NEUROEPIDEMIOLOGY / NEUROEPIDEMIOLOGIE
NEUROLOGIC ADMISSIONS IN THE NIGER DELTA AREA OF NIGERIA – A TEN YEAR REVIEW
LES MALADIES NEUROLOGIQUES OBSERVEES EN HOSPITALISATION, SUR UNE PERIODE DE 10 ANS DANS LA REGION DU DELTA AU NIGERIA
- Dept. of Internal Medecine, KING SAUD HOSPITAL P.O. BOX 1905, UNAIZAH 81888 UNAIZAH, AL QASSIM REGION KINGDOM OF SAUDI ARABIA
ABSTRACT
Background
The Niger-delta area of Nigeria constitutes about 20% of the population of the nation. The pattern of neurologic diseases in this area is not known.
Objective
The study was undertaken to determine the pattern of these diseases, compare this with those elsewhere and to have a baseline for future studies.
Methods
The medical records of all cases admitted with neurologic diseases in the University of Port Harcourt Teaching Hospital (UPTH) Port Harcourt between April 1993 and March 2003 were retrospectively reviewed and the frequency of neurologic diseases, sex, age and outcome of these diseases analyzed.
Results
Neurologic diseases constituted 1.5% and 33.1% of hospital and medical admissions respectively with M: F ratio of 1.4:1 and mean age of 52.6 years. The five topmost diseases were stroke (61.6%), meningitis and encephalitis (13.4%), tetanus (6.5%), spinal cord diseases (6.5%) and epilepsy (3.8%). Apart from stroke, the others were commoner in the young. Other neurologic diseases were rare causes of neurologic admissions. Neurologic deaths constituted 3.7% and 28.9% of hospital and medical deaths respectively. The common causes of neurologic deaths were stroke (65%), meningitis and encephalitis (18.7%) and tetanus (8.5%).
Conclusions
Neurologic diseases are common in this part and have a similar pattern as in other parts of southern Nigeria. Stroke and CNS infections are a major cause of morbidity and mortality. This finding makes the establishment of regional stroke units; improvement of the sanitary conditions of the home and environment, widespread use of immunizations for those at risk a matter of urgent healthcare priority.
Keywords : Africa, Epidemiology, Neurologic disease, Neurology, Nigeria, Stroke units
RESUME
Introduction
Le Delta du Niger constitue environ 20 % environ de la population du Nigeria, et le profil des affections neurologiques de cette région n’est pas connu.
Objectif
L’étude présentée a pour but de déterminer les aspects de ces maladies neurologiques en les comparant avec celles menées par d’autres équipes. Le travail servira de base pour mener d’autres études ultérieures.
Méthode
Les données médicales de tous les cas admis à l’université de Port Harcourt entre avril 1993 et mars 2003 ont été examinées rétrospectivement à partir des dossiers d’hospitalisation. La fréquence de maladie neurologique, le sexe, l’âge et l’évolution ont été analysés.
Résultats
Les maladies neurologiques représentent 1,5 % et 33,1 % des admissions respectivement en hospitalisation et sur l’ensemble de la pathologie médicale. Le ratio homme / femme est de 1,4 : 1 avec une moyenne d’âge de 52,6 ans. Les cinq maladies les plus fréquemment observées ont été : les accidents vasculaires cérébraux (61,6 %, les méningites et encéphalites (13,4 %) le tétanos (6,5 %), les maladies de la moelle épinière (6,5 %) et les épilepsies (3,8 %). En dehors des accidents vasculaires cérébraux, ces affections sont communes aux jeunes. Les autres affections neurologiques sont rares. Les décès imputables à la pathologie neurologique représentaient 3,7 % et 28,9 %, respectivement au niveau hospitalier et au plan médical.
