CLINICAL STUDIES / ETUDES CLINIQUES
EFFECTIVENESS OF SUMATRIPTAN FOR ACUTE TREATMENT OF MIGRAINE HEADACHE IN AN AFRICAN POPULATION
- College of Medicine, University of Ibadan, Nigeria
- University of Maiduguri Teaching Hospital, Maiduguri, Nigeria
- University of Nigeria Teaching Hospital, Enugu
- GlaxoWellcome Nigeria Limited, 41, Creek Road P.M.B. 1401, Apapa, Lagos
ABSTRACT
Background
The triptans are currently the drugs of choice for acute treatment of migraine. Although there are several newer triptans, sumatriptan that was first introduced into clinical practice is still preferred to newer triptans by subjects in several clinical trials.
Objective
This study was conducted to determine the effectiveness of sumatriptan in an African population where triptans have not been introduced.
Methods
Subjects were recruited consecutively in three large teaching hospitals that are located in ethno-geographically different regions in Nigeria. Migraine headaches, which were classified using the criteria of the International Headache Society, were rated on visual analogue scale, while associated symptoms of migraine were rated on ordinal scale. Ratings of headaches and of associated symptoms before and four hours after 50 mg sumatriptan dose were compared using non-parametric tests.
Results
42 subjects, 11 males and 31 females, completed the study. 11 (26 %) subjects had migraine with aura, while 31 (74 %) subjects had migraine without aura. Before treatment headache was rated 0 -3 by no subject, 4 – 7 by 20 subjects, and 8 -10 by 22 subjects, but after treatment headache was rated 0 – 3 by 30 subjects, 4 – 7 by 7 subjects, and 8 – 10 by 5 subjects (P < 0.0001). Before treatment, 15 (36 %) subjects had nausea or vomiting, 23 (55 %) subjects had photophobia or phonophobia, and 36 (86 %) subjects had severe impairment of activity. Photophobia and phonophobia were reduced significantly (P < 0.0001), impairment of activity was reduced significantly (P = 0.02), but the proportion of subjects with nausea and vomiting did not change significantly (P > 0.05). Severity of headache, presence of associated symptoms, and impairment of activity were not associated with relief
of headache.
Conclusion
Sumatriptan is effective to relieve the headache and the associated symptoms of migraine, and to induce early return to activity in this study population. Sumatriptan was well tolerated without serious clinical adverse effects.
Keywords: Africa, Headache, Migraine, Sumatriptan
RESUME
Introduction
Les triptans représentent actuellement le traitement de choix des migraines. Bien qu’il y ait plusieurs types de triptans, le sumatriptan qui fut le premier a être introduit sur lemarché, a la faveur des prescripteurs.
Objectif
L’objetif du travail présenté est d’étudier l’effet du sumatriptan sur une population africaine.
Methodes
Les sujets ont été recrutés consécutivement dans 3 hôpitaux universitaires situés dans différents zones géographiques du Nigéria. La classification répondait aux critères de l’ International Headache Society . L’évaluation des migraines a été réalisée avant puis 4 heures après la prise de 50 mg de sumatriptan.
Résultats
42 sujets, 11 de sexe masculin et 31 de sexe féminin composaient le groupe d’étude. 11 (26%) présentaient une migraine avec aura, tandis que 31 (74%) signalaient une absence d’aura.Avant le traitement les migraines se répartissaient selon les scores suivants : 0 – 3, 4-7 20 patients ; 8 – 10, 22 patients. Après traitement, l’évaluation était la suivante : 0 – 3, 30 patients ; 4 – 7, 7 patients ; 8 – 10, 5 patients ( P < 0.0001). Avant le traitement, 15 (36%) patients présentaient des nausées et des vomissements, 23 (55%) se plaignaient de photophobie et de phonophobie, et 36% (86%) subissaient un gêne fonctionnelle importante. Les photophobies et phonophobie étaient réduites significativement ( P = 0.02), mais la proportion de sujets souffrant de nausées et vomissements était inchangée (P > 0.05). La sévérité des crises, la présence de signes associées, et la perturbation des activités sociales n’étaient pas correlées au soulagement des douleurs.
