
|
|
|
ORIGINAL PAPERS / ARTICLES ORIGINAUX
ETIOLOGICAL AND PROGNOSTIC FACTORS FOR STROKE IN YOUNG PEOPLE IN BRAZZAVILLE AND POINTE-NOIRE
FACTEURS ÉTIOLOGIQUES ET PRONOSTIQUES DES AVC DU SUJET JEUNE À BRAZZAVILLE ET POINTE-NOIRE
E-Mail Contact - PRINCE ELIOT GALIENI SOUNGA BANDZOUZI :
eliotprince2002@yahoo.fr
ABSTRACT Introduction. Strokes are a public health problem worldwide, increasingly affecting young people, especially in Sub-Saharan Africa. In Congo, strokes in young people between Brazzaville and Pointe-Noire are limited by the lack of recent data. Objective. To determine the etiological and prognostic factors of young people who suffered strokes in Brazzaville and Pointe-Noire. Methodology. This is a multicenter cross-sectional analytical study conducted in Brazzaville and Pointe-Noire over a period of 8 months. Patients aged 18 to 55 years old, hospitalized for a first stroke confirmed by brain imaging, were included. The study variables were: sociodemographic, clinical, paraclinical and stroke progression. Statistical analyses were performed using SPSS 21 software. Results. The hospital frequency was 49.8% in Pointe-Noire and 34.8% in Brazzaville. Hemorrhagic stroke was the most frequent (60.3%). The mean age of patients was 46.8 ± 6.9 years with a male predominance (53%). The main risk factors in Brazzaville and Pointe-Noire were: high blood pressure 72.9% and 62.6%, alcohol 25.7% and 49.6%; Human Immunodeficiency Virus infection 5% and 13.7%. Embolic heart disease (20.3%) was the most frequent cause of ischemic stroke and for Hemorrhagic strokes high blood pressure was found in 70% in both cities. The mortality rate was 24.5%, including 52.6% in Brazzaville and 47.4% in Pointe-Noire. Conclusion. Conclusion. Stroke in young people is increasing sharply in Congo with high mortality. This is an alarm bell that requires increased awareness of vascular risk factors in the general population. Keywords: Stroke, young people, aetiology, mortality, Congo.
RESUME Introduction. Les AVC constituent un problème de santé publique dans le monde, touchant de plus en plus les sujets jeunes surtout en Afrique Subsaharienne. Au Congo, les AVC chez les sujets jeunes entre Brazzaville et Pointe-Noire, sont limitées par le manque de données récentes. Objectif. Déterminer les facteurs étiologiques, pronostiques des sujets jeunes victimes d’AVC à Brazzaville et Pointe-Noire. Méthodes. Il s’agit d’une étude analytique transversale multicentrique menée à Brazzaville et Pointe-Noire sur une durée de 8 mois. Ont été inclus, les patients âgés de 18 à 55 ans, hospitalisés pour un premier AVC confirmé par une imagerie cérébrale. Les variables d’étude étaient : sociodémographiques, cliniques, paracliniques et évolutives des AVC. Les analyses statistiques ont été réalisées à partir du logiciel SPSS 21. Résultats. La fréquence hospitalière était 49,8% à Pointe-Noire et 34,8% à Brazzaville. L’AVC hémorragique était la plus fréquente (60,3%). L’âge moyen des patients était de 46,8 ± 6,9 ans avec une prédominance masculine (53%). Les principaux facteurs de risques à