
|
|||
|
CASE REPORT / CAS CLINIQUE
BUTTERFLY VERTEBRA DIFFERENT CLINICAL PRESENTATION
VERTÈBRE EN PAPILLON. PRÉSENTATIONS CLINIQUES
LAYAS A.
2
E-Mail Contact - ZEGLAM Adel M. :
zeglama@yahoo.com
ABSTRACT Butterfly vertebra is a very rare anomaly, but can be associated with disabling disorders. Diagnosis is sometimes difficult if complete history and neurological examination were not undertaken, as illustrated by these two reports; a girl aged 2 years 6 months, who was referred from the Orthopaedic department with a history of frequent tripping over and weak left leg since birth. Clinical examination revealed a monop aresis of the left leg, aterial-septal defect (ostium secundum type), pulmonary stenosis and deformed thoracic cage. The second case is of a man aged 54 years who has been suffering from low back pain since early adolescence. He now has polyarthropathies which were investigated and found to be due to early onset osteoarthritis.Surprisingly no degenerative changes were found at the level of the butterfly vertebra. The literature is reviewed regarding butterfly vertebra associated with diastematomyelia, aterial-septal defect; pulmonary stenosis and osteoarthritis.There are no reports of such associations. We believe that in a patient with a butterfly vertebra and a clinical picture of dysraphism, investigations are indicated, mostly because of the differences in the clinical presentation. RESUME La vertèbre en » papillon » est une anomalie très rare qui peut s’associer à divers handicaps. Le diagnostic est parfois difficile à porter car l’histoire clinique et l’examen neurologique sont mal appréhendés. Nous rapportons 2 cas : une fille âgée de 2 ans et 6 mois et un homme âgé de 54 ans. La littérature est revue. INTRODUCTION Butterfly vertebra is a very rare anomaly, but can be associated with disabling disorders. Diagnosis is sometimes difficult if complete history and neurological examination were not undertaken, as illustrated by these two reports; CASE REPORT 1 A 2 years and 6 months girl presented to the Paediatric Consultant Clinic having been referred from the Orthopaedic Clinic with a history of frequent tripping over and weak left leg since birth.  Picture 1 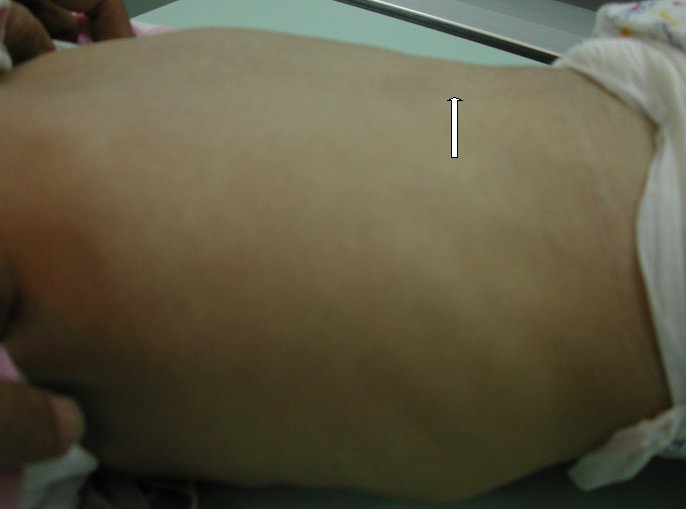 Picture 2 Plain x-ray spine showed Butterfly vertebra (T12) .MRI of dorsolumber spine reports (radiologist’s report) “T12 butterfly vertebra.TheT11and L1 vertebrae are seen to project into the central T12 defect. There is diastematomyelia with the cord splitting into two near equal hemi-cords at around T11 level and reuniting at L3 level. There is an anteroposterior bony septum at L1 level splitting the lumber canal into near equal halves.L1spinous process is bifid. The cord is low lying and tethered at S1level.Lipoma of filum terminale is seen. There is lumber dural ectasia. The central cord is prominent at T8 to T10 level. No interspinal or pre/paravertebral collection is seen” (see figures 1-10).  