La cause de décès la plus importante a été les accidents vasculaires cérébraux suivis des méningites et encéphalites (18,7 %) et tétanos (8,5 %)
Conclusion
Les affections neurologiques habituellement rencontrées ont un aspect similaire à celles observées dans le sud du Nigéria. Les AVC et les affections du système nerveux sont les principales causes de morbidité et de mortalité. Ces données impliquent la mise en place d’unités régionales d’AVC de même que l’amélioration des conditions sanitaires de l’environnement et de l’habitat et l’élargissement des vaccinations.
Mots-clefs : Afrique, maladies neurologiques, Nigéria, unité d’urgence neuro-vasculaire, épidémiologie.
INTRODUCTION
The Niger-delta extends over an area of about 70,000km2 and accounts for 7.5% of Nigeria’s land mass. It covers a coastline of 560km, about a third of the entire coastline of Nigeria, traversing nine states (Abia, Akwa Ibom, Bayelsa, Cross River, Delta, Edo, Imo, Ondo and Rivers) of the 36 states of the country with an estimated population of 20 million (1). The predominant occupation in the area are farming and fishing, with the oil sector as the main industrial base and responsible for over 90% of the nation’s export earnings. Port Harcourt, the Rivers State capital is the official capital of this area and harbors one of the four teaching hospitals in this area. Only two of these hospitals have the CT scan facility and there is no facility for the MRI. There are only two neurologists in this area. This study was conducted in the University of Port Harcourt Teaching Hospital (UPTH), a 484-bed tertiary referral center, with catchments area covering Rivers, Bayelsa, Abia, Akwa Ibom, Imo and parts of Cross River states and has an annual admission rate of 10,000 (2).
The hospital started active clinical services at its present temporary site in 1984. The Neurology Unit of the Department of Medicine was only recently created with the installation of a CT Scanning facility in the hospital in 2002. The pattern of neurologic admissions in this area is not known.
This study was therefore undertaken to determine the pattern of these diseases, compare it with those elsewhere in the country and also serve as a baseline for proper planning of the new unit and a yardstick for future studies.
MATERIALS AND METHODS
The records of all medical admissions between April 1993 and March 2003 were collected from the medical wards and the medical records department of the hospital. Admission into the medical wards is from age of 14 years, so patients below this were not included. Figures of hospital admissions and deaths during the same period were also collected from the medical records department. Cases admitted for purely neurologic disorders were extracted for the study. The following data were extracted from these patients’ records – age, sex, date of admission, diagnosis, date of discharge and outcome (whether discharged, died, discharged against medical advise or absconded, or referred to other tertiary centers or departments). These data were then analyzed. The neurologic diseases were grouped into the following diseases: stroke, TIAs (transient ischemic attacks), meningitis (bacterial, included tuberculous and viral) and encephalitis (viral, included rabies), spinal cord diseases (included Pott’s disease, cervical and lumbar spondylosis, and disc disease), tetanus, Parkinson’s disease and other movement disorders (included tremors, dystonias and dyskinesias), epilepsies, cerebellar syndromes, primary CNS tumors, neuropathies (cranial, autonomic and peripheral neuropathies included diabetic neuropathies), myopathies and neuromuscular disorders (included muscular dystrophies, polymyositis and myasthenia gravis), primary dementias and the primary headaches (migraine, cluster and tension headaches).
The diagnoses were made clinically in the majority of the patients, with laboratory confirmation in a few. The laboratory tests, depended on the suspected neurologic disease process and included complete blood count, ESR, serum biochemistry, ECG, x-rays, serological tests, microbiology, histopathology. CT scanning was used in a very small minority of patients since it became available only in 2002 and also because of affordability. The EEG, nerve conduction studies, EMG, carotid angiography, viral studies, histochemistry and other higher technology neurologic investigative tools were not utilized in the diagnoses of these patients because these facilities were not available. Lumbar puncture and muscle biopsies were used where these were indicated.