Conclusion
Le sumatriptan a un effet bénéfique sur les crises migraineuses et les signes associés et autorise un retour rapide aux activités sociales dans la population africaine étudiée. Le sumatriptan est bien toléré sans effet secondaire significatif.
Mots clés : Afrique, Céphalées, Migraine
INTRODUCTION
The triptans, which were introduced for acute treatment of migraine headaches about a decade ago are currently the preferred drugs for acute treatment of migraine [33]. They have been shown to relieve migraine headache fast, consistently, and with good tolerability [10]. The triptans, which are analogues of serotonin, have high affinity for 5HT1B/1D receptors, which are presynaptic, and for 5HT/1F receptors, which are postsynaptic [15, 41].
Although both neural and vascular hypotheses have been proposed to explain the pathogenesis of migraine [1], current opinion favours neural mechanisms [14, 29, 31], which involves activation of the trigeminovascular system [27]. The triptans have been shown to inhibit release of vasoactive peptides through agonist action at 5HT1B receptors [17, 43] that are located on the peripheral terminals of the trigeminal nerve. They have also been shown to inhibit transmission of impulses at the nucleus caudalis of the trigeminal nerve [9, 17] through agonist action at postsynaptic 5HT1F receptors [15, 17]. Furthermore a study, which showed that sumatriptan scavenges free radicals in vitro [18], suggests that the triptans may act through non-neural mechanisms.
Several studies have shown that patients with migraine prefer drugs that not only relieve headache rapidly [37], but also relieve associated symptoms rapidly [24]. The triptans have been shown to meet several of patients’ requirements for rapid relieve of their migraine [9]. Several triptans, many of which have comparable efficacy, have been approved for clinical use in several countries, and have been shown to be safe [28, 42]. Sumatriptan, the first triptan introduced into clinical use, is still the most widely prescribed triptan [9]. Sumatriptan has been shown to be superior to placebo [36], analgesics [7, 35], and ergot drugs for the relief of the headache [3, 8]and of the associated symptoms [24] of migraine.
Although sumatriptan has been shown to relieve migraine headache effectively in several clinical trials, response of patients has not been uniform [45]. In African populations where very few clinical trials of the triptans have been carried out [21], there is the need for more information about the response of patients with migraine to the triptans. This study was conducted to determine the effectiveness of sumatriptan for the acute treatment of migraine headache in an African population.
PATIENTS AND METHODS
Study sites
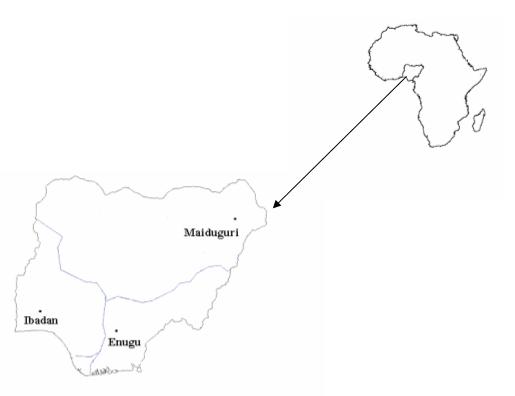
This study was conducted in three large teaching hospitals in Nigeria, which are located in three major towns, Ibadan, Enugu, and Maiduguri (Figure 1). The catchment of each teaching hospital is within distinct large ethnic groups in Nigeria. Subjects were recruited consecutively over a period of one year from patients attending the neurology outpatient clinics of the teaching hospitals after informed consent. Migraine headaches were classified by neurologists in each study site using the criteria of the International Headache Society [16].
Inclusion and exclusion criteria
Inclusion criteria were; subjects aged 18-65 years, duration of migraine attacks of at least one year, frequency of attacks of one to six per month, ability of subjects to distinguish migraine headache from other types of headaches, and ability of subjects to provide written informed consent to participate in the study. Exclusion criteria were; pregnancy or risk of pregnancy, breast-feeding, oral contraceptives, history suggestive of ischaemic heart disease or abnormal electrocardiogram (ECG) suggesting myocardial ischemia, severe hypertension with grade 3 or 4 hypertensive retinopathy changes or diastolic blood pressure greater than 95 mmHg, impaired hepatic or renal function, epilepsy, alcohol abuse with an average alcohol intake above 135grams/week, history of basilar migraine, ophthalmoplegic migraine, and cluster headache.