Figure 1  Figure 2  Figure 3 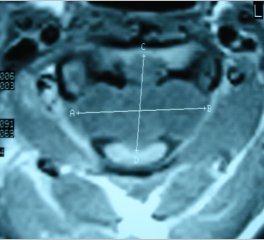 Figure 4 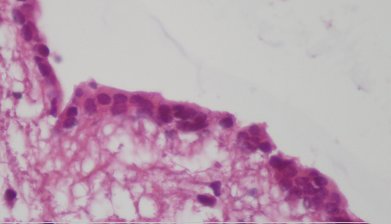 Figure 5 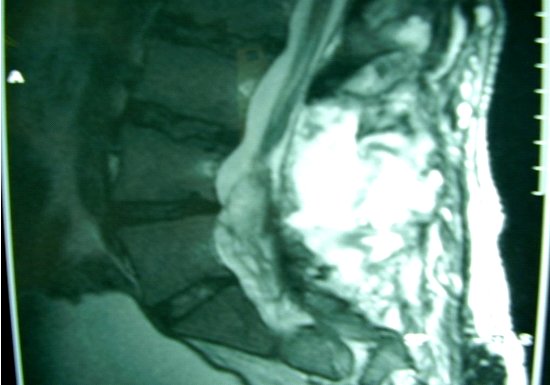 Figure 6 Figure 1, 2, 3, 4, 5, 6: butterfly vertebra at T12.Diastematomylia T11-L3.Tethered cord S1 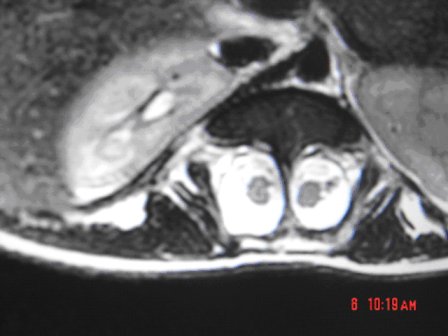 Figure 7 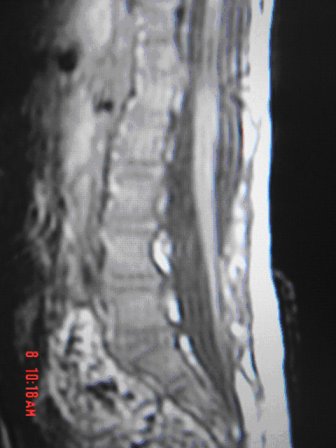 Figure 8 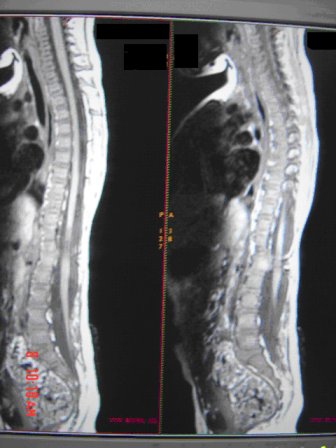 Figure 9 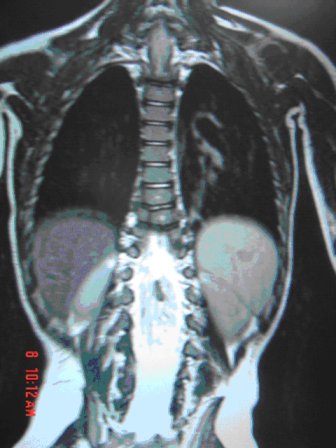 Figure 10 Figure 7, 8, 9, and 10: enlargement and malformation of the canal due to ductal ectasia All of her haematological tests were normal including liver function tests. Echocardiogram revealed a small ASD (ostium secundum type), of 14.4 mm and moderate pulmonary stenosis with a peak gradient of 32 mmHg. CASE REPORT 2 A 54 year old Libyan male; University teacher has been suffering from low back pain since early adolesensce .His back pain is exacerbated by standing for long time and unlike other common causes of backache it is particularly eased by forward bending .His low back pain does not radiate to lower limbs. He is otherwise perfectly well and his general as well as his neurological examinations was unremarkable. He was found to have butterfly vertebra when he was investigated for polyarthropathy in the early seventies .It was confirmed that his arthropathies were due to early onset osteoarthritis. No degenerative changes were found at the level of the butterfly and the adjacent areas. The clinical picture is typical for lumbar stenosis (bending forward). The stenosis apparently between L5/S1 and the level of the butterfly vertebra is at L4. (See figure 11 – 13)  Figure 11 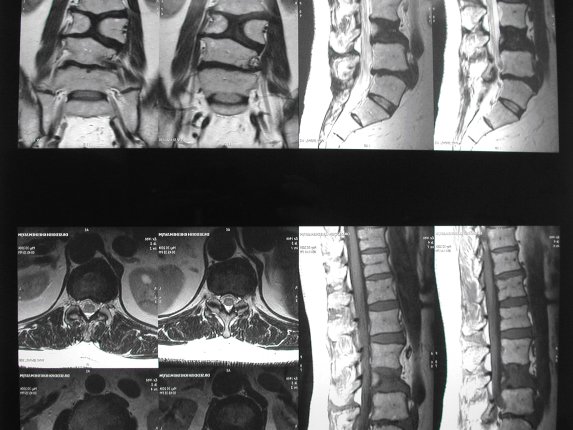 Figure 12 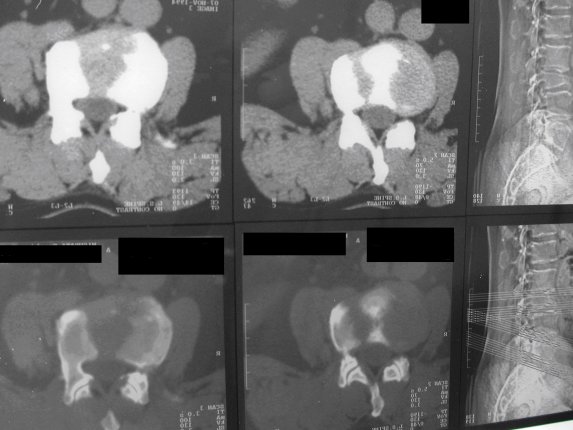 Figure 13 DISCUSSION Butterfly vertebra is a rare malformation of the spine. Probably first described in 1844 in the 12th thoracic vertebra of a 55-year-old adult by Rokitansky (1850). It is classified as a congenital developmental anomaly in the early embryonic period resulting in a variety of vertebral body malformation. (1,2,3,4,5,6,7) Ruge.Wilts 1977; O’Rahilly et al 1983; Mann & Murphy 1990). Butterfly Vertebra usually occurs in the lumber and thoracic spine and males are generally more affected than females (2) Barnes 1994; Aufdenhide & Rodriguez-Martin 1998). The butterfly malformation may involve two adjacent vertebral bodies, but the neural arches of the affected vertebrae are usually intact. The two halves of the vertebral body are generally equal in size, but hypoplasia of one or both halves sometimes occure. Moreover, they may be displaced laterally or wedged anteriorly, so that butterfly vertebra can result in Kyphosis or scoliosis due to the diminished height of anterioly-wedged vertebral body. In these cases affected subjects are likely to have back pain after heavy lifting or carrying as suggested by Fisher & Vandemark (1945) Epstein (1955) and Barns (1994). Midline spinal cord/vertebral skeletal defects, termed spinal dysraphism result from defective closure of the caudal neural