CLINICAL STUDIES / ETUDES CLINIQUES
CEREBRAL VENOUS THROMBOSIS. RETROSPECTIVE STUDY OF 30 CASES
THROMBOSE VEINEUSE CEREBRALE. ETUDE RETROSPECTIVE DE 30 CAS.
- Service de Neurologie, CHU Hassan II, Fès, Maroc
ABSTRACT
Background
The Cerebral venous thrombosis (CVT) is a rare origin of stroke. However, the clinical presentation and etiologies are various. The prognosis is better than arterial thrombosis. Magnetic resonance imaging (MRI) and MR Venography (MRV) are currently the key diagnostic.
Methods
We studied 30 cases collected in the department of neurology of the university hospital of Fez (Morocco). This study was conducted between January 2003 and October 2007 and lasted 58 months. The cerebral CT-scan was performed in 27 cases (90%) while the MRI examination was done in 18 patients (67%); and most patients (90%) received anticoagulant therapy.
Results
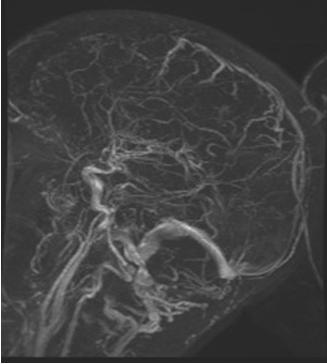
The mean age of our patients was of 29 years old, ranging between 18 days old and 65 years old. Predominance of female was noticed (70%). The clinical presentation of patients was dominated by the following profiles: headache in 24 cases (80%), motor and sensory disability in 15 cases (50%), seizures in 10 cases (33%), and consciousness disorder in 10 cases (33%).
CVT was associated to post-partum in 10 cases (33%), infectious origin in 8 cases (26%), Behcet disease in 2 cases (7%), pulmonary carcinoma in one case, thrombocytemia in one case and idiopathic in 7 cases (23%).
The evolution was good in 20 cases (67%), minor squealaes were observed in 6 patients (20%), while major squealaes were observed in 2 cases and death of 2 cases was also registered.
Conclusion
The CVT is pathology of good prognosis once the diagnosis is promptly performed and early heparin treatment initiated.
Key Words: Cerebral venous thrombosis, Heparin, Angio-MR
RESUME
Introduction
La thrombose veineuse cérébrale (TVC) est une cause rare d’accident vasculaire cérébral (AVC). La présentation clinique et les étiologies sont variées. Le pronostic est meilleur que la thrombose d’origine artérielle. L’imagerie par résonance magnétique (IRM) et la venographie par résonance magnétique (VRM) sont actuellement les moyens de choix pour poser le diagnostic.
Méthodes
Nous avons étudié 30 cas colligés au service de neurologie de l’hôpital universitaire de Fès (Maroc). Cette étude a été réalisée entre Janvier 2003 et Octobre 2007 et a duré 58 mois. Le scanner cérébral a été réalisé dans 27 cas (90%) tandis que l’examen par IRM cérébrale a été réalisé chez 18 patients (67%). La plupart des patients (90%) ont reçu un traitement anticoagulant à dose curative.
Résultats
L’âge moyen de nos patients était de 29 ans, variant entre 18 jours et 65 ans ; avec une nette prédominance féminine (70%). La présentation clinique des patients a été dominée par les profils suivants: des céphalées dans 24 cas (80%), un déficit sensitivomoteur dans 15 cas (50%), des crises épileptiques dans 10 cas (33%) et des troubles de la conscience dans 10 cas (33 %).
La TVC a été due au post-partum dans 10 cas (33%), une infection dans 8 cas (26%), une maladie de Behçet dans 2 cas (7%), un cancers pulmonaire dans un cas, une thrombocytémie dans un cas. La TVC est restée idiopathique dans 7 cas (23%).
L’évolution a été favorable dans 20 cas (67%). Des séquelles mineures ont été observées chez 6 patients (20%), tandis que des séquelles majeures n’ont été observées dans 2 cas. Deux cas de décès ont été enregistrés.