Detailed medical history was obtained from all subjects, and complete physical examination was done during the recruitment visit. 12 lead ECG, blood chemistry, full blood count, urinalysis and blood sugars were requested for all subjects. Subjects who fulfilled the inclusion criteria were recruited into the study.
Ratings of headache and associated symptoms
Subjects were taught to record the severity of headache on a visual analogue scale, which had a rating of 0 for no headache and a rating of 10 for the most severe headache. Ratings of 0 – 3 represented no to mild headache, 4 – 7 represented moderate headache, while 8 – 10 represented severe headache. Subjects were told to record the severity of headache immediately preceding the dose of sumatriptan, and to record the presence of associated symptoms like nausea, vomiting, photophobia, phonophobia, and of impairment of activity. Impairment of activity was rated as none, slight, severe, or required bed rest.
A drug bottle containing two 50 mg tablets of sumatriptan , a diary card with a 10-point visual analogue scale, and a card to report adverse effects were given to each subject at each visit. Subjects were instructed to take 50 mg sumatriptan orally when migraine headache is established.
Severity of headache, presence of associated symptoms, and impairment of activity were reassessed four hours after 50 mg dose of sumatriptan. Subjects who did not obtain relief of headache within 4 hours were allowed to take their usual migraine medications. Subjects were permitted to take a second dose of 50 mg sumatriptan if migraine headache recurred within 24 hours after initial headache had subsided. Subjects were not allowed to take any of their usual migraine drugs, analgesics, or antiemetics with sumatriptan. All adverse effects were recorded on a separate card. Subjects were instructed to report to the neurology outpatient clinic within 48 hours of each migraine attack treated. The protocol for this study was developed by GlaxoWellcome.
The local ethical committees of the respective teaching hospitals approved the study. The study was performed in accordance with the Declaration of Helsinki, as revised by the World Medical Assembly, Venice, 1983 or Hong Kong 1989. GlaxoWellcome Nigeria monitored the study in accordance with corporate Standard Operating Procedure, which complied with the principles of Good Clinical Practice.
Statistics
Changes in the ratings of headache before and after the dose of sumatriptan were compared using the sign test, while changes in the proportion of subjects with photophobia and phonophobia, nausea and vomiting, and impairment of activity were compared using chi square test. The relationship of relief of headache, as outcome variable, with severity of headache before treatment, age less than or above 40 years, gender, presence of nausea and vomiting, and presence of photophobia and phonophobia, as predictor variables, was tested using conditional logistic regression. Relief of headache was defined as headache rating of 0-3 after the dose of sumatriptan. Statistics were done using the SPSS statistical package version 10 (SPSS Inc., Chicago, IL, USA).
RESULTS
55 subjects, 20 in Ibadan, 16 in Enugu, and 19 in Maiduguri, were recruited into the study, but 13 subjects defaulted, five from Ibadan, two from Enugu and six from Maiduguri. Default was due largely to irregularity of hospital services, which occurred during the study. The characteristics of the subjects are presented in Table 1. The characteristics of the subjects who defaulted were not different from the subjects who completed the study. The mean age of 42 subjects, 11 males and 31 females who completed the study, was 34 years (SD 8, median 35, range 18 – 48). 31 subjects had migraine without aura, while 11 subjects had migraine with aura. The mean duration of migraine was 9 years (SD 7, median 7, range 1-34), while the mean frequency of migraine attacks per month was 3 (SD 0.5, median 3, range 3-4). Subjects in the three study centres were comparable with respect to age, duration of migraine, and frequency of attacks of migraine headache per month (Table 1).
