
|
|
|
CASE REPORT / CAS CLINIQUE
MYASTHENIA GRAVIS WITH MOTOR NEURONE DISEASE
MYASTHENIA GRAVIS ET MALADIE DU MOTONEURONE
E-Mail Contact - PARVAIZ A. Shah :
parvaizshah11@gmail.com
ABSTRACT A 56 year old male presented with features of easy f atiguability, episodic hoarseness and nasal quality of voice accompanied by nasal regurgitation of liquids for three years. Neurological examination revealed lingual atrophy with fasciculations,pyramidal tract signs and features of neuromuscular junction dysfunction. Moreover, CT scanning of thorax revealed thymic enlargement. The co-occurrence of myasthenia gravis with motor neurone disease is being reported for its rarity. KEY WORDS: Amyotrophic lateral sclerosis, False positive , Myasthenia gravis ,Progressive bulbar palsy. INTRODUCTION Myasthenia gravis, relatively an uncommon neurological disorder tends to be commoner in females than males with a ratio of 3:2.It usually occurs in third and fourth decades in females whereas incidence peaks in fifth and sixth decades in males.Various disorders associated with myasthenia gravis include pure red cell aplasia, thymoma/thymic hyperplasia, perniciousanaemia, vitiligo, pemphigus, alopecia, dysthyroidism, hypercalcemia, Cushings syndrome, hypogammaglobunemia, rheumatoid arthritis, lupus erythromatosus, Issac,s syndrome, polymyositis, various genetic (acetylcholine receptor abnormalities) and antistriatal antibodies[1].Immunological disorders, neuromuscular transmission abnormalities and acetylcholine receptor antibodies have been rarely reported with motor neurone disease[2,3,4,5].Association of myasthenia gravis with amyotrophic lateral sclerosis, although reported, is extremely rare[6,7,8].Here,we report a patient of amyotrophic lateral sclerosis with progressive bulbar palsy who presented simultaneously with clinical,serologic,electrophysiologic and pharmacological features of myasthenia gravis CASE A 56 year old male, an Islamic clergy man, presented with complaints of easy fatiguability and episodic hoarseness of voice(dysphonia) with nasal quality for three years. Patient noticed fatiguability after traversing a distance of about 500 meters.Moreover,he would observe hoarseness of voice with nasal quality and nasal regurgitation of liquids after delivering a sermon. The frequency and severity of his symptoms had worsened for the past one year.However,there was no diurnal variation of his symptomatology. Except for being hypertensive for the last six years, his medical history was unremarkable. There was no electrophysiological evidence of peripheral neuropathy but electromyography of appendicular musculature revealed neurogenic pattern. CT Scan of thorax revealed thymic enlargement(noninvasive type).MRI Scan of brain as well as that of craniovertebral junction was unremarkable. However, serum acetylcholine receptor antibody was positive. Other laboratory parameters including hemogram, thyroid function tests, basline serum chemistry, serum calcium, muscle enzymes and immunoglobulin profile were within normal range. With constellation of aforementioned clinical and laboratory parameters,a diagnosis of motor neurone disease (amytrophic lateral sclerosis) with myasthenia gravis(Osserman’s class 11) was entertained.Patient was instituted treatment for myasthenia gravis(Pyrodostigmine 60mg,Q.I.D & Prednislone 60mg O.D) with remarkable improvement in his symptomatology i.e.nasal twang/regurgitation and appendicular motor power.Patient did not give consent for thymectomy.Seven weeks after initial diagnosis,patient developed worsening of his motor symptoms after a febrile illness which dramatically improved after administration of antibiotics and plasmaphresis.During follow up,he developed diabetes mellitus which was satisfactorily managed by insulin administration.At last,patient succumbed to aspiration pneumonia about fourteen months after the initial diagnosis and expired. Discussion Myasthenia gravis, a postsynaptic neuromuscular junction dysfunction, usually presents with episodic motor weakness with worsening of symptoms after voluntary motor activity. The diagnosis of myasthenia gravis is established by cardinal clinical features which may be corroborated by positive Tensilon/Neostigmine test, repetitive nerve stimulation test and presence of serum acetylcholine receptor antibodies. Repetitive nerve stimulation test is positive in about 50% of myasthenic patients if peripheral muscles are sampled. The yield may be 80% if proximal muscles like nasalis is sampled. However, a negative repetitive test does not exclude the diagnosis of myasthenia gravis. Similarly, a false positive Tensilon/ neostigmine test has been reported in amyotrophic lateral sclerosis and polymyositis[9].The patient under discussion did not fulfill the requisite criteria for the diagnosis of polymyositis. He had evidence of bilateral lower motor neurone involvement of lingual musculature. In view of normal neuroimaging of brain and craniovertebral junction, a structural lesion involving brainstem especially medulla or hypoglossal nerve along its course was ruled out.The combination of upper and lower motor neurone features in appendicular musculature, bulbar palsy, clinical as well as electrophysiological evidence of neuromuscular junction dysfunction and presence of acetylcholine receptor antibody substantiates the diagnosis of myasthenia gravis with amyotrophic lateral sclerosis.The occurrence of false positive myasthenia gravis with amyotrophic lateral sclerosis is negated by improvement in his symptomatology after administration of anticholine-esterases, steroids and plasmaphresis. conclusion Our patient had presented with features of myasthenia gravis with motor neurone disease. Simultaneous occurrence of myasthenia gravis and motor neurone disease may result from the common aberrant immune process as one of the presumed causative factors for amyotrophic lateral sclerosis is believed to be the pathological immune process. Moreover, some of the electrophysiological features of amyotrophic lateral sclerosis may be partly attributed to the presence of acetylcholine receptor antibody. 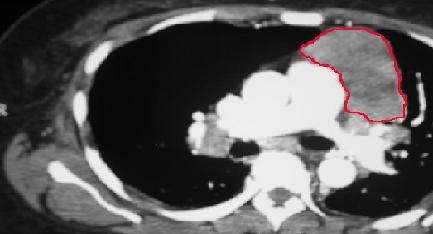 Fig 1 CT Scan of chest showing enlarged thymus gland (Thymoma) REFERENCES
|
© 2002-2018 African Journal of Neurological Sciences.
All rights reserved. Terms of use.
Tous droits réservés. Termes d'Utilisation.
ISSN: 1992-2647