Conclusion
La TVC est une pathologie de pronostic favorable si le diagnostic est effectué rapidement et un traitement par héparine est démarré précocement.
Mots clés: thrombose veineuse cérébrale, Héparine, angio-IRM
INTRODUCTION
The CVT is a rare origin of stroke. This pathology was considered as an infectious disease for a long period. In addition, it was assumed that it affects the superior sagittal sinus leading to death. Anticoagulants were contraindicated while the diagnosis was performed at the autopsy stage. Actually CVT is a disease with various clinical presentation and etiologies. MRI and MRV are the key diagnostic tools. Heparin is the first-line treatment. The prognosis is better than arterial thrombosis with mortality rate well below 10%.
The purpose of the current study is to describe and discuss different features of this pathology including frequency, clinical model, diagnosis and outcome in Morocco.
PATIENTS AND METHODS
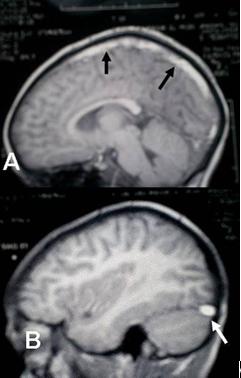
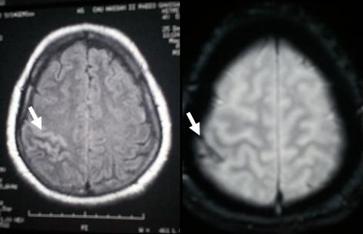
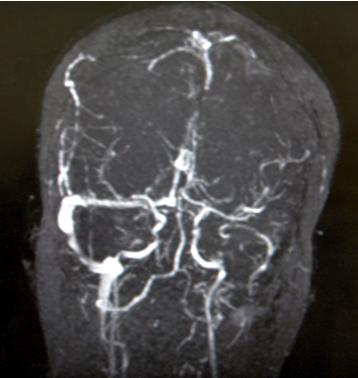
We studied 30 cases colligated in the department of neurology of the university hospital of Fez (Morocco). This study was conducted between January 2003 and October 2007 and lasted 58 months. All patients demonstrating clear radiological signs of CVT were included. The cerebral CT-scan was performed in 27 patients (90%). The period between onset and CT scan varied from one day to 45 days. 17 patients underwent the MRI examination (56%). Ninety percent of patients (90%) received anticoagulant therapy. The inclusion criteria were spontaneous hyperdensity or cord sign (CT scan before contrast injection); empty delta sign and empty lateral sinus sign (after contrast injection). Basing on MRI, criteria were hypersignal on T1 and T2 of sinuses (Fig. 3), abnormal defect or rupture of the sinus in MRV except two cases of deep cerebral venous thrombosis who presented indirect signs of thrombosis of deep veins. The MRI T1 and T2 weighted were done in axial, sagittal and coronal slices. Axial FLAIR and echoplanar susceptibility-weighted (T2*), and T1 with gadolinium injection were also achieved. Our patients have had the MRI and MRV between the fifth and thirtieth day of onset. The diagnosis of sinus thrombosis was based on hyperintense signal on T1 and isointense or hyperintense signal on T2, and by the absence of flow on MRV. The diagnosis using the CT scan was based on the presence of: empty delta sign or empty lateral sinus sign.
The CT scan was sufficient for establishing the diagnosis in 13 cases (43%). Consequently, the MRI examination was not performed for these patients. The MRI examination was performed directly and without earlier CT-scan in 3 patients (10%). Fourteen patients (47%) have benefited from both CT scan and MRI.
RESULTS
The mean age of our patients was 29 years old, ranging from 18 days to 65 years old. High predominance of female involvement was noticed with sex ratio of 2.3. The average period between the onset of symptoms and consultation was 18 days. The table 1 summarizes patients’ data.
Clinical presentation
The mode of onset of symptoms was subacute in 50% of cases, acute in 47% and progressive in one case (3%).