RESULTS
A total of 1,748 patients were admitted with neurologic disorders during the period under review out of which 1393 cases had sufficient data to be included into the study. The frequency of sex, age, morbidity and outcome of neurologic diseases were analyzed. Neurologic diseases constituted 1395 (33.1%) of 4213 medical admissions and 1.5% of 92,544 hospital admissions while in terms of mortality, they constituted 509(28.9%) of 1,759 medical deaths and 3.7% of 13,933 hospital deaths. The sex distribution of patients was 810 (58.1%) males and 585 (41.9%) females (Table 2), giving a sex ratio (M: F) of 1.4:1. The ages of the patients ranged from 14 – 110 years with a mean of 52.6 years. The mean age for males and females was 51.5 years and 54.1 years respectively. The shortest duration and longest duration of hospitalization was 1 day and 254 days respectively with a mean of 16.08 days. The mean duration of hospitalization for males and females was 15.05 and 17.49 days respectively. With regards to outcome, 787 (56.4%) of the patients were discharged, 509 (36.5%) died, 81 (5.8%) were discharged against medical advise (DAMA) or absconded and 16 (1.1%) were referred to other tertiary centers or our surgery department in the hospital. A summary of the above findings is shown in Table 1.
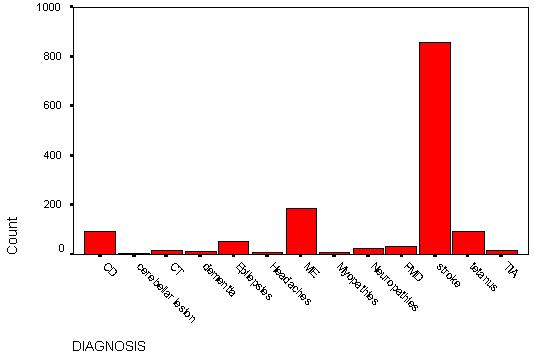
The frequency and the sex distribution of the various neurologic diseases as grouped above are shown in Tables 3, Fig. 1 and Table 4 respectively. Table 5 and Fig. 2 show the respective frequency of age ranges of the neurologic diseases individually and collectively. The frequency of admissions and deaths in relation to medical and hospital admissions and deaths are shown in tables 6. Tables 7 – 15 show the outcome neurologic diseases, as a whole and individually. The duration of hospitalization of these patients is on Tables 16 and 17.
DISCUSSION
This study revealed that neurologic diseases are common in the Niger-delta area of Nigeria. These diseases included stroke, TIAs, meningitis (mainly bacterial, including tuberculous meningitis and viral) and encephalitis (mainly viral including rabies), spinal cord disorders (mainly Pott’s disease, cervical and lumbar spondylosis, and disc disease), tetanus, Parkinson’s disease and other movement disorders (mainly tremors, dystonias and dyskinesias), epilepsies, cerebellar syndromes, primary CNS tumors, neuropathies (mainly cranial, autonomic and peripheral neuropathies, including diabetic neuropathies), myopathies and neuromuscular disorders(included muscular dystrophies, polymyositis and myasthenia gravis), primary dementias and primary headaches (migraine, cluster and tension headaches). These diseases constituted 1.5% of all hospital admissions and 33.1% of medical admissions. There was no significant sex predominance in these diseases as a whole. The mean age of the patients was 52.6 years with a slightly lower mean age in males. The highest peak age range of cases was between 60 to 64 years. The frequency of occurrence revealed that stroke (mainly cerebral infarction), infections (meningitis, encephalitis and tetanus), spinal cord diseases and epilepsies were the most common neurological disorders admitted with frequency rates of 61.6%, 19.9%, 6.5% and 3.8% of all neurologic admissions respectively. These four major disorders constituted 91.8% of all neurologic cases admitted. It was also noted that four of the cases of viral encephalitis had rabies, all of who died. Pott’s disease was the predominant cause of spinal cord diseases (31%). Other less common neurologic diseases were Parkinson’s disease and movement disorders 2.2%, neuropathies 1.8%, TIAs 1.2%, CNS tumors 1.1%, primary dementias 0.8%, primary headaches 0.4%, myopathies and neuromuscular disorders 0.5% and cerebellar diseases 0.3%. All these represented only 8.2% of the neurologic admissions. Parkinson’s disease constituted 83.3% of cases in the group of patients with movement disorders.