Ratings of migraine headache and of associated symptoms are shown in Table 2. Before the 50 mg dose of sumatriptan no subject rated headache 0 – 3, but four hours after the dose of sumatriptan 30 (71 %) subjects rated headache 0 – 3 (P < 0.0001). Headache was rated as severe by 22 (52 %) subjects before 50mg dose of sumatriptan, but by 5 (12 %) subjects four hours after the dose of sumatriptan. Before the dose of sumatriptan 15 (36 %) subjects had nausea or vomiting compared with 7 (17 %) subjects after the dose of sumatriptan (P = 0.09). Photophobia and phonophobia were present in 23 (55 %) subjects before the dose of sumatriptan, but in 4 (10 %) subjects after the dose of sumatriptan (P < 0.0001). Severe impairment of activity or bed rest that were present in 36 (86 %) subjects before the dose of sumatriptan, were present in 5 (12 %) subjects after the dose of sumatriptan (P = 0.02). Relief of headache was described as meaningful by 30 (71%) subjects. 3 (7 %) subjects had recurrence of headache that required the use of rescue dose of 50 mg sumatriptan within 24 hours of initial relief of headache.
Relief of headache was not associated with type of migraine (p > 0.05), severity of headache before treatment (p > 0.05), presence of nausea or vomiting (p > 0.05), presence of photophobia or phonophobia (p > 0.05), and impairment of activity (p > 0.05), but was associated with age (p = 0.01). Subjects less than 40 years of age were more likely to obtain relief of headache than subjects older than 40 years. None of the subjects reported any significant adverse effects, and none withdrew from the study because of adverse effects.
DISCUSSION
This study shows that sumatriptan is effective to relieve the headache of migraine. The proportion of subjects that had migraine headache relieved completely or reduced to mild levels, in this study, is comparable to the findings of clinical trials in populations outside of Africa [37]. Recurrence of headache after initial relief is one of the reasons for dissatisfaction with the triptans [13]. Following initial relief of headache after 50 mg sumatriptan dose, recurrence of migraine headache has been shown to range from 27 % to 41 % [12]. The finding of this study, which shows that 7 % of subjects took rescue medication after initial relief of headache, indicates that the effects of sumatriptan is lasting. Effectiveness of sumatriptan in this study is also shown by the high proportion of subjects who described relief of headache as meaningful.
Sumatriptan is effective irrespective of the severity of the headache in this study. Furthermore the type of migraine, with or without aura, is not associated with relief of headache. Sumatriptan has been shown to be effective for both migraine with and without aura [10]. The effectiveness of sumatriptan is also not associated with the presence of photophobia or phonophobia in this study. Although relief of migraine headache was shown to be correlated with relief of nausea and vomiting in one study [22], nausea and vomiting are often not relieved in a large proportion of patients treated with the triptans [26]. In this study the presence of nausea and vomiting was not associated with relief of headache. Relief of headache was also not associated with impairment of activity. However, subjects younger than 40 years of age were more likely to obtain relief of headache than subjects older than 40 years of age in this study.
Since migraine is more than just the headache [37], relief of associated symptoms is an important component of acute management of migraine. Photophobia and phonophobia has been reported by about 93 % of subjects with migraine in some studies [37]. In this study sumatriptan was effective to relieve photophobia and phonophobia, which were present in 55% of subjects. Nausea and vomiting has been reported in about 76 % of subjects with migraine [37]. Although sumatriptan has been shown to be better than placebo to relieve nausea and vomiting, most subjects in this study did not obtain relief of nausea and vomiting. Impairment of activity has been reported in up to 83 % of subjects with migraine [5]. Early return to activity is one of the preferences of migraine subjects for an effective drug [37]. In this study sumatriptan was effective to induce early return to activity, which was impaired in 86 % of subjects.
Extensive post-marketing studies have shown that 50 mg sumatriptan given orally is well tolerated without serious clinical adverse effects [11, 19, 28].Common adverse effects of sumatriptan include paresthesia, chest pressure, and chest pain [43]. Comparatively less CNS adverse effects have been associated with sumatriptan, probably because it is the least lipophilic of all the triptans [38] and may not penetrate the blood brain barrier as the newer triptans [20]. In this study no subject complained of any of the adverse effects that have been associated with sumatriptan.
