
|
|
|
CASE REPORT / CAS CLINIQUE
BROWN TUMOR OF LUMBAR SPINE IN PATIENT WITH CHRONIC RENAL FAILURE
LOCALISATION LOMBAIRE D'UNE TUMEUR BRUNE DANS L'INSUFFISANCE RENALE CHRONIQUE
E-Mail Contact - BERTAL Abderrazzak :
abbertal@yahoo.fr
ABSRACT Brown tumors are erosive bone lesions caused by increased osteoclastic activity. They usually occur in the severe forms of secondary hyperparathyroidism, as in patients with hemodialysis-dependent chronic renal disease. Involvement of the lumbar spine with this tumor causing neural compression is extremely rare. We report a 49-year-old man, who had been on haemodialysis for CRF for over 15 years, presented with leg weakness and back pain over the thoracolumbar junction. There were no motor or sensory disturbances. Spinal MRI revealed osteolytic lesions of the ribs and lumbar vertebrae L1. The clinical and radiological abnormalities resolved after parathyroidectomy and spine surgery. Key-words: Brown tumor, hyperparathyroidism, lumbar spine, osteoclastomas, parathyroidectomy. INTRODUCTION Brown tumors or osteoclastomas are benign lesions of the bone, representing a reparative cellular process secondary of an hyperparathyroidism induced osteoclastic activity [1]. In patients with hemodialysis-dependent chronic renal disease, these lesions occur in the severe forms of secondary hyperparathyroidism. It occur commonly in the pelvis, ribs, clavicles and extremities, involvement in the spine is exceedingly rare [5]. The authors report a case of a 49 year-old man, submitted to a long period of hemodialysis, and who presented with a brown tumor of the lumbar spine, treated successfully. CASE REPORT A 49-year old man with a 15-year history of periodic hemodialysis-dependent chronic renal failure of unknown cause. He was referred to our department of neurosurgery for a back pain and a progressive bilateral lower-extremity weakness. On physical examination, there was mild tenderness over his lumbar spine. There were no motor or sensory disturbances, muscle tone was normal. Deep tendon reflexes and plantar responses were flexor, and sphincter tone was normal. Laboratory results demonstrated that serum levels were remarkable for creatinine of 12 mg/dl (normal range 0.6-1.2 mg/dl), for calcium of 11 mg/dl (normal range 8.6-10.5 mg/dl) and for PTH level of 1200 pg/ml. Plain radiographs and spinal MRI revealed osteolytic lesion of L1 lumbar vertebrae, causing the spinal cord compression (fig 1). The preoperative differential diagnosis included a metastatic tumor and a spinal tuberculosis. DISCUSSION Brown tumors (BTs) or osteoclastomas also named osteitis fibrosa cystic are benign lesions of the bones. They correspond to a reparative cellular process secondary to an hyperparathyroidism-induced osteoclastic activity [1]. Bone defects are filled with fibroelastic tissue, which deforms the bone and simulates a neoplasm [9]. BTs arise as complications of a primary (3-7%) or a secondary hyperparathyroidism (1-2%), and the latter is a well-recognized complication in patients with end-stage renal failure, resulting in renal osteodystrophy including osteosclerosis, brown tumor and osteomalacia [8]. On neuroimaging, BTs realize lytic lesions that stimulate a little reactive bone formation, eventually misleading the diagnosis, especially when the lesions are multiples like in a secondary malignant tumor, amyloidosis, giant cell tumor [1,7,8] and spinal tuberculosis, which is still common in Morocco. Magnetic resonance imaging is very helpful in the accurate evaluation of the location and the extent of the tumor, exhibiting a low signal intensity on T1 and T2 weighted images, with foci of increased intensity corresponding to spots of hemorrhage [3,7]. However there is no specific image characteristics described for spinal BTs. Laboratory findings in patients with brown tumor include elevated serum levels of calcium and alkaline phosphatase and low serum levels of phosphate. The concentration of parathyroid hormone in serum is elevated. CONCLUSION In conclusion, BTs represent a reparative cellular process rather than a neoplastic process. Spine localisation, although rare, should be considered in the differential diagnosis of spinal lesions. Serum phosphate, calcium and PTH levels should be included in routine survey for multiple osteolytic lesions especially in patient with chronic renal failure. BTs can be resolves after parathyroidectomy, however surgical resection and stabilisation of spine may be needed to preserve neurologic function. 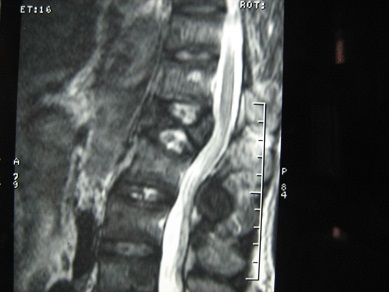 Figure 1 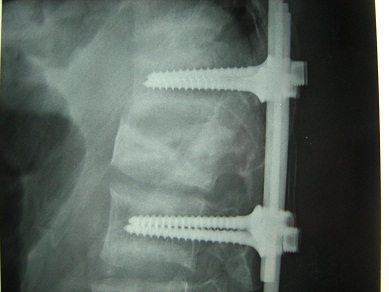 Figure 2 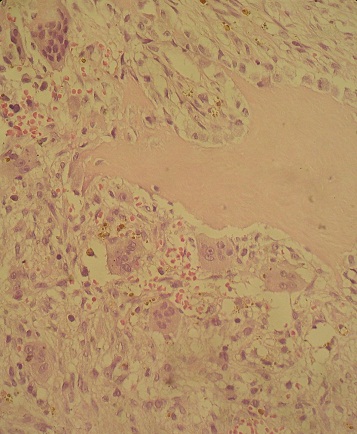 Figure 3 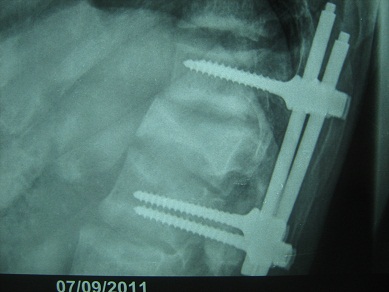 Figure 4 REFERENCES
|
© 2002-2018 African Journal of Neurological Sciences.
All rights reserved. Terms of use.
Tous droits réservés. Termes d'Utilisation.
ISSN: 1992-2647