Brazzaville et Pointe-Noire étaient : l’hypertension artérielle 72,9% et 62,6%, l’alcool 25,7% et 49,6% ; l’infection au Virus de l’Immunodéficience Humaine 5% et 13,7%. Les cardiopathies emboligènes (20,3%) étaient la cause la plus fréquente des AVC ischémiques et pour les AVC hémorragiques l’hypertension artérielle était retrouvée dans 70% dans les deux villes. Le taux de mortalité était 24,5% dont 52,6% à Brazzaville et 47,4% à Pointe-Noire. Conclusion. Les accidents vasculaires cérébraux chez le sujet jeune sont en forte augmentation au Congo, avec une fréquence plus importante à Pointe-Noire. Il s’agit d’une sonnette d’alarme qui nécessite le renforcement de la sensibilisation des facteurs de risque vasculaire en population générale. Mots clés : AVC, sujet jeune, étiologie, mortalité, Congo. INTRODUCTION Stroke remains a significant public health concern, with a high mortality rate that is a worldwide issue. Historically, stroke has been predominantly observed in the elderly population in Western countries; however, in sub-Saharan Africa, there has been a notable shift in the epidemiological profile, with an increasing prevalence observed among the young population (24, 5, 19, 29). The occurrence of stroke in young people is significantly influenced by cardiovascular risk factors, including arterial hypertension, excessive alcohol consumption, a sedentary lifestyle, and smoking (6, 9, 4). In Congo, stroke represents the primary cause of hospitalisation and mortality in neurology departments, with a hospital frequency of 32.8% in young people and a mortality rate of 29.1% (23, 30). The paucity of recent data on stroke in young people between Brazzaville and Pointe-Noire limits the scope of this study. The extant literature on this subject primarily focuses on adult populations, with no distinction being made for young subjects. While these studies have yielded data on the risk factors and clinical manifestations of stroke in these cities, they do not permit direct comparison in young adults. The aim of this study is to determine the aetiological and prognostic factors for young stroke victims in Brazzaville and Pointe-Noire. METHODOLOGY The present work was an analytical, cross-sectional, multicentre study conducted from 1 March to 31 October 2024 (eight months). . It was carried out in the departments of Brazzaville and Pointe-Noire, the administrative and economic capitals, respectively. The neurology departments and neurovascular care unit of the CHUB in Brazzaville, and the neurology, intensive care and emergency departments of the Loandjili and Adolphe Cise general hospitals in Pointe-Noire. The inclusion criteria for this study were as follows: all patients aged between 18 and 55 years, hospitalised in the specified departments and suffering from a first-time stroke confirmed on cerebral imaging.The data were collected on a pre-established survey form based on the admission registers of the selected departments and the patients’ medical records for the collection of sociodemographic, clinical, paraclinical and evolutionary information. The study