
|
|
|
CASE REPORT / CAS CLINIQUE
NEUROENDOSCOPIC TRANSVENTRICULAR TREATMENTT OF CYSTIC CRANIOPHARYNGIOMA: A CASE REPORT
TRAITEMENT TRANSVENTRICULAIRE NEUROENDOSCOPIQUE D'UN CRANIOPHARYNGIOME KYSTIQUE : CAS CLINIQUE
E-Mail Contact - SALEM-MEMOU Sidi :
fkct@hotmail.com
ABSTRACT Background Craniopharyngiomas are rare benign epithelial tumours that develop in the sellar and suprasellar region. The often intimate relationships of the tumour with delicate neurovascular structures and the frequent absence of a cleavage plane prompted neurosurgeons to seek less aggressive approaches as an alternative to surgical excision. The transcortical transventricular neuroendoscopic approach represents an interesting option for cystic or predominantly cystic forms, which represent the majority of craniopharyngiomas. Case presentation We report the case of a 4-year-old girl who was brought into the emergency room with signs of severe intracranial hypertension. Brain magnetic resonance imaging (MRI) showed a large cystic lesion of the sellar and suprasellar region compressing and occupying the third ventricle with bi-ventricular hydrocephalus. The patient was urgently treated by transventricular endoscopy with draining of the cyst and extensive marsupialisation in the ventricle. The contents of the cyst were yellowish, oily and filled with shiny fragments. The postoperative course was marked by a good improvement in clinical symptoms. The control MRI at 27 months showed sagging of the cyst with significant reduction in its size. Conclusion In this case, the pure transventricular neuroendoscopic approach was simple and safe with good long-term results. Keywords: craniopharyngioma, cyst, neuroendoscopy, transventricular approach RÉSUMÉ Introduction Les craniopharyngiomes sont des tumeurs épithéliales bénignes rares qui se développent dans la région sellaire et suprasellaire. Les relations souvent intimes de la tumeur avec des structures neurovasculaires importantes et l’absence fréquente d’un plan de clivage ont incité les neurochirurgiens à rechercher des approches moins agressives comme alternative à l’exérèse chirurgicale. L’approche neuroendoscopique transventriculaire transcorticale représente une option intéressante pour les formes kystiques ou à prédominance kystiques, qui représentent la majorité des craniopharyngiomes. Observation Nous rapportons le cas d’une fillette de 4 ans qui a été amenée aux urgences avec des signes d’hypertension intracrânienne sévère. L’imagerie par résonance magnétique cérébrale (IRM) a montré une importante lésion kystique de la région sellaire et suprasellaire comprimant et occupant le troisième ventricule avec une hydrocéphalie bi-ventriculaire. La patiente a été opérée en urgence par endoscopie transventriculaire avec drainage du kyste et large marsupialisation dans le ventricule. Le contenu du kyste était jaunâtre, huileux et rempli de particules brillantes. L’évolution postopératoire a été marquée par une bonne amélioration de la symptomatologie clinique. L’IRM de contrôle à 27 mois a montré un affaissement du kyste avec une réduction significative de sa taille. Conclusion Pour ce cas, l’approche neuroendoscopique transventriculaire pure a été simple et sûre avec un bon résultat à long terme. Mots-clés : craniopharyngiome, kyste, neuroendoscopie, voie transventriculaire. BACKGROUND Craniopharyngiomas are rare benign epithelial tumours, originating in the pituitary stem or pituitary gland and developing in the sellar and suprasellar region. Their treatment is still subject to debate (12). Radical surgery makes sense in the face of this benign extracerebral tumour. However, this is major surgery, given the deep localisation of the tumour and its sensitive anatomical relationships with the vasculonervous structures of the base. The totally solid forms of craniopharyngioma represent only 10%, while the cystic or predominantly cystic forms can reach 60% (4,15). These cysts can become large, compressing the optic pathways and the hypothalamus and lead to obstructive hydrocephalus. In these cases, to avoid surgical morbidities, alternative surgical strategies aimed at shrinking the cyst may be used (8). The transcortical transventricular neuroendoscopic approach represents an interesting alternative for these cystic or predominantly cystic forms. In this article, we report a case of cystic craniopharyingioma urgently treated by pure transventricular endoscopic route without catheter placement. In this case, the pure transventricular neuroendoscopic approach was simple and safe with good long-term results. CASE PRESENTATION A 4-year-old girl with no pathological medical history was received in the emergency room of our hospital for progressive disturbances of consciousness. Questioning the parents revealed a history of severe headache, nausea, visual disturbances and behavioral disturbances for the past 2 months. The physical examination found a patient with disturbed consciousness (Glasgow Coma Scale 9/15) without evidence of neurological localization. Magnetic