|
|||||||||||||||||||||||||||||
|
CASE REPORT / CAS CLINIQUE
BILATERAL SUBDURAL HEMATOMA A RARE COMPLICATION OF COMMON PROCEDURE IN 30-YEAR-OLD FEMALE PATIENT: A CASE REPORT AND LITERATURE REVIEW
HEMATOME SOUS DURAL BILATERAL SECONDAIRE A UNE PONCTION LOMBAIRE.
E-Mail Contact - AYELE Biniyam Alemayehu :
biniyam.a7@gmail.com
ABSTRACT Background: Lumbar puncture (LP) is a frequent procedure done for administration of spinal anesthesia or for obtaining cerebrospinal fluid for analysis. The common complications of LP are pain at the local site and post LP headache. Rarely the following complication could occur: infections of central nervous system, brain stem herniation, and subdural hematoma. Post LP hematoma needs to be suspected in those patients whom post LP conservative management failed and headache lasts more than one week. Case presentation: We report a 30-year-old, Ethiopian woman who present with bilateral subdural hematoma following lumbar puncture for spinal anaesthesia. She presented with three weeks history of persistent headache, nausea and vomiting. The symptoms started three days following spinal anaesthesia procedure done for cesarean section. Conclusion: Post-dural puncture headache is the commonest benign complication of lumbar puncture. However, change in character of headache, absence of response to routine measures, development of neurological signs, and persistence of headache beyond one week should prompt physicians to consider rare and fatal complications of post-dural puncture such as subdural hematoma. Moreover, timely diagnosis and management is often associated with good prognosis. Key Words: Lumbar puncture, Spinal anaesthesia, Subdural hematoma, RESUME Introduction: La ponction lombaire (PL) est une procédure fréquente effectuée pour l’administration de l’anesthésie rachidienne ou pour obtenir du liquide céphalo-rachidien pour analyse. Les complications courantes de la PL sont la douleur au site local et la céphalée post PL. Les complications suivantes sont plus rares : infections du système nerveux central, engagement du tronc cérébral et hématome sous-dural. Un hématome post PL doit être suspecté chez les patients dont la prise en charge conservatrice du syndrome post PL a échoué et chez lesquels les maux de tête durent plus d’une semaine. Observation : Nous rapportons le cas d’une femme éthiopienne de 30 ans qui a présenté un hématome sous-dural bilatéral après une ponction lombaire pour une rachianesthésie. Elle avait des antécédents de céphalées persistantes, de nausées et de vomissements pendant trois semaines. Les symptômes ont commencé trois jours après la procédure d’anesthésie rachidienne effectuée pour la césarienne. Conclusion: La céphalée post-PL est la complication bénigne la plus courante de la ponction lombaire. Cependant, la modification du caractère des céphalées, l’absence de réponse aux mesures de routine, le développement de signes neurologiques et la persistance des céphalées au-delà d’une semaine devraient inciter les médecins à envisager des complications rares et mortelles de la PL telles qu’un hématome sous-dural. De plus, un diagnostic et une prise en charge rapides sont souvent associés à un bon pronostic. Mots-clés: Hématome sous-dural, Ponction lombaire, Rachianesthésie.
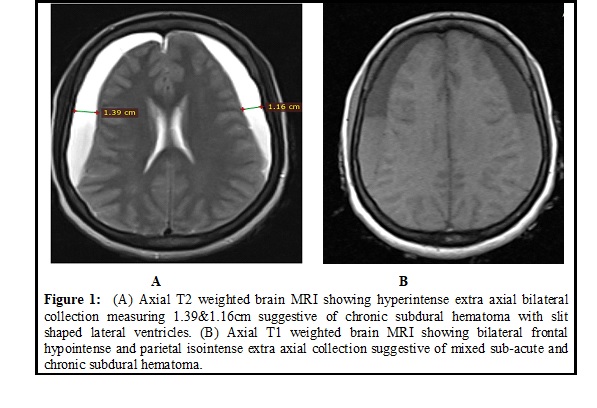
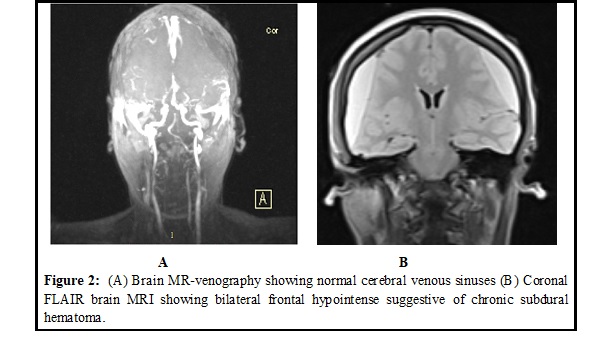
INTRODUCTION Subdural hematoma (SDH) is a common intracranial hemorrhage that is associated with significant morbidity. Moreover bilateral SDH is not uncommon in clinical practice, especially among elderly and diabetics (3). Lumbar puncture (LP) is one of the commonest procedures performed in the clinical practice (2). Post–LP headache is one of the commonest benign complications of LP occurring in 37% (1). Post-dural puncture headaches are often improves within the first one week and characterized by postural headache responsive to conservative treatment such as bed rest and hydration. However, in extremely rare situation, LP may complicate with subdural hematoma (SDH). Post LP subdural hematoma present as post-LP headache but fail to improve within the first one week and often loss its characteristics of postural dependence. To our knowledge, this is the first case of post LP bilateral subdural hematoma from Ethiopia. CASE PRESENTATION We present a 30-year-old female patient from Addis Ababa, Ethiopia. She presented with severe global headache associated with nausea and vomiting of three weeks duration. The headache was non-positional and not responsive to over-counter medications. A week prior to the onset of the headache, she gave birth to a healthy baby by caesarean section (CS) after spinal anesthesia was given. Indication of CS was prolonged labor and prior CS scar. No history of