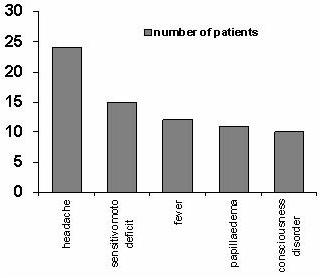
The clinical presentation was variable, but the most common symptoms were headaches in 24 cases (80%), motor and sensitive disability in 15 cases (50%), seizures in 10 cases (33%) including two cases of status epilepticus, consciousness disorder was noticed in 10 cases (33%) and fever (40%) (Fig. 1).
Biological and Radiological Examinations
The biological examination showed anemia in 13 cases (43%), hyperleucocytosis in 8 cases (27%), raised erythrocyte sedimentation rate in 11 cases (37%), thrombophilia was recorded in four patients including low S-protein in three cases and C-protein in one case.
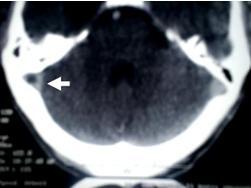
The CT-scan showed direct signs such as empty lateral sinus in 11 cases (37%) (Fig. 2), cord sign in six cases (20%), empty delta sign in seven cases (23%). The indirect signs were cortical hypodensity in 10 cases (33%), subcortical hypodensity in 12 cases (40%), parenchymal hematoma (1 case), enhancement of wall sinuses after contrast agent injection in 9 cases (30%), multiple and grouped hyperdensities in six cases (20%).
14 patients benefited from both CT scan and MRI examinations. The CT scan performed diagnosis in five cases (35%), confirmed by MRI associated with MRV. The CT scan was normal in three cases (21%). The MRI associated with MRV was more efficient in demonstrating the lesion compared to CT in 9 patients (65%) (Table 2).
The CT-scan and/or MRI including the MRV showed the CVT in the sagittal superior sinus (SSS) in 15 cases (50%), right lateral sinus (RLS) in 12 cases (40%), left lateral sinus (LLS) in 3 cases (10%), cavernous sinus (CS) involvement in 5 cases (16%), deep cerebral vein in two cases (7%), and cortical cerebral vein in one case. The diagnosis of cortical cerebral vein thrombosis was performed by a hyposignal on echo-planar susceptibility weighted (T2*) images in one case (Fig. 5).
The diagnosis of deep cerebral vein thrombosis was performed by indirect signs on MRI, and theses cases have shown normal deep venous system on MRV images.
Etiology
All patients underwent systematically an investigation of the thromboembolic antecedent, clinical examination, blood cells enumeration, prothrombin time (PT), activated partial thromboplastin time (APTT), erythrocyte sedimentation rate (ESR) and a thoracic x-ray.
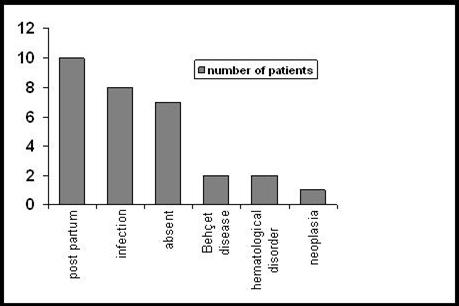
The post-partum was the most frequent cause of CVT in our series consisting of 10 cases (33%); infectious origin was seen in 8 cases (26%), four cases of otomastoiditis, three cases of severe staphylococcal of the face and these patient have had delayed treatment, one case of ethmoiditis, one case of miliary tuberculosis; Behcet disease in 2 cases (7%); pulmonary carcinoma in 1 case; essential thrombocytemia in 1 case and thrombophilia in one case (deficiency in protein C) (Fig. 4). Finally, the CVT was idiopathic in 7 cases (23%).
The Treatment
The treatment of intracranial hypertension was based on carbonic anhydrase inhibitor or mannitol (63%), and the lumbar puncture was performed in order to remove the cerebrospinal fluid (23%). Most of our patients (90%) received heparinotherapy (low-molecular-weight heparin 68% or standard heparin 32%) relieved by oral anticoagulant for 6 months. Four patients (10%) did not receive heparin, two have had a thrombosis of the cavernous sinus complicated by a carotid aneurysm; hence the anticoagulation was contraindicated. The third patient was the newborn of 18 days.