The above findings compare with those of Talabi (3) in UCH, Ibadan who reported frequencies of: stroke (50.4%), tetanus (14.2%), meningitis (12.4%) and myelopathies (8.1%). These disorders and seizures were reported as the most common neurologic diseases in that study. The difference in frequency rates in the two studies may be related to the difference in the duration of the study periods. The overall outcome of neurologic diseases showed that 787 (56%) were discharged, 509 (36.5%) died, 81(5.8%) were discharged against medical advice or absconded and 16 (1.1%) were referred to other hospital departments or tertiary centers. The death rate represented 28.9% and 3.7% of medical and hospital deaths respectively. The duration of hospitalization of patients with neurologic diseases was usually long, ranging from less than one day observed mainly in patients who died soon after admission, to 254 days, with a mean of 16.08 days. Females had a longer period of hospitalization (mean 21.37 days) than males (mean 16.04 days).
The age and sex distribution, outcome and period of hospitalization for the different types of neurologic diseases also varied. For the most common neurologic diseases, the following were observed:
Stroke – The peak age of admission was 60 to 64 years. This was in keeping with previous findings that stroke is a disease of the elderly in this environment (4) as is elsewhere (5), in contrast to earlier reports that stroke was more common below the age of 50 in the African (6,7). This trend may be related to the improving standard of living and longevity in our environment. However, when compared with Caucasians, a higher proportion of relatively younger Africans and Asians appear to suffer from stroke (8). There was a slight male preponderance (M: F=1.2:1) as had been noted previously (9). In terms of outcome, 468 (54.5%) of stroke admissions were discharged, 331 (38.5%) died, 52 (6.1%) were discharged against medical advice and 6 (0.7%) were referred. This stroke mortality represented 65% of neurologic deaths, 18.8% medical deaths and 2.37% hospital deaths. This shows that stroke mortality is quite high in this environment. Previous workers have also observed this finding. Odia and Wokoma (10) reported that cerebrovascular disease was the most common cause of deaths in the medical wards of UPTH, accounting for 15.9% of medical deaths. In Lagos Nigeria, Adegabite et al (11) noted stroke mortality of 36.5% and in Ibadan Nigeria; Adetuyibi et al (12) also observed that stroke was the commonest cause of neurologic deaths. The mean duration of hospitalization of stroke patients was 16.5 days.
Meningitis and encephalitis – This condition was also noted to be a significant cause of neurologic admissions and affected mainly the younger age group, with the highest age peak occurring in the age-range 15 to 19 years with a sex ratio (M: F) of 1.6:1. In the cases with this condition, 79 (42.2%) were discharged, 95 (50.8%) died, and 13 (7%) were discharged against medical advice. This group of patients recorded the highest mortality of 50.8%, although this represented 18.7% of neurologic deaths, 5.4% of medical deaths and 0.68% of hospital deaths. This mortality rate was very high when compared with that reported by Peters et al (13) in Calabar who recorded 19 (28.8%) deaths out of 66 cases studied. Their study however, did not include cases with encephalitis and was over a 5-year period. The mean duration of hospitalization of these patients was also the shortest (10 days), second only to patients admitted with TIAs. This was probably related to the high mortality rate.
Tetanus – This was another infective condition of the CNS affecting mainly the younger population. The peak age range affected was 20 to 24 years with a male predominance (M: F=2:1). In this group of patients, 45 (50%) were discharged, 43 (47.8%) died, 1 (1.1%) was discharged against medical advise and 1 (1.1%) was referred. The mortality represented 8.5% of neurologic deaths, 2.4% medical deaths and 0.31% hospital deaths. The high mortality rate noted in this group of patients is well known(14) and this is related to the low immunization rates of the population, late presentation, and inadequate intensive care facilities. The mean duration of hospitalization among these patients was 13.4 days.