tube. Abnormal neural tube closure beginning early in the embryologic sequence produces dysraphism states which involve both neural and skeletal elements (myelomeningocele), while late-occurring closure defects produce congenital anomalies restricted to the posterior elements of the vertebrae (spina bifida occulta). Occult spinal dysraphism is a defect of intermediate severity in which vertebral anomalies are associated with underlying intraspinal pathology or developmental abnormalities, such as a hairy patch, skin tag, port-wine stain, haemangioma, and subcutaneous lipoma or sinus tract. Common intraspinal lesions include dermoid tumours, intraspinal lipomas and diastematomyelia. While some patients with occult spinal dysraphism may show signs of neurological dysfunction and talips equinovarus from birth, most develop symptoms insidiously at around 3 years of age, but many do not develop problems until school age or adolescence. Tethered Cord Syndrome consists of low conus medullaris resulting from an intradural lipoma, a diastematomyelia, or adhesion, shortening, or thickening of the filum terminale. As a result, nerve roots; cauda equine and conus are adhered to the dura. Cutaneous signs are lacking in 50% of the cases. Signs and symptoms are variable depending on the complexity of the abnormalities. These can present in early infancy or become manifest in early childhood. The clinical syndrome includes low back pain, scoliosis, tiptoe walking, foot deformities, bladder dysfunction, lower extremity weakness and muscle atrophy. Objective finding may consist of decreased tone and deep tendon reflexes in lower extremities, patchy decrease in sensation, deepening of the arch and contractures of the toes. The presentation of the two patients is clearly different. One is a child and has a clinical picture strongly suggestive of dysraphism. The constellation of radiological findings is clearly malformative, and the butterfly vertebra is only part of it. In this young girl no cutaneous lesions were seen and because she has not been toilet trained yet, it was very difficult to make any comments on her renal functions although her blood and urine tests were normal. We were not able to find any association between butterfly vertebra, spinal dysraphism, heart lesions and thoracic cage deformity in any of the literatures that we have revised. The second patient has an acquired spinal stenosis, and the butterfly vertebra is an incidental finding and although the patient has osteoarthritic changes no degenerative changes were found at the level of the butterfly vertebra. We believe that in a patient with a butterfly vertebra and a clinical picture of dysraphism, investigations are indicated, mostly because of the clinical picture. When the butterfly vertebra is isolated radiological investigations are not needed.
REFERENCES
|
© 2002-2018 African Journal of Neurological Sciences.
All rights reserved. Terms of use.
Tous droits réservés. Termes d'Utilisation.
ISSN: 1992-2647