Several triptans [30, 39, 44] have been compared with respect to effectiveness, tolerability, and cost, but there is no consensus that there are differences in the effectiveness and tolerability between the triptans [9, 40]. Although difference in the pharmacological profile of the triptans are known[10, 32], no clearly defined rationale has been established for choosing specific triptans [4, 45]. A study, which compared 53 clinical trials of triptans, concluded that finding the best triptan will involve trial and error because individual patient responses cannot be predicted [9]. Some studies, however, suggest that patients prefer specific triptans [2, 25, 30].
In conclusion this study shows that sumatriptan is effective to achieve lasting relief of the headache and most of the associated symptoms of migraine. Since economic consideration is an important component of the management of migraine [6, 34] in addition to rapid onset of complete relief of headache [23, 34], sumatriptan would be the appropriate triptan for this study population.
Funding
This study was funded by GlaxoWellcome, Nigeria.
| COMMENTS |
The authors discuss the problem of migraine in an African setting. They then undertake a trial of triptan to assess the response to treatment. They comment that this is a first study of a triptan in an African population. The study is well designed and appropriate checks and balances have been put into place. The article is well written and based on a solid and interesting discussion. However, there are some mistakes from a methodological point of view. It is not a randomised, but the observation of some patients before and after a treatment with sumatriptan.
The statement that sumatriptan remains the drug of choice should be considered with care as current studies suggest that eletriptan 40mg and rizatriptan 10mg have the best efficacy and tolerability.
The Editorial Board |
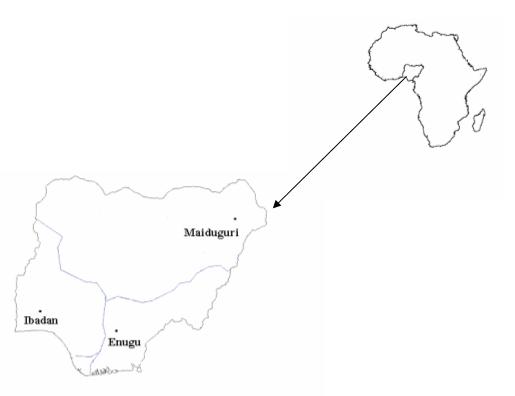
Figure 1: Map of Nigeria showing the study communities.
Table 1: Characteristics of subjects at baseline
| |
|
|
Study location |
|
| Characteristics of subjects |
|
Ibadan |
Enugu |
Maiduguri |
| Number of subjects |
|
|
|
| |
Male |
5 |
5 |
1 |
| |
Female |
10 |
9 |
12 |
| Mean age years (SD) |
|
34 (9) |
36 (7) |
30 (6) |
| Migraine type |
|
|
|
| |
With aura |
5 |
0 |
6 |
| |
Without aura |
10 |
14 |
7 |
| Mean duration of migraine in years (SD) |
|
6 (6) |
11 (9) |
10 (6) |
| Mean frequency of attacks per month (SD) |
|
4 (0.5) |
3 (0.4) |
3 (0.4) |
Table 2: Ratings of headache and associated symptoms before and four hours after 50 mg sumatriptan dose
| |
|
Before sumatriptan |
|
After sumatriptan |
| Symptoms |
|
n |
(%) |
n |
(%) |
| Headache |
|
|
|
|
|
| |
8-10 |
22 |
(52) |
5 |
(12) |
| |
4-7 |
20 |
(48) |
7 |
(17) |
| |
0-3 |
0 |
(0) |
30 |
(71) |
| Nausea or vomiting |
|
|
|
|
|
| |
Present |
15 |
(36) |
7 |
(17) |
| |
Absent |
27 |
(64) |
35 |
(83) |
| Light or sound sensitivity |
|
|
|
|
|
|
| |
Present |
23 |
(55) |
4 |
(10) |
| |
Absent |
19 |
(45) |
38 |
(90) |
| Impairment of activities |
|
|
|
|
|
|
| |
Bed rest |
21 |
(50) |
4 |
(10) |
| |
Severe |
15 |
(36) |
1 |
(2) |
| |
Slight |
6 |
(14) |
21 |
(50) |
| |
Absent |
0 |
(0) |
16 |
(38) |
REFERENCES
- ADAMS R, VICTOR M, ROPPER AH. Principles of Neurology. McGraw Hill, New York 1997; 185 – 187.
