CASE REPORT / CAS CLINIQUE
METASTATIC PROSTATE CARCINOMA MIMICKING MENINGIOMA
METASTASE D'UN CARCINOME PROSTATIQUE EVOQUANT UN MENINGIOME INTRACRÂNIEN
- Neurology, Mayo Clinic Scottsdale Scottsdale, Arizona
- Medical Oncology, Mayo Clinic Scottsdale Scottsdale, Arizona
- Departments of Neurological Surgery, Mayo Clinic Scottsdale Scottsdale, Arizon
- Neuroradiology, Mayo Clinic Scottsdale Scottsdale, Arizona
- Radiation Oncology, Mayo Clinic Scottsdale Scottsdale, Arizona
E-Mail Contact - DRAZKOWSKI Joseph F. :
ABSTRACT
We report the case of a large dural-based adenocarcinoma of the prostate clinically and radiographically mimicking a meningioma. A 57-year-old male presented to our institution for the first time with a progressive history of gradual hemiparesis, seizures and headache. Imaging revealed a very large extraparenchymal lesion with significant mass effect initially felt to be consistent with a meningioma. The patient underwent successful surgical resection. The pathology revealed metastatic adenocarcinoma of the prostate. The patient received postoperative radiotherapy and subsequent imaging demonstrated no evidence of disease progression. We discuss the implications of intracranial mass lesions in patients with prostate cancer and review of the literature.
RESUME
La xanthomatose cérébro tendineuse est une maladie héréditaire rare caractérisée par des taux de cholestérol élevés au niveau du plasma et du cerveau. Nous rapportant le cas d’une patiente de 24 ans, hospitalisée pour une démence progressive et des troubles de la marche. Nous rapportons le cas d’une métastase d’un adénocarcinome de la prostate évoquant radiologiquement un méningiome chez un patient de 47 ans.
Keywords : Carcinome, méningiome, métastase, prostate, épilepsie, tumeur, carcinoma, meningioma, metastatic, prostate, seizure, tumor
INTRODUCTION
Prostate adenocarcinoma rarely invades the brain parenchyma, but has significant potential for metastatic involvement for bone and other organ systems [5]. Rarely, elderly males with known prostate carcinoma have been reported to have intracranial extraparenchymal lesions consistent with metastatic disease [2,4]. These have been identified during routine cancer surveillance and at autopsy [2,4,6,7]. While the radiographic appearance of prostate carcinoma can simulate the appearance of intracranial meningiomas, such metastatic deposits are less common than other metastatic tumors and incidental meningiomas in that age group [3,7]. We report an unusual case of a relatively young patient who developed progressive neurological symptoms due to a very large intracranial dural-based prostate metastasis and discuss subsequent evaluation and treatment.
CASE MATERIAL
This 57-year old man presented to our emergency department with a several week history of left-sided headache, right hemiparesis and new onset partial epilepsy. A radical retropubic prostatectomy for adenocarcinoma was performed three years before at an outside hospital prior to presentation to our institution. Prior treatment included radiation therapy for left eighth rib metastasis and lupron shortly after the initial diagnosis at the outside institution. No records were available upon his presentation, but the patient had had no subsequent care since the initial therapy due to noncompliance.
The patient was unable to undergo a magnetic resonance imaging (MR) study. A computerized tomography (CT) scan demonstrated a large enhancing extra-axial left frontal parietal mass measuring 9 x 3 cm (Fig. 1). Dexamethasone and phenytoin were started shortly after admission to the hospital. Cerebral angiography demonstrated that the principal blood supply to the tumor was from enlarged scalp vessels with little intra-axial supply. The tumor was noted to be moderately vascular and the external carotid artery feeding vessels were successfully embolized (Fig. 2). A left frontal parietal craniotomy and resection of a large dural based extra-axial mass was performed (Fig. 3). There was no intraparenchymal involvement of the tumor. The pathology confirmed the diagnosis of metastatic prostate adenocarcinoma. The postoperative course was uneventful with no further seizures and improvement of the hemiparesis.
A metastatic workup demonstrated a prostate specific antigen of 83.4 ng% and the previously radiated bony involvement in the left eighth rib. No additional sites of metastatic involvement were identified. The patient underwent external beam radiotherapy to the brain of 3740 cGy without difficulty and is receiving ongoing casodex and lupron therapy. Followup evaluation has demonstrated no evidence of recurrence or disease progression.
DISCUSSION
This case represents an unusual presentation of symptomatic metastatic prostate adenocarcinona mimicking a meningioma in a young patient [4]. As was true in our case, prostate adenocarcinoma rarely involves the brain parenchyma [1,3,5,7]. The radiographic appearance of prostate cancer can mimic those features seen in meningiomas [2,4,6,7]. The hyperostosis, as seen in this case, is similar to that seen in meningiomas and appears blastic as opposed to lytic [4,6,7]. The enhancement pattern on CT scanning seen in metastatic prostate carcinoma to the dura in this case is similar to that seen in intracranial meningiomas. Common to meningiomas, the blood supply to this tumor was primarily from the extraparenchymal circulation. However, the angiographic findings in this case were somewhat unusual for a meningioma in that most of the blood supply to the tumor was from enlarged scalp vessels and there was very little vascular supply from the middle meningeal artery. Preoperative embolization in this patient was very useful given the large size of the tumor.