The antibiotherapy was administrated to patient with infectious origin (47%). The antiepileptics (27%) were prescribed to cases of seizures. We used steroids (prednisone 1mg/kg/day) in two cases of Behcet disease. Allopurinol (300mg/day) and hydroxycarbamid (1000mg/day) were used in cases of essential thrombocytemia. Two patients with severe disorder of consciousness were hospitalized at the intensive care department; one of them has died in this unit. The surgery was not the treatment of choice in any of the reported cases.
The Outcome
After treatment, a full recovery was noticed in 18 cases (60%). The squealaes were observed in 8 patients (27%), these consisted of blindness in one case associated to cavernous sinus thrombosis. Hemiparesis was noticed in 3 cases, tetraplegia associated to cognitive dysfunction was recorded one case of deep cerebral veins. The epilepsy was noticed in a case stabilized using carbamazepin; the ophtalmoplegia after a cavernous sinus thrombosis; pyramidal hypertonia at the newborn of 18 days. Three patients died (10%) including one post partum, one of cavernous sinus thrombosis and one idiopathic.
DISCUSSION
The cerebral venous thrombosis is a rare type of stroke that might occur at any age. The diagnosis of CVT requires a visualization of the thrombosis, which is commonly demonstrated by cerebral MRI and MRV. The CT-scan might be helpful but does not allow establishing the diagnosis.
The CVT affects about five people per million per year and represents 0.5 % of all strokes [6]. The CVT might occur in any stage of life including newborn and old people. Most authors are unanimous about the predominance of the CVT in young subjects, which was also revealed in our study. Similar agreement was found for the gender ratio [6]. It is not verified in our series because the sex ratio is 2,3. This feminine predominance is explained by the frequency of the CVT owing to post – partum cause in our study.
The clinical presentation is determined by the patient age, the delay between the onset and the hospitalization, the location of the thrombosis and the occurrence of cerebral parenchymal lesions.
The clinical presentation is dominated by headache which represents the main and first symptom in all studies. The CVT associating isolated headache symptom only is possible without associating the intracranial hypertension, subarachnoid haemorrhage, or meningitis [16]. Other symptoms are partial and generalized seizures, motor or sensitive deficits, altered consciousness, and papilloedema which might be associated to other symptoms [4]. Motor or sensitive deficit, altered consciousness and seizures are frequent in our study like Einhäupl study (1990); this was mostly related to delayed patients consultation. The 18 days newborn patient has shown generalized seizures and hyporeactivity as the main symptoms of the SSS thrombosis. The case n° 20 has shown isolated cortical cerebral vein thrombosis revealed by motor deficit without seizures association.
In SSS thrombosis, signs are dominated by the unilateral or bilateral motor deficit seizures and consciousness disorder. On the other hand, the isolated intracranial hypertension syndrome is not frequent in SSS thrombosis. However, the CVT of the LS is often revealed by an isolated intracranial hypertension syndrome. When the left LS is affected, aphasia may occur. One patient in our study presented with Wernicke aphasia and partial seizures.
The clinical manifestations of deep CVT are more severe. They often include coma and bilateral motor deficit. These manifestations have been noticed in case n° 18, while the case n° 29 presented only a unilateral motor deficit. Seizures are more frequent during the CVT comparing to the other types of stroke. Seizures occur mainly in cases of parenchymal lesions, SSS thrombosis and in patients having motor or sensitive deficit [27].
Most of the routine blood assessment does not have diagnostic value of the CVT. However, this will probably assist in establishing the etiological diagnosis. Several studies confirmed the elevation of the D-dimers during the CVT but their predictive negative value seems only interesting for patients having signs of encephalic reach. As a result, an absence of D-dimers elevation in case of isolated headache can not eliminate the CVT diagnosis [15].
In our study, the cerebrospinal fluid (CSF) mostly showed abnormal composition and elevation of the intracranial pressure. The CSF assessment revealed associated purulent meningitis in two patients, meningitis with an increased number of lymphocytes and red cells, an isolated elevation of red cells at two patients. However, we did not find any elevation of proteins in CSF. The opening pressure was elevated in all patients except the cases of cavernous sinus thrombosis. It varies between 19 and 48 cm H2O.