incorporated the following variables:sociodemographic (age, sex, marital status, professional category, level of education, socioeconomic level, department of residence); clinical (traditional risk factors: hypertension, diabetes, alcoholism, smoking, sedentary lifestyle, obesity, heart disease; contextual risk factors: HIV infection, use of psychoactive substances (tramadol, Indian hemp, cocaine, etc.), cancers, haematological cancers, cervical trauma; paraclinical (type of stroke), etc.). The data were analysed using SPSS version 21. Categorical variables were compared using Pearson’s Chi-square test or Fisher’s exact test when expected frequencies were <5. For each significant bivariate association, unadjusted Odds Ratios (OR) and their 95% confidence intervals were calculated from 2×2 contingency tables. Variables with a p-value <0.20 in the bivariate analysis, as well as clinically relevant variables, were included in a multivariate logistic regression model to identify independent predictors of mortality. Adjusted Odds Ratios (aOR) with their 95% confidence intervals were reported. Statistical significance was set at p < 0.05. RESULTS During the course of the study, 553 patients were hospitalised for stroke, 290 in Brazzaville and 263 in Pointe-Noire. Of these patients, 232 met the inclusion criteria, giving a hospital frequency of stroke in young people of 42% for the two cities. The in-hospital rate in Brazzaville was 34.8% (101/290) and in Pointe-Noire 49.8% (131/263). The mean age of the patients was 46.8 ± 6.9 years, with extremes of 26-55 years. The sample included 123 male patients (53%) and 109 female patients (47%), resulting in a sex ratio of 1.1. The distribution of patients by age group is illustrated in (figure 1). The mean time taken to admit patients was 9.6 ± 0.6 hours, with extremes of 1 and 72 hours. The reasons for consultation are enumerated in (table I). The median Glasgow score was 15, with an interquartile range of 13-15. The (figure 2) illustrates the distribution of patients according to their state of consciousness on arrival, as assessed by the Glasgow score. The mean systolic blood pressure was 18.1 ± 2.6 cmHg, and the mean diastolic blood pressure was 11.7 ± 8.3 cmHg. Arterial hypertension was identified in 162 (69.8%) patients, and the distribution of patients according to the grade of hypertension is illustrated in (figure 3). The mean pulse oxygen saturation level was found to be 97.9% ± 6, with desaturation observed in only 14 (6%) patients. The imaging findings revealed that 92 (39.6%) subjects exhibited ischaemic strokes, while 140 (60.4%) cases demonstrated haemorrhagic strokes. The median NIHSS score was determined to be 15, with an interquartile range of 10-20. The distribution of patients according to the stage of stroke, as assessed by the NIHSS score upon admission, is illustrated in (figure 4). (Figure 5) illustrates the severity of haemorrhagic stroke as assessed by the ICH score.During hospitalisation, 94 (40.5%) patients experienced at least one complication, of whom thirty-one had pneumonia (33%) and a urinary tract infection (33%), twenty-five had pressure sores (26.6%) and five had a recurrence (5.3%). The distribution of traditional and contextual risk factors for stroke in the two cities is demonstrated in (tables II and III), respectively. The aetiologies of ischaemic strokes in the two cities are presented in (table IV) according to the TOAST classification.In all patients, the aetiology of haemorrhagic stroke was chronic arterial hypertension in 79.3% (n=111) of cases, and rupture of a vascular malformation in 4.3% (n=6). In 16.4% (n=23) of cases, the underlying cause of the condition was not established. In hospital, 57 patients died, representing a case-fatality rate of 24.5% for the two cities: 52.6% (n=30) in Brazzaville and 47.4% (n=27) in Pointe-Noire. In the course of subsequent observation, 12 patients passed away, 6 within the first month and 6 within the third month. Of the 163 survivors, 67 (41.1%) resided in Brazzaville and 96 (58.9%) in Pointe-Noire. Factors associated with case fatality in the univariate analysis are shown in Tables V and VI; independent predictors identified in the multivariate model are presented in Table VII. DISCUSSION 1. Frequency of stroke in young people The hospital incidence rate of stroke in young people in Brazzaville and Pointe-Noire was 42%, and in Abidjan in 2024, Sai et al. (27) observed a similar frequency, estimated at 46%. However, Mapouré et al. (22) reported a much lower frequency in Douala in 2016, at 15.26%. The study by Mapouré et al. (22) examined the spectrum of cerebrovascular disease, incorporating transient ischaemic attacks and subarachnoid haemorrhage. This discrepancy could be suggestive of a trend towards increased stroke incidence in young individuals within the sub-Saharan African region. A comparison of Brazzaville and Pointe-Noire reveals that the hospital incidence of stroke in young people is higher in Pointe-Noire (49.8%) than in Brazzaville (35.5%), although Brazzaville records more cases of stroke at all ages than Pointe-Noire.It is important to note that Brazzaville and Pointe-Noire have different socio-economic conditions. Brazzaville, the capital of the Congo, is an administrative city where the majority of employees are civil servants, as evidenced by the higher number of employees in Brazzaville in our study population. However, in Pointe-Noire, the coastal city and economic capital of the Congo, jobs are mainly filled by private companies, with a large number of subcontractors, indicating the precarious nature of this type of employment and the difficulties in finding a job (Smith, 2023). Consequently, the majority of patients in Pointe-Noire were unemployed, indicating a higher societal stress level in Pointe-Noire compared to Brazzaville, which is associated with the more prevalent harmful behaviours observed in Pointe-Noire, such as excessive alcohol consumption, substance abuse, and smoking. A comparison of the hospital incidence of stroke in young people in Brazzaville between 2022 and 2024 showed an increase in stroke, confirming the trend towards an