CASE REPORT / CAS CLINIQUE
INTRACEREBRAL ARTERIOVENOUS MALFORMATION: DIAGNOSIS OF A CASE WITH COMPUTERIZED TOMOGRAPHY IMAGING
MALFORMATION ARTERIO-VEINEUSE INTRACÉRÉBRALE: A PROPOS D'UN CAS DIAGNOSTIQUE GRACE AU CT-SCANNER
- Department of Radiology, College of Medicine, University of Ibadan, Ibadan, and University College Hospital, Ibadan, Nigeria
- Division of Neurological Surgery, Department of Surgery, College of Medicine, University of Ibadan, Ibadan, and University College Hospital, Ibadan, Nigeria
ABSTRACT
Cerebral arteriovenous malformations (AVM) are rarely diagnosed and reported from our region of the world possibly due to the paucity (even unavailability) of the necessary imaging modalities especially digital subtraction angiography (DSA). In this report we present the CT features making for the confident diagnosis of a case of cerebral AVM, even in the absence of a DSA.
A 26-year-old man presented recently to us with history of headache not associated with any other general clinical or neurological deficits. An initial cranial contrast CT showed a right parietal 5 x 5cm parenchymal mass lesion with features highly suggestive of an AVM. The follow-up CT angiography later confirmed this lesion to be indeed a high grade AVM involving a high flow fistulous communication between the main branches of the right middle cerebral artery and the deep cerebral venous system.
Where there is no facility for DSA like in our own practice there are some specific CT scan imaging features that afford fairly accurate diagnosis of cerebral AVMs.
Key words: Arteriovenous malformation, Cerebral, CT angiography
RÉSUMÉ
Les Malformations artério-veineuses cérébrales (MAV) sont rarement diagnostiqués et déclarés de notre région du mondeen Afrique peut-être due à cause de la rareté (mêmeou indisponibilité) des modalités moyens d’imagerie nécessaire, en particulier l’angiographie numérique (DSA). Dans ce rapportt article, nous présentons les caractéristiques du CT-csanner qui a permis de faire confiance pour le diagnostiquer c d’un cas de MAV cérébrale , même en l’absence d’un DSA.
Un homme de 26 ans, avait récemment présenté à nous avec l’histoire des céphalées maux de tête isoléesn’est pas associé à aucun sans autre général, les ddééfficicits cliniques ou neurologiques. Un premier contraste tomodensitométrieCT scanner crânien ne a montré une lésion pariétale droite de 5 x 5cm lésion massive du parenchyme avec des caractéristiques très suggestives d’une MAV. Le suivi de Ll’angiographie CT tard a confirmé le caractère d’cette lésion à effet une MAV de grade haute qualité avecimpliquant une communication deà haut débit fistuleuse entre les branches principales de l’artère cérébrale moyenne droite et le système veineux profond cérébrale.
Lorsqu’il n’ya pas de facilité pourEn l’absence de DSA comme dans notre propre pratique il ya quelques spécifiques , le CT- scanner des fonctions d’imagerie qui offre nt un diagnostic assez précis de MAV cérébrales.
Mots clés: malformation artério-veineuse cérébrale, l’Angiographie CT
INTRODUCTION
Intracranial vascular malformations are congenital lesions due to alterations in the development of the arteriolocapillary network. Traditionally, they are divided into four types according to their histological characteristics: cavernous angiomas or cavernomas, arteriovenous malformations, venous angiomas, and capillary telangectasias[19]. An arterio-venous malformation (AVM) can be defined as a complex tangle of abnormal arteries and veins linked by one or more fistulas. The fistulas allow high-flow, rapid shunting and can induce arterial hypotension in adjacent areas of the brain due to the vascular steal phenomenon[11].Although AVMs are thought to result from developmental derangements of the angioarchitecture in the various stages of the intrauterine and postnatal vascular formation, other mechanisms such as trauma, occlusion of the venous sinus with the formation of neovascular collaterals, or occlusion of branch arteries with the formation of arterial collaterals also appear to play some roles.[11] It affects both the male and female gender in nearly equal proportions and it usually presents before the age of 40 years[11] Ten to 58% of patients have associated classic aneurysms[11]. The commonest presentation is intracranial haemorrhage and is usually as intracerebral or intraventricular bleed.[9,12]. Other modes of presentations include sub-arachnoid haemorrhage, and headache in 7-8 %, trigeminal neuralgia and hydrocephalus[18].