Detailed CT scan findings have been described in earlier literature [11-10]. The CT scan without and with of contrast agent injection remains the first exam done whenever a CVT is suspected [23, 28]. It provides the diagnosis proof and allows showing the direct signs of CVT. However, up to 20% CVT cases have shown a normal CT [7]. More frequently there are patients with isolated intracranial hypertension. Therefore, a CVT diagnosis should be systematically discarded before retaining an idiopathic intracranial hypertension diagnosis [25, 21]. However, the CT scan sensitivity was 30% in Ameri study [1]. The empty delta sign (the frequent direct sign) was found in six patients (23%) compared to 20% found in the literature [30]. The empty lateral sinus sign is the equivalent of the empty delta sign. This seemed to be underestimated in the literature [2], whereas it represents the first direct sign in our study and was found in 11 patients (37%). It is necessary to differentiate it from hypoplasic sinus mainly the left lateral sinus. A special attention must be given to the signs of the transverse sinus on the mastoid in images before contrast agent injection.
Indirect signs are more frequent and less specific compared to direct signs in the different studies. This was also confirmed in our study (85%). Most often, the CT-scan shows thrombosis consequences on the cerebral parenchyma under shape a hypodensity (oedema or venous infarction), or a hyperdensity bound to a haemorrhage going from some small patches to a real intraparenchymal haematoma. The infarct is frequently hemorrhagic (10 to 50% of cases in the literature) [13]. In our study, the CT scan was sufficient to diagnose 50% of cases at the admission.
Currently, the golden rule is to combine the MRI and the MRV for visualizing the thrombosed vessel. The indirect signs of the CVT shown in the MRI are not specific and are similar to those in the CT scan. The sensitivity of the MRI associating the MRV is 90% in Lafitte study [26]. The MRI and the MRV allowed the diagnosis in all cases of our series (56%) (Fig.7). The MRI alone is limited by flow artifacts that can lead to false positives and the absence of hyperintense signal on T1 and T2-weighted images at the onset of acute thrombosis [19]. During the first 3 to 5 days the thrombosed sinus is isointense on T1 and hypointense on T2. It is then too difficult to differentiate it from normal veins. All MRI examinations have been carried out after the 5th day of the onset. For all cases; (except those with deep veins thrombosis, cortical veins thrombosis and the cavernous sinus thrombosis); the thrombosed sinus was hyperintense on T1 and hyper or isointense on T2. MRV done alone cannot discriminate hypoplasia than lateral sinus thrombosis [3]. It is illustrated by one case (n° 5) that shows an amputation of the hypoplasic LLS confirmed by morphological T2 and T1 sequences. The cortical or deep vein thrombosis might be misdiagnosed even by MRI and MRV. This fact occurred in one case presented with a deep vein thrombosis (case N° 18).
The diagnosis of isolated cortical vein thrombosis could be difficult, requiring conventional angiography. In our series, conventional angiography investigation was not used. The Echo-planar susceptibility-weighted images (T2*) are particularly useful in isolated cortical venous thrombosis and during early stage of acute CVT when T1 and T2 lack sensitivity [24]. The diagnosis of cortical venous thrombosis was performed by echo-planar susceptibility-weighted images (T2*) at one patient (case n° 20) (fig. 5).
The thrombosis of the cavernous sinus was revealed in three cases by absence of heightening of one or the two cavernous sinuses in the coronal T1 images after Gadolinium injection. Two patients had cavernous sinus thrombosis associated with intracavernous carotid aneurysm.