resonance imaging (MRI) of the brain showed a large cystic lesion of the sellar and suprasellar region extended under the forehead and behind, compressing and occupying the third ventricle with obstruction of the Sylvius aqueduct (Fig. 1A). This cystic lesion was hyperintense on the T2 sequences (Fig. 1A, 1B, 1C) and T1 (Fig. 1D), and obstructed the two Monroe foramens resulting in bi-ventricular hydrocephalus with significant transependymal resorption (Fig. 1B, 1C). The biological and hormonal results were normal. In the face of this radio-clinical picture, an emergency endoscopic operative decision was made. After general anesthesia, the patient was placed in supine position, with the head in neutral position slightly raised and fixed. Through a drill hole 3 cm from the midline and 1 cm anterior to coronal suture, the right frontal horn was approached by a rigid endoscope with a 30° lens. In the lateral ventricle cavity, the dome of the cyst was identified, filling the Monro foramen (Fig. 2A). A large opening of the cyst was made using monopolar coagulation and scissors, letting it escape under strong pressure; yellowish, oily liquid rich in shiny fragments (Fig. 2B, 2C and 2D). Abundant and progressive washing made it possible to obtain complete drainage of the cystic contents. Then, the endoscope was introduced into the cyst through the stoma, which allowed visualization of the yellowish deposits on the internal wall of the cyst and to drain as much as possible by rinsing (Fig. 2E and 2F). No communication between the cyst and the basal cisterns was made due to the absence of anatomical landmarks. Collapsing of the cyst and release of the Monro foramen were evident when the endoscope was removed. The closure was carried out according to the conventional technique. Drug treatment with corticosteroids was administered postoperatively. The immediate postoperative follow-up was simple with a clear improvement in clinical symptoms. There were no postoperative complications, including chemical meningitis. The postoperative control MRI performed 27 months after the operation showed the collapse of the cyst with significant reduction in its size and release of the CSF circulation pathways (Fig. 3). Note that the signal for cystic content on the control MRI was identical to that of the CSF, suggesting its continuous dilution (Fig. 3). DISCUSSION Craniopharyngioma is a benign brain tumour of embryonic origin which can be solid, cystic or mixed. For many decades and all over the world, neurosurgeons recommended the complete removal of this histologically benign tumour because it was supposed that its complete surgical removal should, in theory, allow its cure. Many surgical approaches have been used to remove these lesions, including the pterional, sub-temporal, interhemispheric, transcortical, transcallosal, transsphenoidal and translamina terminalis approaches (7,10,13,14). However, the often-intimate relationships of the tumour with delicate neurovascular structures and the frequent absence of a cleavage plan have modified this strategy towards less aggressive approaches. The search for new surgical management strategies as an alternative to the excision of craniopharyngiomas is primarily related to the high recurrence rate and the appearance of neurological sequelae incompatible with a good quality of life for some of the patients. The transsphenoidal endoscopic approach allows, in some cases, the removal of the tumour without manipulation of the brain, and has been associated with a reduction in the risk of postoperative complications (9). However, dissecting the tumour from the hypothalamus and the optic pathways, even through this minimally invasive surgical approach, may be the cause of a significant morbidity (8). The totally solid forms of craniopharyngioma represent only 10%, while the cystic or predominantly cystic forms can reach 60% (4,15). These cysts can become large, compressing the optic pathways and the hypothalamus and lead to obstructive hydrocephalus. In these cases, to avoid surgical morbidities, alternative surgical strategies aimed at shrinking the cyst may be used (8). Permanent and repeated cystic drainage can be effective even in the long term in most cases, since the clinical symptomatology of these cystic lesions is more related to the mass effect than to tumour infiltration. Conventionally, the management of these cystic craniopharyngiomas consists of placing a catheter in the cyst, connected to a subcutaneous reservoir, for the periodic aspiration of the cystic contents but also for the intracystic injection of chemo- and radiotherapeutic agents, to control tumour growth and delay the potentially harmful effects of surgery or radiotherapy (3). The use of neuroendoscopic positioning of intracystic catheters is considered to be safer than the stereotaxic approach, since the capsule of the cyst can be thick and visual control is preferable in this case. The concept of marsupialisation of the cyst in the ventricles, aimed at the