Catheter angiography, the digital subtraction angiography (DSA), is the gold standard imaging study for complete evaluation of intracranial vascular anomalies. But other computed imaging modalities of the current era, including computed tomography (CT) scan, computed tomography angiography (CTA), magnetic resonance imaging (MRI) and magnetic resonance angiography (MRA), can also give a fair diagnostic idea of many of such lesions when DSA is not available as in our own practice. In view of the rarity of such documents from our practice region we here present one case of cerebral AVM recently seen by us and which was diagnosed with the help of only cranial CT and CTA. We emphasize the specific neuroradiologic characteristics that can afford a confident CT diagnosis of a cerebral AVM even in the absence of the more definitive imaging studies.
CASE REPORT
A 26-year-old man was referred to the University College Hospital, Ibadan for cranial CT on account of persistent right sided headaches of 3 months duration which was not relieved by analgesics. His total clinical and neurological evaluation was otherwise unremarkable. So also was his family history unremarkable for the presence of vascular anomaly.
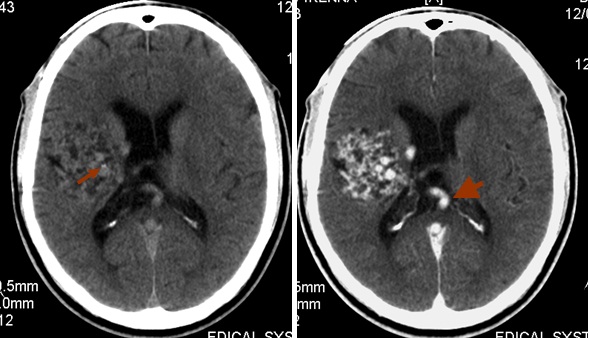
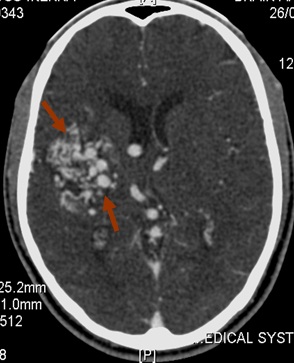
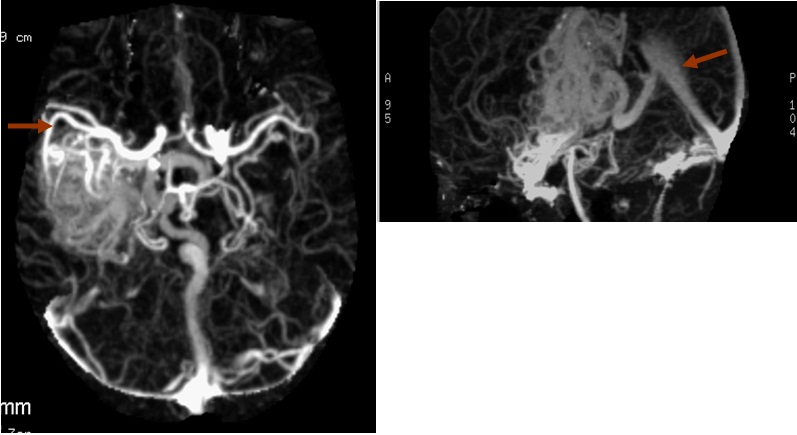
Computerized tomography of the brain was requested for the initial evaluation of this persistent headache. This screening brain CT showed an irregular area of mixed density with two small foci of hyperdensity (HU 80-87) in the right parietal region adjacent to the body of the right lateral ventricle. [Figure Ia] The lesion extended inferiorly to the temporal region and appeared to be in some relationship to the area of the middle cerebral artery. [Figure Ib] It showed serpiginous contrast enhancement with early venous filling of the straight sinus. These findings prompted a follow-up study with CT angiography being the only vascular study available in our practice. The CT angiography also showed the lesion to have increased vascularity with multiple irregular tortuous vessels of different sizes. [Figure II] These vessels include both arterial and venous circulation filling simultaneously in the region of the right parietal lobe, extending medially in the region of the thalamus and internal capsule. The Maximum Intensity Projection (MIP) images also showed that the distal or sylvian branch of the right middle cerebral artery was involved in the AVM [Figure III].
Due to many social and logistic constraints of our practice area cranial surgery for attempted resection of the vascular lesion could only be realized after about 8 months of clinical presentation. The surgical attempt was however also unsuccessful due to other logistic inadequacies intraoperatively. The post operative cranial CT findings were essentially the same except for the craniectomy defects in the right parietal bone with associated mild soft tissue swelling.