The CVT is often multifactorial since several disorders might initiate or dispose patients. International studies of the Cerebral Vein and Dural Sinus Thrombosis (ISCVT) 44% of the patients had shown more than one origin and predisposing factor including the congenital and genetic thrombophilia was recorded in 22% patients [22]. In developed countries, non-infectious origins such as oral contraceptives, cancer, and thrombophilia are the most frequent with a prevalence of 80% [4, 5]. The etiologies in our study were similar to the developing countries findings [32, 17]. Infections and post-partum causes are the most frequent. Local infectious etiologies are observed in seven cases including four cases of otomastoiditis, three cases of severe staphylococcal of the face and one case of ethmoiditis. CVT in these cases may be explained by the consultation delay of our patients. The CVT represents 23.5% of the stroke during pregnancy and postpartum [9]. Several factors could be associated to the postpartum CVT; this included the caesarean, the arterial hypertension, and anemia. On the other hand, eclampsia is not a risk factor. Indeed no case of eclampsia has been registered in our study [20]. In one case, CVT occurred after epidural analgesia. Oral contraceptives represent 12% in Biousse and Bousser study. In our context, we are convinced that some cases are not diagnosed considering the increasing use of the oral contraceptives. Hemostasis investigation includes congenital or genetic thrombophilia (deficiencies in antithrombin III, protein C, and protein S and having the factor V Leiden or prothrombin gene mutations, and antiphospholipid antibodies). We have investigated the thrombophilia in four cases; and one case of deficiency in protein C, and two cases in protein S were revealed. The protein S deficiency was not confirmed by a second dosage. Congenital thrombophilia is certainly underestimated in our study. CVT due to Behcet disease is frequent in Mediterranean countries, but Behcet’s cases seem less frequent in our study compared with Daif study. The low frequency of Behçet disease might be explained by our limited cases. CVT was idiopathic in 20% in agreement with literature data [14].
Heparin (low-molecular-weight heparin or standard heparin) is the first-line treatment even in presence of hemorrhagic infarction [18, 29]. In our study, 90% of patients benefited from the anticoagulant treatment including those with hemorrhagic infarction. Systemic or local thrombolysis may be used in CVT when patients deteriorate despite adequate anticoagulation and other causes of deterioration have been ruled out, thrombolysis or thrombectomy may be considered in specialized centers [12, 31]. In patients with isolated intracranial hypertension, a lumbar puncture for removing the cerebrospinal fluid is required before starting heparin. If intracranial pressure is severely raised, the general recommendations should be followed, this starts with mannitol treatment to admission to an Intensive Care Unit with intracranial pressure monitoring or even decompressive hemicraniectomy when a risk of cerebral herniation exists. We used carbonic anhydrase inhibitor for intracranial hypertension or mannitol or even steroids although they are not recommended by most authors [8]. Antiepileptics and antibiotics are useful to treat seizures and infection. One patient underwent partial epilepsy stabilized under carbamazepin. The advisable anticoagulant treatment duration is six at 12 months. For our patients, the mean duration of anticoagulation was 6 months. ISCVT shows that death and severe sequelaes were observed in 15% of patients [22]. In our study, the result was similar to ISCVT (13% vs 15%).with two cases of severe sequelaes and two cases of death.
