already trained local neurosurgical personnel in the care of this major but preventable cause of morbidity and mortality. Next to the significance of trauma is the burden of hydrocephalus – unexpectedly the second most common indication for neurosurgical treatment in our centre. Ventriculo-peritoneal shunting and endoscopic third ventriculostomy, which hardware and technical skills are becoming more readily available and affordable nowadays, should be given priority attention in the protocols of new centres in the poor African countries. Unfortunately, this type of advocacy for a comprehensive patient/disease triage can only be efficiently coordinated if a national epidemiological data base is generated from multi-centre studies round the country. This is still lacking in our case, and is evidently long overdue. If this study, like other published local studies, represent the real situation in our country and possibly, in some other developing countries where the available specialist manpower and equipment are grossly inadequate, it would be instructive that in establishing neurosurgical centres, the services should be structured to take cognizance of the local disease profile in order to deliver the optimum benefits to the greatest number of persons. Such structured programmes would also substantially improve the training and dexterity of ancillary health personnel, as well as the skill and experience of the neurosurgical Staff, in appropriate service delivery. CONCLUSION AND RECOMMENDATIONS In South-East Nigeria, trauma – mostly from road traffic accidents, remains the most important indication for neurosurgical consultations, constituting the main workload in our service. The best solution has been proven historically to be prevention, and as such, short and long term preventive measures should be instituted by the government to reduce the burden of road traffic injuries. Presently, there is every need to establish efficient emergency mobile services, education of the public on steps to be taken at accident sites to prevent re-injuries, continuing medical education especially for Staff of the Accident and Emergency Unit and private health facilities where majority of the patients first present, and government facilitation and sponsorship for the training of more neurosurgeons in neurotrauma. Table 1: Age Distribution
Table 2: Diagnoses made on individual cases
Table 3: Duration of Admission
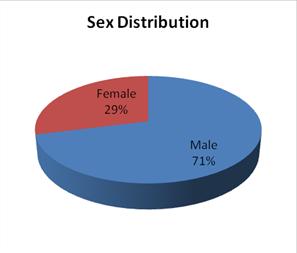 Figure 1 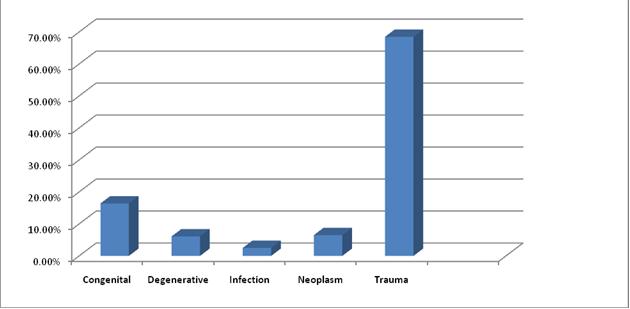 Figure 2 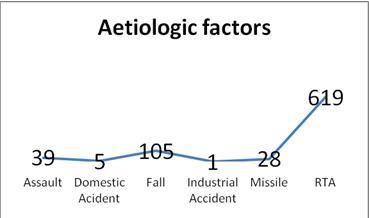 Figure 3 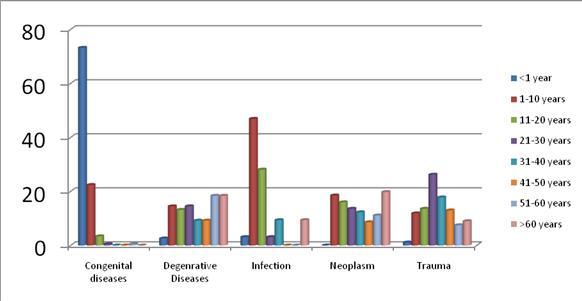 Figure 4 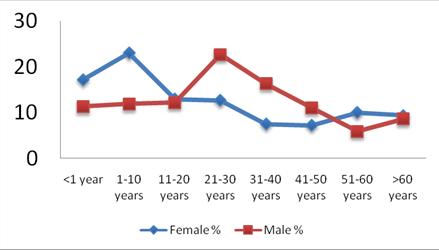 Figure 5 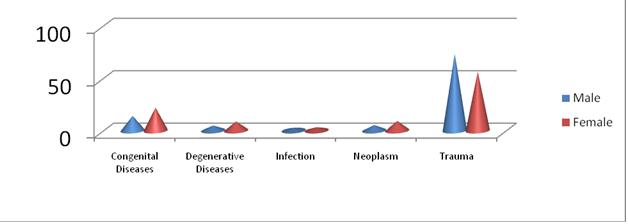 Figure 6 REFERENCES
|
© 2002-2018 African Journal of Neurological Sciences.
All rights reserved. Terms of use.
Tous droits réservés. Termes d'Utilisation.
ISSN: 1992-2647