CASE REPORT / CAS CLINIQUE
CEREBELLAR HAEMANGIOBLASTOMA IN PREGNANCY: A REPORT OF 2 CASES SUGGESTING ACCELERATED GROWTH
LES HEMANGIOBLASTOMES CEREBELLEUX : A PROPOS DE 2 CAS SUGGERANT UNE ACCELERATION DE LEUR DEVELOPPEMENT DURANT LA GROSSESSE
- Division of Neurosurgery, Groote Schuur Hospital, University of Cape Town, South Africa
E-Mail Contact - CARTER David B. :
ABSTRACT
Haemangioblastoma is a relatively uncommon vascular tumour, usually occurring in the cerebellum. Twenty-eight cases of cerebellar haemangioblastoma in pregnancy have previously been described in the literature. It has been suggested that the hormonal and vascular changes of pregnancy have been associated with accelerated growth and symptomatology. We present two patients with haemangioblastoma, whose growth and vascularity during pregnancy support this view.
Keywords: Africa, Haemangioblastoma, Pregnancy, Posterior fossa tumour
RESUME
Les hémangioblastomes sont des tumeurs relativement peu fréquentes, intéressant le cervelet. La littérature fait état de vingt-huit cas d’hémangioblastomes apparus durant la grossesse. Il a été suggéré que l’accélération de leur développement et de la symptomatologie étaient liées aux changements hormonaux et vasculaires associés à la grossesse. Nous rapportons deux cas de patientes atteintes d’hémangioblastome dont le développement et la vascularisation durant la grossesse corroborent ce point de vue.
Mots clés : Afrique, Hémangioblastome, Grossesse, Tumeur de la fosse postérieure
INTRODUCTION
Haemangioblastomas are relatively rare primary vascular tumours, typically occurring in the cerebellum of adults. They are histologically benign lesions consisting of lipid-laden stromal cells within a well-defined capillary network. They may be solid or cystic and are often very vascular. They occur sporadically or as part of von Hippel-Lindau disease (VHL). We were only able to find twenty-five cases occurring in pregnancy, described in the literature (1-14), and consequently it has been difficult to draw conclusions regarding their relationship to pregnancy. We describe two cases of cerebellar haemangioblastomas that presented in pregnancy, which support the theory that pregnancy may indeed accelerate tumour growth.
CASE REPORTS
Case 1: A 22 year old woman presented in the twenty ninth week of her second pregnancy. She complained of three days of worsening ataxia and headache. Throughout her pregnancy, she had been experiencing daily nausea and vomiting. In addition, her right arm had weakened over the prior two months.
On examination, she had bilateral papilloedema, and right arm weakness, as well as left cerebellar signs. A CT scan of the brain demonstrated a mixed solid/ cystic, contrast enhancing midline posterior fossa mass, causing obstruction of the fourth ventricle and hydrocephalus.
An external ventricular drain was inserted on the day of admission, followed two days later with a posterior fossa craniectomy and resection of the tumour. At operation, the tumour was found to be extremely vascular, with the patient requiring a transfusion of seven units of packed red cells during the six-hour procedure. The tumour was completely resected, and histologically confirmed to be a haemangioblastoma. The patient had an uneventful postoperative course, with the external drain being removed thirteen days after insertion. She was reviewed clinically for evidence of Von Hippel-Lindau disease, and it was determined that this was a sporadic haemangioblastoma. She is at present awaiting an elective caesarean section, scheduled for her thirty eighth week of pregnancy.
Case 2: A 23 year old woman presented in her thirtieth week of her second pregnancy. She complained of a week of worsening ataxia and diplopia, associated with headache, nausea and vomiting for three weeks. Examination revealed bilateral papilloedema, a left abducens nerve palsy, and mild cerebellar signs in the left lower limb. CT scan of the brain showed a contrast enhancing midline posterior fossa mass, with both cystic and solid components, and associated hydrocephalus.(Fig.1) Again, clinical workup showed that this was a sporadic haemangioblastoma.
The patient’s management was similar, with the insertion of an external ventricular drain, followed two days later by a posterior fossa craniectomy.
At surgery, the tumour was again noted to be extremely vascular, with the procedure taking six and a half hours, and the patient needing four units of packed red cells peri-operatively. The tumour was completely resected and confirmed to be a haemangioblastoma.
The patient had an uncomplicated postoperative course, with the drain being removed seven days after insertion. She went on to deliver a healthy infant.