DISCUSSION
AVMs are the most frequent vascular malformations of the brain. They consist of vascular clusters that form direct arteriovenous shunts without any intermediary capillary network. The main presenting symptoms of AVMs of the brain are bleeding, seizures, progressive neurology deficit; and headaches [2]. Headache was a presenting symptom in this patient. The majority of malformations become symptomatic during the second or third decade of life and 80% become symptomatic by the end of the fourth decade. The yearly rate for the first haemorrhage is approximately 2% or 3% while that for recurrent bleeding is as high as 6% for the first year and 2% per year thereafter [11]. For each bleed there is an average risk of 10% mortality and 30% morbidity. Small AVMs seem to bleed more often than large ones [13].The diagnosis is usually initially suggested by computed tomography (CT), computed tomography angiography (CTA), magnetic resonance imaging (MRI), and magnetic resonance angiography (MRA), and is usually confirmed by catheter angiography which is the gold standard. A dynamic nuclear medicine scan is also a good way to demonstrate the existence of an AVM though this is rarely used. In this case report only a CT and CTA could be done. Plain X-ray films may show linear, circular, or punctuate areas within the skull; these are however not usually characteristic and their frequency has been as high as 30% [4] with enlargement of vascular grooves but this was not seen in this patient. Pre contrast CT scans will usually demonstrate patchy areas of increased densities ranging from 50 to 100+ Hounsfield Units (HU) interspersed with areas of low density[14] sometimes with calcifications, or it may sometimes be normal. Immediately after a bolus injection of contrast agent, CT will show serpiginous dilated afferent and efferent vessels, as well as enhancement of the nidus of the AVM in more than 90% of cases with both intravascular and extra vascular accumulation of contrast within the malformation [14]. This appearance was fairly well demonstrated in the index patient.
There are however some limits of plain cranial CT in the diagnosis of AVMs that are worthy of note. This may be especially more notable with AVMs that have bled or with small AVMs that may be undetectable by the resolution of the average CT scanner. The former factor could make the distinction between a tumor and an infarction more difficult to detect[21] This said, the CT angiographic picture is never the less frequently characteristic in that several tortuous arteries are regularly enlarged from two to five times the caliber of the normal cortical vessels.[2] On rare occasions, angiography done after bleeding will fail to show the malformation while another angiogram in a few weeks or months will occasionally show it.[2]
In our patient the CT images showed the participation of the internal carotid artery branches (the right middle cerebral artery) in this vascular malformation. In a review of 129 intracranial AVMs, external carotid supply to pial AVMs was found in 15.5%[22] which is seen more frequently with big AVMs located in the parieto-occipital region and, to a lesser degree, in the posterior fossa and temporal region. Catheter angiography, the gold-standard vascular imaging study, is invaluable to appreciate the factors of risks of hemorrhagic complications.[9,15,10.1] It is mandatory to confirm the diagnosis, to map the afferent arteries and efferent veins, to determine the speed of the blood flow through the malformation, and to decide the best alternative of treatment. A selective internal carotid and at least one vertebral angiogram should be done routinely. In most cases, selective external carotid angiography is also necessary, with super-selective catheterization of the branches that contribute to the dural component of the AVMs [8,16,7] However, this could not be done for our patient due to the unavailability of this imaging modality in our practice.
Magnetic resonance imaging is another important diagnostic study which could be invaluable in the diagnosis and grading of AVMs, as well as the follow-up of obliteration of the nidus, either after embolization or after radio surgery. Magnetic resonance angiography utilizing phase-contrast or, less optimally, time-of-flight, techniques on the other hand is able to accurately and non-invasively depict the arterial feeders and venous drainage of arteriovenous malformations of the brain [5]. Nussel and co-workers [17] showed important information was gained from MRA in 70% of cases examined. Huston and associates [6] also showed additional information on 3D-Phase Contrast MRA in depicting venous outpouchings that were obscured on conventional cerebral angiography.
The different alternatives of treatment include surgical resection or conservative therapy for small asymptomatic AVMs [6.23]. Embolization therapy is also employed where available using different materials like solid particles, detachable balloons, and some liquid agents; so also is radiotherapy [3] for some small AVM’s deep seated in the brain stem or basal ganglia. In conclusion, we report this case of an AVM with some degree of confidence using only conventional CT and CTA thus showing that where there is no facility for DSA like in our own practice there are some specific CT scan imaging features that afford fairly accurate diagnosis of cerebral AVMs.
REFERENCES
- BROWN RD, WIEBERS DO, FORBES GS: Unruptured intracranial aneurysms and arteriovenous malformations: Frequency of intracranial hemorrhage and relationship of lesions. J Neurosurg 1990 Dec,73(6):859-6315
- DEBRUN G M, BREITER S.N, Chapter 42 Arteriovenous Malformation Radiology on CD by Taverras and Ferrucci 2003
- DERUTY R, PELISSOU-GUYOTAT I, MOREL C, BASCOULERGUE Y, TURJMAN F. Reflections on the management of cerebral arteriovenous malformations. Surg Neurol. 1998 Sep;50(3):245-55;discussion 255-6
- DRAKE CG: Cerebral arteriovenous malformations: Considerations for and experience with surgical treatment in 166 cases. Clin Neurosurg. 1979;26:145-208.