Depending upon the extent of the systemic disease, the prognosis for patients with metastatic prostate adenocarcinoma to the brain can be significantly better than other types of metastatic cancer involving the brain [1,3,5]. However, it can be acutely life threatening if not recognized and aggressively treated [6]. This case illustrates a patient with otherwise stable systemic disease presenting with progressive neurologic deterioration due to previously undiagnosed metastatic intracranial disease. Prostate cancer, when detected and treated early, can be very effectively controlled. Intracranial masses in this patient population need to be considered for timely evaluation and treatment. Appropriately, incidentally discovered intracranial meningiomas are often initially observed in many patients before definitive surgical intervention is pursued. While this particular case demonstrated a very large tumor for which surgical intervention at the time of initial presentation was appropriate, a smaller asymptomatic mass in this clinical setting could potentially be mistaken for a benign lesion. This report illustrates the need for the continued awareness that malignant lesions can masquerade as benign lesions, thus emphasizing the need for early and definitive intervention.
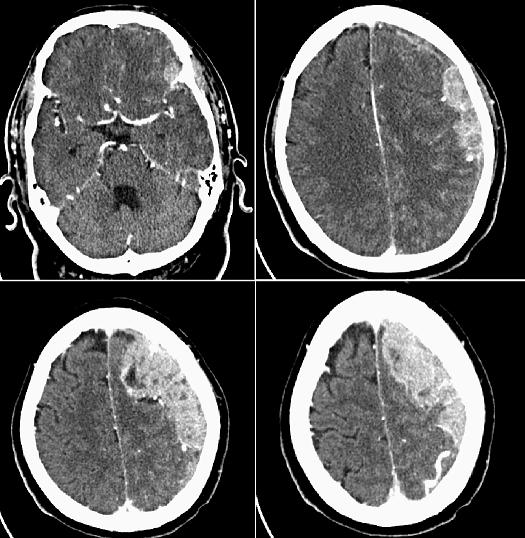
Figure 1
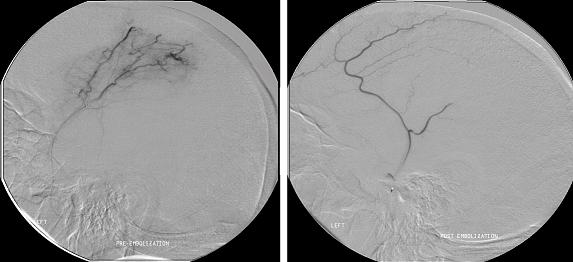
Figure 2
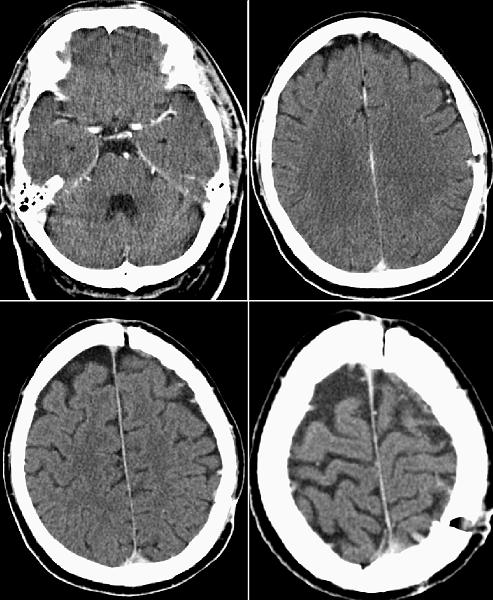
Figure 3
REFERENCES
- KWEE IL, NAKADA T, ST JOHN JN. Triple fossa metastasis of prostate cancer. Neurosurg 1983; 13:584-586
- LINDSBERG PJ, TATLISUMAK T, TIENARI J, BRANDER A. Bilateral sphenoid wing metastasis of prostate cancer presenting with extensive brain edema. European J of Neuro1999; 6:363-366
- LIPPMAN SM, BUZAID AC, IACONO RP, STEINBRONN DV, STANISIC TH, RENNELS MA, GAREWALL HS, AHMANN FR. Cranial metastases from prostate cancer simulating meningioma: report of two cases and review of the literature. Neurosurg 1986; 19:820-823
- LUDWIG HC, BEHNKE J, MARKAKIS E. Brain metastases in neurosurgery: indications, surgical procedures and outcome. Anticancer Res 1998; 18(3C):2215-2218
- NUSSBAUM ES, DJALILIAN HR, CHO KH, HALL WA. Brain metastases. Histology, multiplicity, surgery and survival. Cancer 1996; 78(8):1781-1788
- OLIVERIA MA, ARAUJO JF, BALBO RJ. Cerebral metastases from prostatic neoplasm simulating meningioma. Report of a case. Arch of Portuguese Neuro 1993; 51:251-252
- TREMONT-LUKATS IW, BOBUSTUC G, LAGOS GK, LOLAS K, KYRITSIS AP, PUDUVALLI VK. Brain metastasis from prostate carcinoma. The M.D. Anderson Cancer Center experience. Cancer 2003; 98:363-368