increase in the incidence of stroke in young people (8).The risk factors most frequently identified in 2022 were a sedentary lifestyle and high blood pressure.Alcohol consumption concerned only almost a third of patients. Haemorrhagic stroke (60.3%) was the most common type of stroke, a finding that has been reported in several studies in sub-Saharan Africa (21, 22). This is probably due to the high prevalence and early onset of arterial hypertension in this region.However, in Europe, Aigner et al. (13) showed an overwhelming proportion of ischaemic strokes (94.6%), compared with 5.4% of haemorrhagic strokes. In Caucasian populations, a higher prevalence of atheromatous diseases has been observed, attributable to genetic factors and smoking patterns, which in turn result in a higher prevalence of coronary heart disease and thromboembolic diseases (14, 15). 2. Risk factors The classic risk factors in our study were dominated by arterial hypertension (69.8%), followed by alcohol consumption (39.2%), previous stroke in the family (25.4%) and sedentary lifestyle (22.4%).Smoking and diabetes mellitus were found at lower frequencies, 17.7% and 15.9% respectively. This finding aligns with the results of several African studies, which also identified hypertension, alcohol consumption, smoking, diabetes mellitus and a family history of stroke as the primary risk factors for stroke in young individuals (21, 27). Hypertension emerged as the most prevalent risk factor across these studies. However, a study conducted in Europe reported a higher prevalence of smoking compared with hypertension, which might explain the higher rate of atheromatous disease in their population (1, 2, 14, 15). The prevalence of arterial hypertension, sedentary lifestyle, diabetes mellitus and obesity was found to be higher in Brazzaville, while alcohol consumption, a family history of stroke and smoking were more common in Pointe-Noire. As previously indicated, the environment, socio-economic conditions and behaviours are not identical between Brazzaville and Pointe-Noire. The predominant contextual risk factors identified in our study were drug use (18.1%), medication (12.5%), and HIV infection (9.9%). These three factors were particularly prevalent in Pointe-Noire, where economic and recreational challenges have led to individuals seeking employment in the informal sector, which often exposes them to risk behaviours such as alcohol consumption and the increase in sexual partners. 3. Etiologies The aetiologies of ischaemic stroke were dominated by embologenic heart disease, principally dilated cardiomyopathy, followed to a lesser extent by atherosclerosis, as has been reported in several studies in Africa (10, 12, 25) .In addition, the high incidence of dilated cardiomyopathy is thought to be due to the late diagnosis of arterial hypertension and poor compliance with antihypertensive treatment.The incidence of atrial fibrillation was low in the present study. Research undertaken in Brazzaville has indicated a low prevalence of atrial fibrillation in young subjects and a propensity