- ADELMAN J, LIPTON R, FERRARI M, DIENER H, MCCARROLL K, VANDORMAEL K, LINES C. Comparison of rizatriptan and other triptans on stringent measures of efficacy. Neurology 2001; 57: 1377-1383.
- BIGAL M, TEPPER S: Ergotamine and dihydroergotamine: a review. Curr Pain Headache Rep 2003; 7: 55 – 62 .
- CADY R, DODICK D. Diagnosis and treatment of migraine. Mayo Clin Proc 2002; 77: 255-261.
- CARO G, CARO J, BRIEN J, ANTON S, JACKSON J. Migraine therapy:development and testing of a patient preference questionnaire. Headache 1998; 38: 602-607.
- CARO J, GETSIOS D. Pharmacoeconomic evidence and considerations for triptan treatment of migraine. Expert Opin Pharmacother 2002; 3: 237 – 248.
- CHALAL R, KWONG W, PUTNAM G, THOMPSON D, O’QUINN S, WEBSTER C, METZ A. Patient satisfaction with imitrex tablets 50 mg compared with their usual non-triptan prescription or over-the-counter migraine therapy. Cephalagia 2001; 21: 411.
- Dahlof C. Clinical efficacy and tolerability of sumatriptan tablet and suppository in the acute treatment of migraine:a review of data from clinical trials. Cephalagia 2001; 21(Suppl 1): 9-12.
- FERRARI M, ROON K, LIPTON R, GOADSBY P. Oral triptans (serotonin 5-HT1B/ID agonists) in acute migraine treatment: a meta-analysis of 53 trials. Lancet 2001; 358: 1668-1675.
- FREITAG F. Acute treatment of migraine and the role of triptans. Curr Neurol Neurosci Rep 2001; 1: 125-132.
- GALLAGHER R, CUTRER F. Migraine: diagnosis, management, and new treatment options. Am J Manag Care 2002; 8(Suppl 3): S58-73.
- GERAUD G. Migraine headache recurrence:relationship to clinical, pharmacological and pharmacokinetic properties of triptans. Cephalagia 2001; 21: 406.
- GERAUD G, KEYWOOOD C, SENARD J. Migraine Headache Recurrence: Relationship to Clinical, Pharmacological, and Pharmacokinetic Properties of Triptans. Headache 2003 43: 367 – 388.
- GOADSBY P, LIPTON R, FERRARI M. Migraine- current understanding and treatment. N Engl J Med 2002; 346: 257 – 270.
- GOLDSTEIN D, ROON K, OFFEN W, RAMADAN N, PHEBUS L, JOHNSON K, SCHAUS J, FERRARI M. Selective serotonin 1F (5-HT1F) receptor agonist LY334370 for acute migraine: a randomised controlled trial. Lancet 2001; 358: 1230-1234.
- HEADACHE. Classification and diagnostic criteria for headache disorders, cranial neuralgia, and facial pain. Cephalagia 1988; 8: 1-96.
- HUMPHREY P. How it started. Cephalagia 2001; 21(Suppl 1): 2-5 (2001).
- IKEDA Y, JIMBO H, SHIMAZU M, SATOH K. Sumatriptan Scavenges Superoxide, Hydroxy, and Nitric Oxide Radicals: In Vitro Electron Spin resonance Study. Headache 2002; 42: 888 – 892.
- JAMIESON D. The safety of triptans in the treatment of patients with migraine. Am J Med 2002; 112: 135-140 (2002).
- JOHNSON D, ROLLEMA H, SCHMIDT A, MCHARG A. Serotonergic effects and extracellular brain levels of eletriptan, zolmitriptan and sumatriptan in rat brain. Eur J Pharmacol 2001; 425: 203 – 210.
- KWASA T, JOWI J, AMAYO E. Efficacy and tolerability of oral sumatriptan in the treatment of acute migraine. East Afr Med J 1995; 72: 479-482.
- LIPTON R, GOADSBY P, MCCARROLL K, ALLEN C, LINES C. Are migraine patients who are pain free at 2 h after treatment also more likely to be free of nausea. Cephalagia 2001; 21: 422.
