
|
|
|
CLINICAL STUDIES / ETUDES CLINIQUES
MANAGEMENT OF PATIENTS WITH SEVERE HEAD INJURIES
E-Mail Contact - SEMPLE Patrick Lyle :
psemple@uctgsh1.uct.ac.za
Summary At Groote Schuur Hospital, head injured patients are managed by the Neurosurgical Department. A retrospective study was undertaken to determine whether the intensive management of head injuries with a low Glasgow Coma Scale (GCS) on admission is justiFied. One hundred and five patients admitted during 1990 with a GCS of 8/15 or less were grouped on the basis of their GCS following resuscitation. Thirty four patients were admitted with a GCS oF 3/15 and fifty two patients were admitted with GCS of 6/15-8/15. The outcome of these patients was then analyzed; the findings suggesting that those patients who have been adequately resuscitated, and have had an intracranical haematoma evacuated, but still present with a GCS 5/15 or less at 6 hours post injury have such a poor prognosis that high tech intensive care may not be justified. Resume Au Groote Schuur Hospital, les traumatises craniens sont pris en charge par le Department de Neurochirurgie. Une etude retrospective a ete entreprise pour savoir si les soins intensifs etaient justifies pour les patients qui a leur admission, presentaient un faible niveau de « Glasgow Coma Scale » (GCS); 105 patients hospitalises en 1990 avec un GCS egal ou inferiur a 8/15, etaient groupes en se basant sur leur GCS apres reanimation; 34 avaient un GCS de 3/15, 7 de 4/15, 12 de 5/15, et 52 de 6/15 a 8/15. Le devenir de ces patients a ete analyse. II en resulte que les patients qui, malgre une reanimation correcte et une evacuation de leur hematome intra-cranien, avaient encore six heures apres le traumatisme, un GCS egal ou inferieur a 5/15, le pronostic etait tellement mauvais que la pratique des soins intensifs de haute technicite ne semblait pas justifiee. Keywords : Severe head injury, Outcome, Glasgow Coma Scale, computerized Tomography INTRODUCTION The management of patients with severe head injuries continues to be a major neurosurgical challenge. With improved monitoring and more effective therapeutic modalities the mortality has decreased but the long term morbidity remains very high. 1,4,9,13 This is even more so in third world countries where there are severe financial and logistical constraints on therapeutic 13 Accurate prediction of outcome would enable the medical team to counsel the family, and to make clinical and legal decisions on a sound basis.5 Numerous studies have attempted to predict outcome of severe head injuries at an early stage2,3,6J,8,10,ll,12,15,16,18,19,21 possible factors in prediction that appear to be of importance include age, clinical coma scales, computer tomography findings, electrophysiological responses and cerebral blood flow. At Groote Schuur Hospital all head injuries requiring admission are managed by the neurosurgical department. Our current policy is that all head injuries receive intensive management, despite the fact that with an increasing patient load the available intensive care resources remain limited. The aim of this study was to determine whether high cost intensive management of all severe head injured patients is justified in terms of the ultimate outcome. PATIENTS AND METHODS In 1990, 105 patients admitted to Groote Schuur Hospital following a head injury had Glasgow Coma Scale values of less than 8/15 after resuscitation. All patients received the following treatment – resuscitation on admission; a CT scan of the head; management in an intensive care unit which included intubation, ventilation, pC02 control, regular electrolyte assessment and sedation. The Glasgow Outcome Scale 14 was used to evaluate the outcome at follow-up. The result was described as favourable if there was a moderate disability or good outcome. An unfavourable outcome was recorded if there was death; a persistent vegetative state or severe disability. The mean period of follow up was 6 months. RESULTS The study showed a preponderance of young male trauma patients with 87% of the patients being male, and 65% being under 35 years of age. The most common aetiology was pedestrian motor vehicle accident (33%); followed by blunt assault (22%); driver or passenger motor vehicle accident (15%) and sharp assault or missile injury (8%) each. 44% of the patients suffered an associated injury, most commonly ormopaeciic in nature, 11% of the patients sustained multiple trauma, having 3 or more injuries and 6% had evidence of hypovolaemic shock on admission. The results of the different GCS groups were then analyzed. Thirty-four patients had a GCS of 3/15 after resuscitation. Thirteen of these patients had head injuries of such severity that they died prior to CT scan being obtained. Of the 19 patients on whom a CT scan was done, 10 showed features in keeping with a diffuse cerebral injury. Four had an isolated intracranial haematoma – either a subdural or extradural haematoma. Three patients had knife tracts and two patients gunshot injuries. 