CONCLUSION
CVT is not uncommon in Morocco. Post-partum and infectious causes are more frequent in this study. Behcet’s disease etiology seems to be underestimated. The investigation of the haemostasis should be a routine after each cerebral venous thrombosis. The MRI and Venous MR angiography are the key diagnostic tools. The outcome is favorable using heparin treatment.
| Aknowledgments |
| To Mr El Hashimi M. and Dr. Boujraf S. for their cooperation in revising the English text. |
Table 1 -Patients data
| Patient Number |
Age, gender |
Clinical symptoms |
Causes and risk factors |
Topography |
Parenchyma involevment |
Outcome |
| 1 |
11, M |
ICH, P, IIIrd np, VIth np, exophtalmos, |
Severe staphylococcal of the face |
SC |
no |
normal |
| 2 |
27, F |
ICH, P, motor deficit, DC |
Post partum, otomastoiditis |
SSS
SLD |
yes |
Motor deficit |
| 3 |
60, M |
Seizures, motor deficit, DC, fever |
absent |
SLD |
yes |
normal |
| 4 |
24, F |
Ptosis, headache , IIIrd np, VIth np, exophtalmos, DC, fever |
Severe staphylococcal of the face |
SC |
no |
IIIrd np, VIth np |
| 5 |
17, F |
ICH, P, VIth np, exophtalmos, fever, |
Probable local infection |
SC |
no |
death |
| 6 |
27, F |
ICH, P, seizures, motor deficit, |
Post partum |
SSS |
yes |
seizures |
| 7 |
43, M |
Seizures, motor deficit, |
Absent |
SSS
SLG |
yes |
normal |
| 8 |
28, F |
ICH, seizures, motor deficit, DC |
Post partum |
SSS |
yes |
death |
| 9 |
21, F |
ICH, fever |
Post partum |
SSS |
No |
normal |
| 10 |
17, M |
ICH, P, |
Behçet disease |
SLD |
No |
normal |
| 11 |
18, F |
Headache, status epilepticus, motor deficit, DC, fever |
Post partum |
SSS
SLD |
Yes |
normal |
| 12 |
18, F |
ICH, P, fever |
Otomastoiditis |
SLG |
No |
normal |
| 13 |
46, M |
ICH, IIIrd np, VIth np |
Severe staphylococcal of the face |
SC |
No |
Blindness, IIIrd np, VIth np |
| 14 |
54, M |
ICH, P, motor deficit |
Pulmonary carcinoma with metastasis |
SLD |
yes |
death |
| 15 |
25, F |
ICH, P, status epilepticus, DC, fever |
Post partum |
SSS
SLD |
yes |
normal |
| 16 |
24, M |
Headache, fever, IIIrd np, VIth np exophtalmos |
Ethmoiditis |
SC |
no |
normal |
| 17 |
65, F |
DC |
Miliary tuberculosis |
SLD |
no |
normal |
| 18 |
25, F |
Status epilepticus, DC, fever |
absent |
Basilar veins, ICV |
yes |
Cognitive dysfunction, motor deficit |
| 19 |
13,M |
ICH, P |
otomastoiditis |
SLD |
No |
normal |
| 20 |
40, F |
Headache, motor deficit |
Post partum, epidural analgésia |
Cortical vein |
No |
normal |
| 21 |
7, F |
ICH, P, fever |
Absent |
SSS
SLD
SLG |
No |
normal |
| 22 |
55 |
ICH, motor deficit, DC |
Absent |
SLG |
Yes |
death |
| 23 |
18 months, F |
Status epileptcus, hyporeactivity |
Protein C deficiency |
SSS |
yes |
Pyramidal hypertonia |
| 24 |
40, F |
Headache, seizures, motor deficit |
Post partum |
SSS |
yes |
Motor deficit |
| 25 |
19, F |
Headache, DC |
Post partum, |
SLD |
No |
normal |
| 26 |
18, F |
ICH, P |
Essential thrombocytemia |
SSS |
No |
normal |
| 27 |
44,F |
ICH, motor deficit, fever |
absent |
SSS, RLS |
no |
normal |
| 28 |
24,F |
Headache, DC |
Post partum |
SSS, LLS |
yes |
normal |
| 29 |
28,M |
Motor deficit |
Behcet disease |
Basilar veins |
yes |
Motor deficit |
| 30 |
23,F |
ICH, seizures, DC, fever |
absent |
SSS |
yes |
normal |
IIIrd np, third nerve paralysis; DC, disorder of consciousness; ICH, intracranial hypertension; ICV, internal cerebral veins; P, papilledema SSS, superior sagittal sinus; LLS, left lateral sinus; RLS, right lateral sinus; CS, cavernous sinus; F: feminine; M: masculine.