for its increased prevalence in older age groups (17, 18). The aetiology of haemorrhagic stroke was dominated by chronic arterial hypertension in 79.3% of cases, with a higher frequency observed in Pointe-Noire than in Brazzaville (23, 78). African studies have identified arterial hypertension as the most frequent cause of haemorrhagic stroke (7, 28). Conversely, rupture of a vascular malformation has only been found in a small proportion of cases (28). The paucity of paraclinical investigations, such as angioscanner or angio-MRI, in this context, is likely a contributing factor to these findings.Furthermore, in 20.6% of ischaemic stroke cases and 16.4% of haemorrhagic stroke cases, the aetiology remained undetermined. Conversely, North African and Western authors have reported a high frequency of undetermined (cryptogenic) causes of ischaemic stroke in young subjects (1, 7, 15).These observations underscore the challenges associated with conducting a comprehensive aetiological assessment in our setting, attributed to the limitations in the technical capacity and the substantial financial demands of these diagnostic procedures. 4. Vital prognosis and factors associated with death The mortality rate of patients during hospitalisation was found to be approximately 25%, with the majority of these deaths (approximately 80%) occurring in patients with haemorrhagic stroke. African studies have reported a death rate ranging from 21% to 29.1% (8, 23, 30, 32). The limited availability of neurological and neurovascular units has been identified as a contributing factor to the severity and mortality of stroke cases, along with socio-economic factors such as poverty (16). Conversely, Western studies have documented a lower hospital fatality rate ranging from 0.6% to 4.8% (3, 31). This relatively low case-fatality rate can be attributed to several factors. Firstly, developed countries have more widespread social security coverage, which facilitates easier and faster access to healthcare. Secondly, the presence of neurovascular units in most towns and cities ensures that patients can receive high-quality care, including intravenous thrombolysis and mechanical thrombectomy, and that neurosurgical management is available when necessary. As individuals age, there is a concomitant loss of neurons in the brain, which can result in cerebral atrophy. This atrophy can reduce the risk of cerebral involvement when an intracerebral haematoma expands. However, in young subjects, this margin of compensation for the expansion of the haematoma is not possible in the absence of cerebral atrophy. As a result, there is a higher incidence of intracranial hypertension, which carries an increased risk of cerebral involvement. This, in turn, leads to the excess lethality caused by haemorrhagic stroke in young subjects. The factors associated with death in our study were a low Glasgow score on admission, the presence of pneumopathy, desaturation and recurrent stroke. The univariate odds ratios observed for the lower categories of the Glasgow Coma Scale (GCS) score (9–7 and 6–3) were