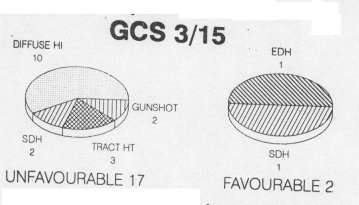 Figure 1 There were 7 patients in the GCS 4/15 group and 5 were investigated. One patient had an angiogram which showed cerebral circulatory arrest and four had a CT scan. Two of these four had features of diffuse cerebral injury and two had acute subdural haematomas. All of the patients in this group had an unfavourable outcome regardless of whether they had diffuse cerebral injury or an isolated intracranial haematoma. 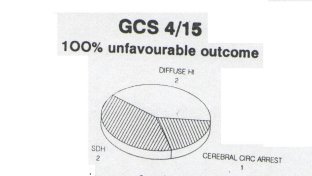 Figure 2 Twelve patients presented with a GCS of 5/15. On Ct scanning six had -features of a diffuse cerebral injury, four had a subdural or extradural haematoma and two had contusions. All the patients with features of a diffuse head injury on CT scan had a unfavourable outcome. However, 66% of patients with an isolated intracranial haematoma had a favourable outcome. 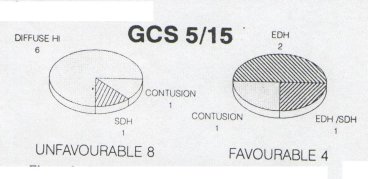 Figure 3 Nineteen patients presented with a GCS of 6/15. On CT scanning twelve showed evidence of diffuse cerebral injury; five had an isolated extradural or subdural haernatoma; one of a knife tract injury and one was normal. Nine of the twelve patients were found to have a good outcome or minor disability. Patients with isolated intracranial haeniatomas had a favourable outcome in 3 out of 5 cases. 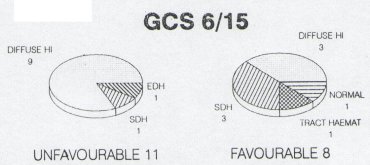 Figure 4 There were 33 patients with a GCS of seven or eight, and thirty-two of these had a CT scan. Findings on the CT scan were eleven subdural haematomas, eight contusions; five extradura. haematonias, seven diffuse cerebral injuries; and one was normal. Five of 7 patients with features of a diffuse cerebral injury on CT scan, either died remained in a persistent vegetative state or had a severe disability. Seventeen of 21 patients with an isolated intracranial haematoma had a favourable outcome. 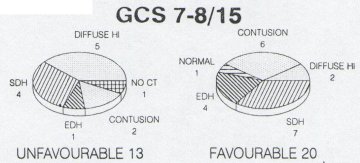 Figure 5 DISCUSSION The aim of most head injury studies has been to determine if there is a group of patients whose injury is so sever that they will not respond to the therapeutic modalities available.l5 If accurate, early prognosis can be made, the available resources can be used to benefit those patients who are more likely to have a favourable outcome.6 The danger which remains, however, is that a patient who may make a significant recovery does not receive optimal therapy. 10,12,16,21 The results of this study suggest that severely head injured patients with a GCS of <5 after resuscitation and with features of diffuse cerebral injury or CT scan have an unfavourable outcome in 100% of cases. If the GCS is >5 there is, however, a favourable outcome in 40%. In patients with isolated intracranial haematornas there is an expected poorer outcome in patients with a lower GCS. Nevertheless, there is a favourable outcome in a significant percentage of patients in GCS groups namely 50% <5 and 71%> 5. Thus there appears to be a group of patients whose head injury is so severe and whose prognosis is so poor, that no intensive management may be justified. They are the patients who once fully resuscitated and on being assessed 6 hrs post injury have a GCS <5 and show no isolated intracranial haematoma on CT scan.
Based on the findings of our study and others in the literature a suggested management protocol to severely head injured patients is illustrated in fig 6.
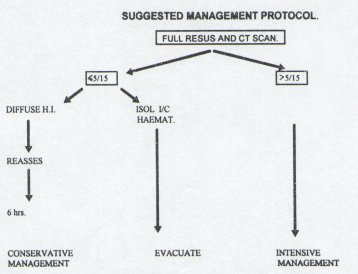 Figure 6 CONCLUSION The authors recognise that this is a small study. It does, however, indicate that based on GCS readings and CT scan performed after resuscitation, there is a group of patients whose head injury is so severe that they will not benefit from intensive management. Limited resources could be more utilised to benefit patients who are more likely to have a favorable outcome. REFERENCES
|
© 2002-2018 African Journal of Neurological Sciences.
All rights reserved. Terms of use.
Tous droits réservés. Termes d'Utilisation.
ISSN: 1992-2647