- GARCIA M R, ALVAREZ H, GOULAO A, PRUVOST P, LASJAUNIAS P : Posterior fossa arteriovenous malformations: Angioarchiteclure in relation to their hemorrhagic episodes. Neuroradiology. 1990;31(6):471-5
- HUSTON J, RUFENACHT DA, EHMAN RL, WIEBERS DO: Intracranial aneurysms and vascular malformations: Comparison of time of flight and phase contrast MR angiography. Radiology. 1991 Dec;181(3):721-.30
- LASJAUNIAS P. MANELFE C, CHIU M: Angiographic architecture of intracranial vascular malformations and fistulas – pre therapeutic aspects. Neurosurg Rev 9(4):253,1986
- LASJAUNIAS P, PISKE R, TERBRUGGE K, WILLINSKY R: Cerebral arteriovenous malformations (C. AVM) and associated arteriovenous aneurysms (AA): Analysis of 101 C. AVM cases, with 37 AA in 23 patients. Acta Neurochir (Wien) 1988 91(1-2):26,
- MARKS MP, LANE B, STEINBERG GK, CHANG PJ: Hemorrhage in intracerebral arteriovenous malformations: Angiographic determinants. Radiology. 1990 Sep;176(3):807-13
- MIYASAKA Y, YADA K, OHWADA T, KITAHARA T KURATA A, IRIKURA K: An analysis of the venous drainage system as a factor in hemorrhage from arteriovenous malformation. J Neurosurg. 1992 Feb;76(2):239-43.
- MOHR, J.P. Current Concepts: Arteriovenous Malformations of the Brain in Adults. NEJM. Vol.340,No.23.June 10,1999.
- MUÑOZ F, CLAVEL P, MOLET J, CASTAÑO C, DE TERESA S, SOLIVERA J, DE QUINTANA C, TRESSERRAS P, RODRÍGUEZ R, BARTUMEUS F Current management of arteriovenous malformations. Retrospective study of 31 cases and literature review Neurocirugia (Astur). 2007 Oct;18(5):394-404;discussion 404-5.
- NAGATA S, MATSUSHIMA T, FUJII K, TAKESHITA I ET AL: Lateral ventricular arteriovenous malformations: Natural history and surgical indications. Acta Neurochir (Wien). 1991;112(1-2):37-46
- NEWTON HT, CRONQUIST S: Involvement of dural arteries in intracranial arteriovenous malformations. Radiology 1969 Nov,93(5):1071-8
- NEWTON HT, PORTS GD: Radiology of the skull and brain. Book 4, pp 2491-2565. St. Louis, CV Mosby, 1974
- NURCHI G, PELAGHI AE. FODDE M, AROMANDO P DETTORI P, CORADDU M: Rupture of a cerebral arteriovenous malformation due to a spontaneous occlusion of the venous drainage. Acta Neurol (Napoli). 1987 Oct-Dec;9(5-6):339-45
- NUSSEL F, WEGMULLER H, HUBER P: Comparison of magnetic resonance angiography, magnetic resonance imaging and conventional angiography in cerebral arteriovenous malformation. Neuroradiology. 1991;33(1):56-61
- OGILVY CS, STIEG PE, AWAD I, BROWN RD, JR., KONDZIOLKA D, ROSENWASSER R, ET AL. Recommendations for the management of intracranial arteriovenous malformations: a statement for healthcare professionals from a special writing group of the Stroke Council, American Stroke Association. Circulation 2001;103(21):2644-57
- SMITH ER, BUTLER WE, OGILVY CS. Surgical approaches to vascular anomalies of the child’s brain. Curr Opin Neurol. 2002 Apr;15(2):165-71
- STELZER K, GRIFFIN B, ESKRIDGE J, EENMAA J, MAYBERG M, HUMMEL S, WINN HRL: Results of neutron radiosurgery for inoperable arteriovenous malformations of the brain. Med Dosim 1991 Sep;16(3):137-41
- TERBRUGGE KG, SCOTTI G, ETHIER R, MELANÇON D, TCHANG S, MILNER C: Computed tomography in intracranial arteriovenous malformations. Radiology. 1977 Mar;122(3):703-5
- VAQUERO J, LEUNDA G, MARTÍNEZ R, BRAVO G: Cavernomas of the brain. Neurosurgery. 1983 Feb;12(2):208-10.
- VINUELA F, DION JE, DUCKWILER G, MARTIN NA, LYLYK P, FOX A, PELZ D, DRAKE CG, GIRVIN JJ, DEBRUN G: Combined endovascular embolization and surgery in the management of cerebral arteriovenous malformations: Experience with 101 cases. J Neurosurg. 1991 Dec;75(6):856-64.
|
|