very high. This magnitude should be interpreted with caution, as these classes had small sample sizes and a highly skewed distribution, including the absence of survivors in the 6–3 group. Such configurations expose the researchers to sparse-data bias and complete separation phenomena, resulting in unstable estimates and wide confidence intervals. The adjusted values from multivariate logistic regression, which are less sensitive to these constraints, provide more robust estimates of the association between initial neurological severity and mortality and were preferred for interpretation. Several African studies have found coma to be a predictive factor for death (21, 23, 28, 31). Pneumopathy as a factor in death has also been reported by Andrianimaro (20) in Madagascar and Sai (27) in Abidjan. Furthermore, a study by Mandzou et al. (24) in Brazzaville reported a fatality rate of 54.2% in stroke patients with swallowing disorders, with bronchopneumonia identified as the primary cause of death. Additionally, Wang (33) reported stroke recurrence as a risk factor for death in 2016. In addition to the factors identified in our study, other variables have been implicated in the literature concerning all age groups, particularly a high NIHSS score, hyperglycaemia/diabetes, haemorrhagic stroke and prolonged hospital stay (33). A comparison between Brazzaville and Pointe-Noire revealed minimal discrepancy between the two cities in terms of case fatality rate. CONCLUSION The prevalence of stroke in young people has been observed to increase in the Congo, with a higher frequency recorded in Pointe-Noire. The study found that haemorrhagic strokes predominate, and that traditional risk factors such as arterial hypertension, a sedentary lifestyle, diabetes mellitus and obesity are more prevalent in Brazzaville, while in Pointe-Noire, the main risk factors identified were alcohol consumption, a family history of stroke and smoking.The analysis also highlighted contextual risk factors, including the use of toxic substances, medication and HIV infection. The prevalence of these three factors was found to be higher in Pointe-Noire.The aetiologies of ischaemic strokes were found to be similar in both towns, with emboligic heart disease being the primary cause, followed by atherosclerosis and chronic arterial hypertension. The fatality rate for strokes in young people was high, with haemorrhagic strokes accounting for the majority of deaths. CONFLICTS OF INTEREST: NO 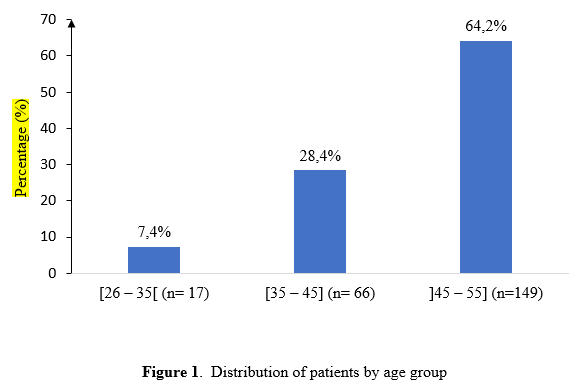 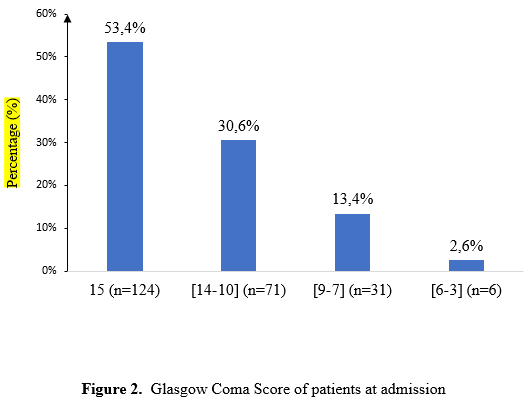 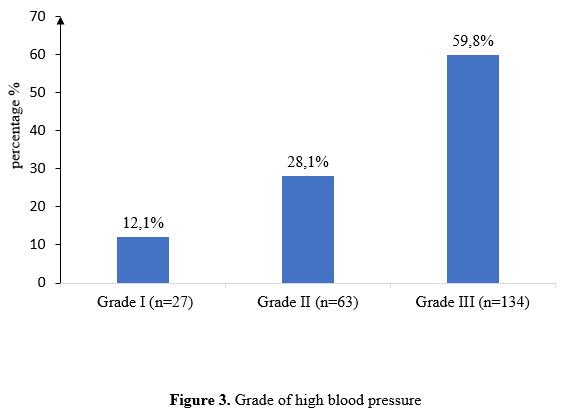 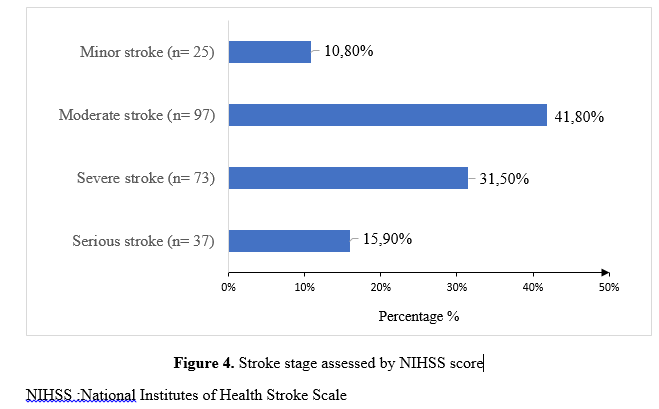 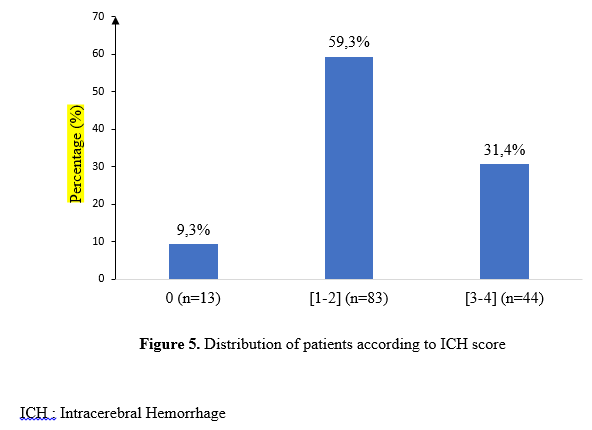 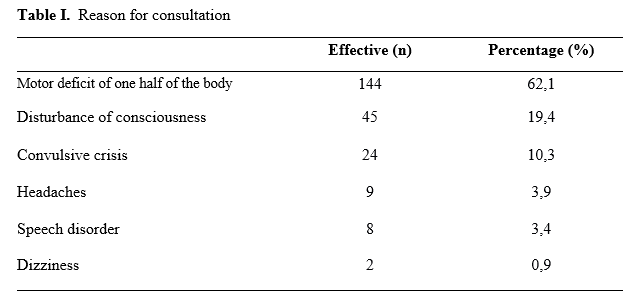 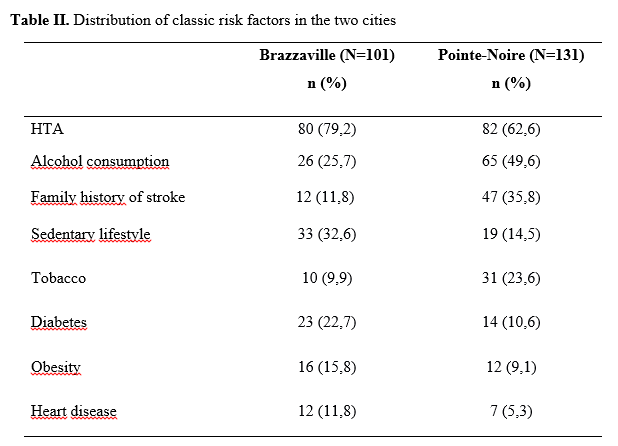 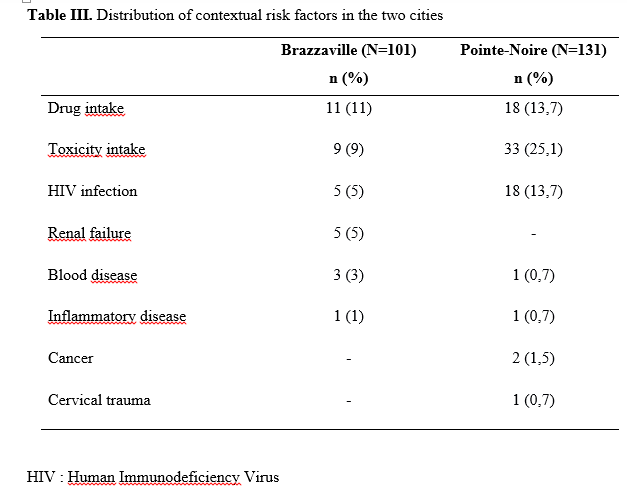 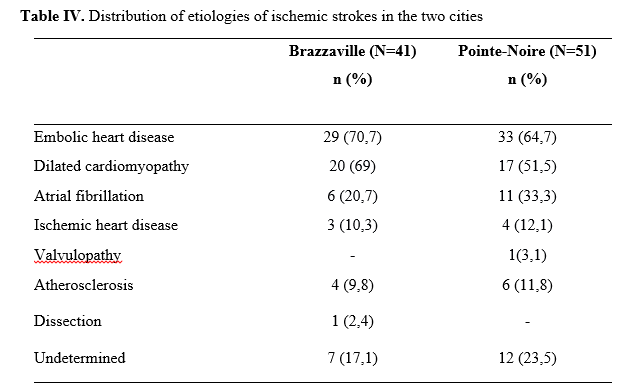 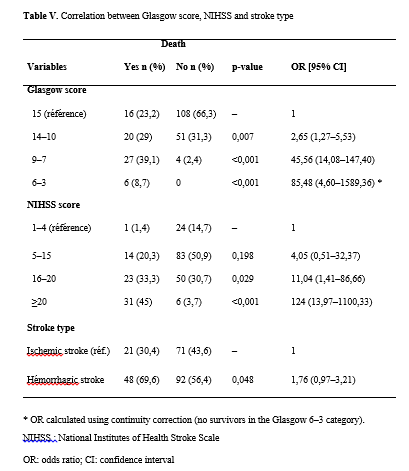  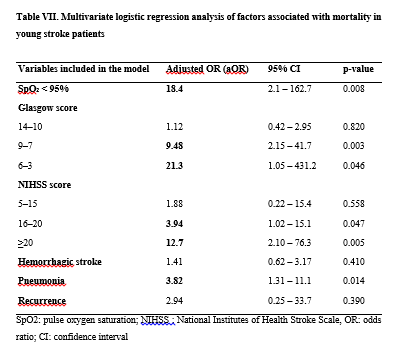 REFERENCES
|
© 2002-2018 African Journal of Neurological Sciences.
All rights reserved. Terms of use.
Tous droits réservés. Termes d'Utilisation.
ISSN: 1992-2647