- LIPTON R, HAMELSKY S, DAYNO J. What do patients with migraine want from acute migraine treatment? Headache 2002; 42(Suppl 1): 3-9.
- MARCUS D. Establishing a standard of speed for assessing the efficacy of the serotonin1B/1D agonists (Triptans). Arch Neurol 2001; 58: 1056-1058.
- MATHEW N. Comparison of therapeutic gains over sumatriptan for eletriptan, naratriptan, rizatriptan, and zolmitriptan:a review of six clinical studies. Cephalagia 2001; 21: 407.
- MATHEW N, SCHOENEN J, WINNER P, MUIRHEAD N, SIKES C. Comparative Efficacy of Eletriptan 40 mg Versus Sumatriptan 100 mg. Headache 2003; 43: 214 – 222.
- MAY A, GOADSBY P. The trigeminovascular system in humans: pathophysiologic implications for primary headache syndromes of the neural influences on the cerebral circulation. J Cereb Blood Flow Metab 1999; 19: 115 – 127.
- NAPPI G, SANDRINI G, SANCES G. Tolerability of the triptans: clinical implications. Drug Saf 2003; 26: 93 – 107.
- PARSONS A, STRIJBOS P. The neural versus vascular hypothesis of migraine and cortical spreading depression. current Opinion in Pharmacology 2003; 3: 73 – 77.
- PASCUAL J, MUNOZ R, LEIRA R. An open preference study with sumatriptan 50 mg and zolmitriptan 2.5 mg in 100 migraine patients. Cephalagia 2001; 21: 680-684.
- PETROBON D, STRIESSNIG J. Neurobiology of migraine. Nature Reviews Neurosciences 2003; 4: 386 – 398.
- RAPOPORT A, TEPPER S. Triptans are all different. Arch Neurol 2001; 58: 1479 – 1480.
- RAPOPORT A, TEPPER S, BIGAL M, SHEFTELL F. The triptans formulations: how to match patients and products. CNS Drugs 2003; 17: 431 -437.
- REEDER C, STEADMAN S, GOLDFARB S. Economic comparison of oral triptans for management of acute migraine:implications for managed care. Am J Manag Care 2002; 8(Suppl 3): S80-84.
- ROBBINS L. Triptans vs analgesics:patients preference. Cephalagia 2001; 21: 406.
- ROON K, LIPTON R, GOADSBY P, FERRARI M. Placebo in triptan trials:efficacy, tolerability and consistency. Cephalagia 2001; 21: 405.
- RYAN R. Patient treatment preferences and the 5-HT1B/1D agonists. Arch Intern Med 2001; 161: 2545-2553.
- SALONEN R. The Sumatriptan difference. Cephalagia 2001; 21: 18-20.
- SANDRINI G, FARKKILA M, BURGESS G, FORSTER E, HAUGHIE S. Eletriptan vs sumatriptan: a double-blind, placebo-controlled, multiple migraine attack study. Neurology 2002; 59: 1210-7.
- SAPER J. What matters is not the differences between the triptans, but the differences between patients. Arch Neurol 2001; 58: 1481-1482.
- SHEFTELL F, RYAN R, PITMAN V. Efficacy, Safety, and Tolerability of Oral Eletriptan for Treatment of Acute Migraine: A Multicenter, Double-Blind, Placebo-Controlled Study Conducted in the United States. Headache 2003; 43: 202-213.
- TEPPER S. Safety and rational use of the triptans. Med Clin North Am 2001; 85: 959-970.
- van den BROEK R, P BHALLA P, MAASSENVanDENBRINK A, de VRIES R, SHARMA H, SAXENA P. Characterisation of sumatriptan-induced contractions in human isolated blood vessels using selective 5-HTIB and 5-HT1D receptor antagonists and in situ hybridisation. Cephalagia 2002; 22: 83-93.
- WELCH K. Sumatriptan and naratriptan tolerability and safety: and update of post-marketing experience. Cephalagia 2001; 21(Suppl 1): 25-28.
- WHITAKER J. Triptans for Migraine Headache: Therapeutic progress meets a heterogenous patient response. Arch Neurol 2001; 58: 1482-1483.