Table 2 – The 14 patients with both CT scan, MRI and MRV
| Case |
CT scan |
MRI |
MRV |
Thrombosed sinus or vein |
| 1 |
Absence of bilateral CS enhancement, |
Absence of bilateral CS enhancement, aneurysm of left intracavernous carotid |
normal |
CS |
| 3 |
Cortical and subcortical hypodensity |
HS T1,T2 RLS; venous infarction |
Amputation RLS |
RLS |
| 5 |
normal |
Absence of bilateral CS enhancement, venous infarction. |
Amputation LLS (hypoplasia). |
CS |
| 6 |
Cortical and subcortical hypodensity, multiple grouped hyperdensities |
IsoT1, hypoT2 SSS; hemorrhagic infarction |
Amputation SSS |
SSS |
| 14 |
Empty lateral sinus sign, enhancement of sinus wall, cortical and subcortical hypodensity |
HS T1,T2 RLS ; multiple metastasis |
Amputation RLS |
RLS |
| 16 |
Absence of bilateral CS enhancement, convexity and enhancement of CS wall |
Absence of right CS enhancement; aneurysm of right intracavernous carotid |
Normal |
CS |
| 17 |
Cord sign, empty right lateral sinus sign. |
HS T1,T2 RLS; multiple tuberculoma. |
Amputation RLS. |
RLS |
| 18 |
bilateral venous infarction (Rosenthal vein and intern cerebral vein). |
Partiel obstruction of LLS (T1 Gadolinium), bilateral venous infarction (Rosenthal vein and intern cerebral vein). |
Normal |
Rosenthal vein and intern cerebral vein |
| 20 |
normal |
HS FLAIR, hyposignal T2* of a cortical vein . |
normal |
Cortical vein |
| 21 |
Empty delta sign, empty lateral sinus sign (right and left) |
HS T1,T2 RLS, LLS, SSS |
Amputation SSS, RLS, LLS |
SSS, RLS, LLS |
| 24 |
Hematoma |
Hematoma |
Defects SSS |
SSS |
| 25 |
Empty right lateral sinus sign |
HS T1, T2 RLS |
normal |
SSS |
| 26 |
normal |
HS T1, isosignal T2 SSS |
|
|
| 28 |
Cortical and subcortical hypodensity, multiple grouped hyperdensities |
hemorrhagic infarction |
Defects SSS, LLS |
SSS, LLS |
HS, hypersignal intensity; SSS, superior sagittal sinus; LLS, left lateral sinus; RLS, right lateral sinus; CS, cavernous sinus
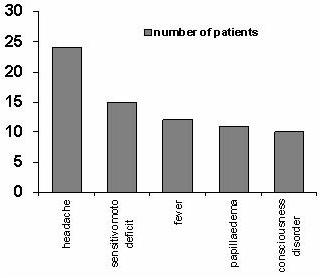
Figure 1
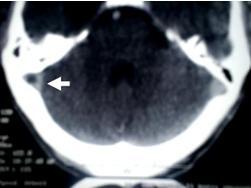
Figure 2 (case N° 14)
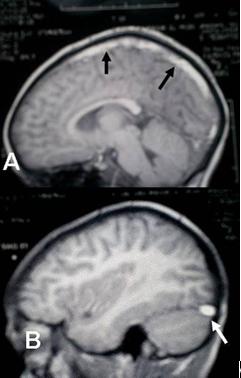
Figure 3 (case N° 21)
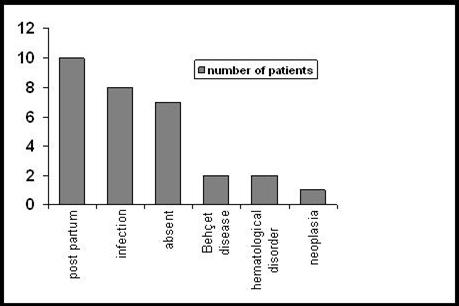
Figure 4
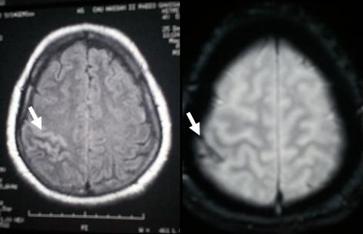
Figure 5 (case N° 20)
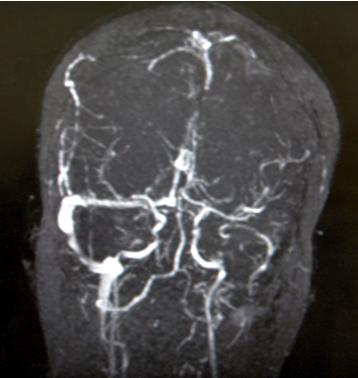
Figure 6
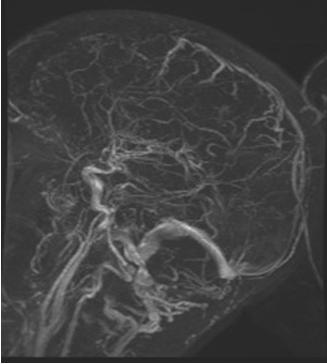
Figure 7