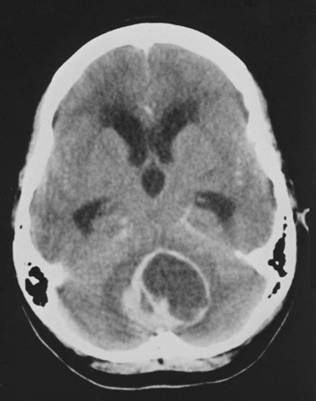
Figure One
DISCUSSION
The effect of pregnancy on the natural history of brain tumours is unclear. Cushing and Bailey stated that pregnancy was a provocative factor for angiomatous tumours, but they were not able to prove this with their data (3). Roelvink et al (12) in their review of the effect of pregnancy on the manifestation or acceleration of symptoms of brain and spinal tumours in pregnancy found that the incidence of brain tumours that become symptomatic in pregnancy is not more than that in age matched women and the frequency of different primary tumours is not changed by pregnancy. However they found that different types of tumours are influenced at different stages of pregnancy (1). With the possible exception of Robinson’s series (11), haemangioblastomas are probably not over-represented among all pregnant women presenting with brain tumours (2). There is therefore no evidence that there is an increased incidence of haemangioblastomas in pregnancy. In VHL disease, it is classic that pregnancy can be accompanied by the enlargement of a cyst in a few months, sometimes leading to dramatic complications both for the mother and the fetus (10). A number of authors have however observed that there appears to be acceleration in the rate of growth and subsequently development of symptoms of haemangioblastoma in pregnancy (2-9). The expansion of the tumour’s vascular bed and the maternal blood volume, as well as hormonal influences have been used to explain the rapid progression in pregnancy (2, 3, 4, 7,13, 14). There appears to be an equal presentation of haemangioblastomas in the first and third trimesters of pregnancy (7). One can speculate that in those patients presenting in the first trimester the tumour has already attained a critical size and then rapidly becomes symptomatic due to the vascular engorgement or hormonal influences on the tumour itself (7). The postulated role of hormonal factors was further strengthened by the demonstration of progesterone receptors in haemangioblastomas by Brown et al.(2) In addition, the intravascular volume reaches its maximum in the third trimester; this would explain the development of symptoms and rapid tumour growth due to engorgement in this period. Both of our patients presented in the third trimester with a rapid progression of symptoms, supporting the hypothesis that increased intravascular volume contributed to the engorgement and enlargement of the haemangioblastomas.
Haemangioblastomas are normally highly vascular tumours and can bleed profusely at surgery. Logically, a vascular tumour could be expected to increase its vascularity due to the vascular engorgement associated with pregnancy. Both of our patients had more profuse bleeding at surgery than expected, requiring significant transfusions. It is our opinion that this increased vascularity of pregnancy not only results in accelerated tumour enlargement, but adds the additional risk of intra-operative bleeding to this surgery and that both surgeon and anaesthetist should be cognoscent of this in their preoperative planning.
REFERENCES
- BOKER A, ONG BY, Anaesthesia for caesarian section and posterior fossa craniotomy in a patient with von Hippel- Lindau disease. Can. J. Anaesth. 2001; 48(4):387-90.
- BROWN DF, DABABO MA, HLADIK CL, EAGAN KP, WHITE CL, RUSHING EJ. Hormone receptor immunoreactivity in haemangioblastomas and clear cell renal carcinomas. Mod. Pathol. 1998;11(1);55-9.
- CUSHING H, BAILEY P. Tumours arising from the Blood Vessels of the Brain: Angiomatous Malformations and Haemangioblastomas. Springfield IL, Charles C Thomas, 1928.
- DELISLE MF, VALIMOHAMED F, MONEY D, DOUGLAS MJ, Central Nervous system complications of von Hippel – Lindau disease and pregnancy; perinatal considerations: case report and literature review. J. Matern. Fetal Med. 2000;9(4):242-7.
- DEMIRARAN Y, OZGON M, UTKU T, BOZKURT P. Epidural anaesthesia for Caesarian section in a patient with von Hippel-Lindau disease. Eur. J. Anaesthesiol. 2001;18(5):330-2.
- GRIMBERT P, CHAVEAU D, REMY SR, GRUNFELD JP. Pregnancy in von Hippel-Lindau disease. Am. J. Obstet.Gynecol. 1999; 180: 110 – 111.
- KASARKIS EJ, TIBBS PA, LEE C. Cerebellar Haemangioblastoma Symptomatic during pregnancy. Neurosurg 1988; 22:770-772.
- LECHOWSKI S, NIESPODZIANSKI K, DOMAGALA S. [Surgery of brain angioma (haemangioblastoma cerebelli) during the 31st week of Pregnancy]. Ginekol Pol 1992; 63(8)424-7.
- NATHAN L, SATIN AJ, TWICKLER DM. Cerebellar haemangioblastoma complicating pregnancy. J Reprod Med 1995; 40:662-664.
- RICHARD S, DAVID P, MARSOT-DUPUCH K, GIRAUD S, BEROUD C, RESCHE F. Central nervous system hemangioblastomas, endolymphatic sac tumors, and von Hippel-Lindau disease. Neurosurg Rev 2000, 23:1-22.
- ROBINSON RG. Aspects of the natural nistory of cerebellar haemangioblastomas. Acta Neurol Scandinav 1965; 41:372-380.
- ROELVINK NC, KAMPHORST W, VAN ALPHEN HA, RAO BR. Pregnancy-Related Primary brain and Spinal Tumours. Arch Neurol 1987; 44:209-215.
- ROMANSKY K, ARNAUDOVA V, NACHEV S. Haemangioblastoma during Pregnancy. Zentralblatt fur Neurochirugie 1992; 53(1): 37-39.
- TEKKOK IH, ACIKGOZ B, SAGLAM S, ONOL B. Vertebral haemangioma symptomatic during Pregnancy- Report of a case and Review of the Literature. Neurosurg 1993; 32:302-306.