continuous dilution of the cyst fluid and its resorption by the CSF pathways was introduced in 1997 by Spaziante and Divitiis (15). This cystoventriculostomy therefore represents an evolution of the first experiences of drainage of cystic craniopharyngiomas carried out by the pioneers (5,6,16). The transventricular neuroendoscopic approach is a minimally invasive option suitable for cystic craniopharyngiomas which are invasive or develop in the ventricular system. Under direct vision control, this approach, which allows total drainage of the cyst with wide marsupialisation in the ventricular system, represents obvious advantages over other drainage techniques (11). The operability of the instrument allows partial resection of the capsule for diagnostic purposes and especially for wide marsupialisation (11). During this procedure, special attention should be paid to complete elimination by aspiration and abundant rinsing of the cystic contents, since its leakage into the ventricles could possibly lead to chemical meningitis. Cysto-cisternostomy, making the cyst communicate with the basal cisterns, can be performed but remains a risky action in an area rich in delicate vascular and nervous structures and where the anatomical landmarks are not always identifiable. Some use stenting, which consists of placing a cysto-ventricular catheter to promote self-elimination of the cyst (8). Cysto-cisternostomy and stenting, which are measures to prevent reclosure and recurrence, were not performed in our case. In the context of a developing country such as ours, the high cost and unavailability of catheters and intracystic chemotherapy or radiotherapy make the endoscopic transventricular approach with a simple evacuation drainage and a wide marsupialisation of the cyst in the CSF circuit, a true minimally invasive alternative in the treatment of these cystic lesions. Even if the drainage and endoscopic transventricular marsupialization result in a significant and lasting regression of the cyst size, it remains nevertheless a temporary surgical option and requires regular clinical follow-up and close neuroradiological monitoring at 3 months, 6 months, and 12 months after surgery and then every 12 months (8). The use of intracavitary adjuvant treatments requires a sealed cavity, confirmed by a permeability test, which is incompatible with large marsupialisation of the cyst (11). In addition, the efficacy of these adjuvant treatment on prolonging recurrence-free survival in patients with cystic craniopharyngiomas is controversial and no randomised study has yet shown their superiority compared to a simple puncture-aspiration (1,2,3). In our case, the simple drainage of the cyst with a large marsupialisation in the ventricule, without cystocisternostomy, or stenting, allowed us to obtain a considerable reduction in the size of the cyst as well as its continuous dilution in the long term (27 months) with disappearance of any mass effect and consequently lasting resolution of clinical symptoms. CONCLUSION In cases of cystic or predominantly cystic craniopharyngioma, when symptoms are caused by the cystic component of the tumour, the minimally invasive transventricular neuroendoscopic approach targeting drainage and marsupialisation of the cyst may be sufficient and should be recommended. In our case, this minimally invasive approach has proven to be safe, simple and effective over the long term. However, it remains a temporary surgical option and requires regular clinical follow-up and close neuroradiological monitoring. Funding: No funding utilized from any organization. Conflicts of interest: None.
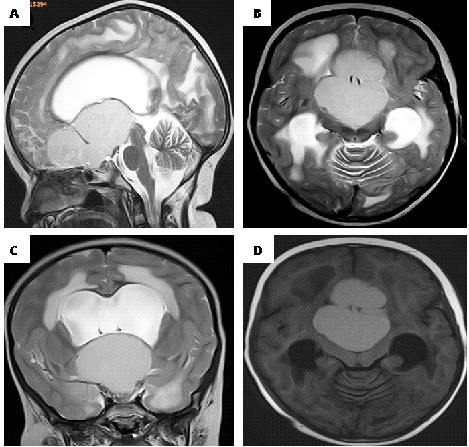 Figure 1. preoperative MRI images A-B-C: T1-weighted and D: T2-weighted showing a large cystic lesion of the sellar and suprasellar region extended under the forehead and behind, compressing and occupying the third ventricle. The cyst obstructs the two Monro foramens, causing a bi-ventricular hydrocephalus with a significant transependymal resorption.
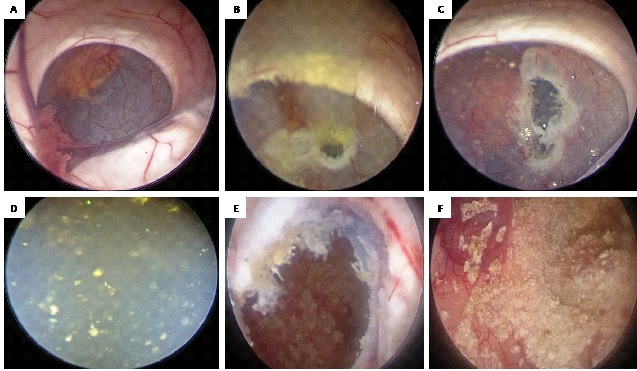 Figure 2. intraoperative neuroendoscopic images: A: view of the interior of the right lateral ventricle showing the cyst obstructing Monro foramen. B: View after fenestration of the cyst showing the oily liquid escaping under pressure. C and D: view after enlargement of the fenestration and rinsing showing the cystic liquid filled with shiny fragments. E and F: view of the interior of the cyst after complete drainage of its contents, showing yellow deposits on its internal wall.
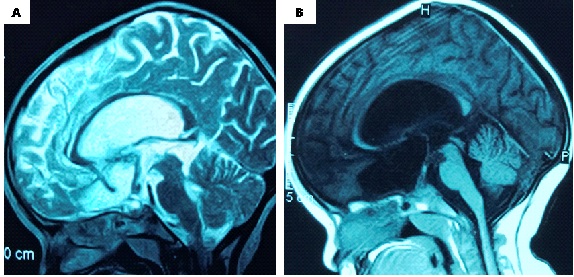 Figure 3. A: sagittal T2-weighted and B: T1-weighted post-operative MRI images (27 months) showing a considerable decrease in the size of the cyst with release of the LCS circulation pathways. Note: the sign from the cyst is identical to that of the LCS, suggesting continuous dilution. REFERENCES
|
© 2002-2018 African Journal of Neurological Sciences.
All rights reserved. Terms of use.
Tous droits réservés. Termes d'Utilisation.
ISSN: 1992-2647