trauma, bleeding disorders, or drug intake. Neurological examination was unremarkable, except for mild neck stiffness. Routine hematological, serological, and coagulation studies were normal. Brain Magnetic Resonance Image (MRI) showed axial T2 and FLAIR weighted hyperintense extra axial bilateral collection measuring 1.39 cm and 1.16 cm suggestive of chronic subdural hematoma with slit shaped lateral ventricles. On axial T1 weighted, brain MRI showed bilateral frontal hypointense and parietal isointense extra axial collection suggestive of mixed sub-acute and chronic subdural hematoma (Figure 1A, 1B & 2B). Brains MR-venography (MRV) study was normal (Figure 2A). After neurosurgical consultation, bilateral bur-hole was done and hematoma drainage was done for bilateral subdural hematoma. On her third post operation day, the patient was discharged home improved. DISCUSSION Rarely, LP can resulted in subdural hematoma. Subdural heamatoma can be unilateral or bilateral (8). We present a young female patient who undergone LP to deliver spinal anesthesia before her CS, latter developed persistent and severe headache which lasted for three weeks before she presented to our facility. Persistence and non-responsive nature of patient’s headache alert us to think of SDH (8,9). Lumbar puncture for spinal anesthesia is a routine practice with rare serious complications. Post lumbar puncture subdural hematoma has been shown to be common in obstetric population. An incidence of intracranial subdural hematoma is 1 in 500,000 obstetric procedures (9). Typical patients with post-dural puncture headache present with postural headache that respond to conservative measures like bed rest, adequate hydration and simple analgesics. Change in character of the headache, development of neurological signs like decline in level of consciousness, diplopia, vomiting and body weakness should prompt physicians to look for other differential diagnosis (5). In puerpurium, the diffrentials could be cerebral vein thrombosis, eclampsia and meningitis, which needs brain scanning and other workups. Treatment of post lumbar puncture subdural hematoma depends on symptom severity, size of hematoma and its mass effect. For hematomas >10 mm in size, midline shift >5 mm and severe neurologic manifestations, surgery should be considered. In majority of the case SDH occurs unilaterally. However, occationally bilateral subdural hematoma may occur among individuals with traumatic brain injury and may occationally complicate neurosurgical procedures. The overall incidence of bilateral SDH has been reported to be between 16% and 20% (3). Upon Pubmed search for reported cases with bilateral sub-dural hematoma following LP, we only found three cases. All the three cases were females (Table 1). However, contrary to our case, the indication of LP in the three cases was to deliver epidural analgesia for control of labor pain. Furthermore, all the cases we found from literature search were managed by conservative medical management including adjuvant corticosteroid, because of minimal hematoma size and headache (4,6,7). However, our patient suffered severe and persistent global headache which is not reponsive to conservative management. In addition the size of bilateral SDH was large compared to all those reported cases of bilateral SDH following LP (Figure 1A & 1B). To our knowledge, this is the first case to be reported from Ethiopia. CONCLUSION Post-dural puncture headache is the commonest benign complication of lumbar puncture. However, change in character of headache, absence of response to routine measures, development of neurological signs, and persisitence of headache beyong one week should prompt physicians to consider rare and fatal complications of post-dural puncture such as subdural hematoma. Moreover, timely diagnosis and management is often asscoited with good prognosis. DECLARATIONS: Ethics approval and consent to participate: The authors’ institution does not require ethical approval for the publication of a single case report. Consent to participate: Written informed consent was obtained from the patient. Availability of data and materials: All data sets on which the conclusions of the case report based to be available as spreadsheets documents and available from the corresponding author on reasonable request from the editors. Competing interests: The authors declare that they have no competing interests. Funding: No funding was received from any organization or individuals.
TABLES AND FIGURES Table 1: Literature review of cases with bilateral subdural hematoma complicating LP
REFERENCES:
|
© 2002-2018 African Journal of Neurological Sciences.
All rights reserved. Terms of use.
Tous droits réservés. Termes d'Utilisation.
ISSN: 1992-2647