Spinal cord diseases – The most common disease in this group was Pott’s disease and this was also more prevalent among the younger patients, with peak age-range 25 to 29 years and a sex ratio (M: F) of 1.8:1. Sixty-one (67%) of the cases were discharged, 15 (16.5%) died, 8 (8.8%) were discharged against medical advise and 7 (7.7%) were referred. The major cause of death was complicating secondary infections. The mortality represented 2.9% neurologic deaths, 0.9% medical deaths and 0.11% hospital deaths. This group of patients had the longest duration of hospitalization ranging from 1 day to 254 days, as they were usually bedridden, with a mean of 30.5 days.
Epilepsies – Majority of the patients in this group were also young with peak age-range 30 to 34 years and most had idiopathic epilepsy and were admitted with status epilepticus. There was no significant sex predilection. Forty (75.5%) of cases were discharged, 10 (18.5%) died and 3 (5.7%) were discharged against medical advise. Mortality was mainly due to status epilepticus and represented 1.9% neurologic deaths, 0.5% medical deaths and 0.07% hospital deaths. The mean duration of hospitalization was 13.2 days.
CONCLUSION
The Niger-delta area of Nigeria is unique in geography but not in the pattern of neurologic diseases. Stroke mainly cerebral infarction, is the commonest neurologic admission and the commonest cause of neurologic and medical death in this area as is noted elsewhere. Nearly two-fifths of stroke patients die. Infections of the central nervous system mainly meningitis, encephalitis and tetanus is the next common cause of admission and affect mainly the younger population. This group of diseases was also noted to have the highest mortality rate (mean 49.3%). Parkinson’s disease and movement disorders, neuropathies, TIAs, CNS tumors, primary dementias and headaches, myopathies and neuromuscular disorders, and cerebellar disorders were rare causes of neurologic admissions in this area.
In view of the above findings, the provision of a regional stroke unit with modern primary, secondary (including standard Intensive Care Units) and tertiary intervention facilities; the improvement of the sanitary conditions of the home and environment; the widespread use of immunizations against meningitis, tetanus and rabies for those at risk, cannot be over-emphasized. These interventions will to cut down drastically the scourge caused by stroke and CNS infections.
| ACNOWLEGEMENTS |
| My gratitude goes to the Almighty God for His mercies and Guidance; to the Matron, Dept of Medicine and the staff of the Medical Records Dept of UPTH, Port Harcourt for their assistance in the collection of the data and finally to my family for ensuring a conducive study environment at home. |
TABLE 1 – Summary of major findings
| TOTAL NO. NEUROLOGIC ADMISSIONS |
1748 |
| TOTAL NO. OF PATIENTS INCLUDED IN THE STUDY (I.E.TOTAL NEUROLOGICAL ADMISSIONS) |
1395 |
| TOTAL NO. OF PATIENTS EXCLUDED FROM THE STUDY |
353 |
| TOTAL NEUROLOGIC DEATHS |
509 |
| TOTAL HOSPITAL ADMISSIONS |
92,544 |
| TOTAL HOSPITAL DEATHS |
13,933 |
| TOTAL MEDICAL ADMISSIONS |
4,213 |
| TOTAL MEDICAL DEATHS |
1759 |
| % MEDICAL ADMISSIONS OF HOSPITAL ADMISSIONS |
4.6% |
| % NEUROLOGIC ADMISSIONS OF HOSPITAL ADMISSIONS |
1.5% |
| % NEUROLOGIC DEATHS OF HOSPITAL DEATHS |
3.7% |
| % NEUROLOGIC ADMISSIONS OF MEDICAL ADMISSIONS |
33.1% |
| % NEUROLOGIC DEATHS OF MEDICAL DEATHS |
28.9% |
| MEAN AGE OF NEUROLOGIC PATIENTS |
52.6YRS |
| MEAN AGE (MALES) |
51.5YRS |
| MEAN AGE (FEMALES) |
54.1YRS |
| MEAN DURATION OF HOSPITALIZATION OF ALL PATIENTS |
16.07 DAYS |
| MEAN DURATION OF HOSPITALIZATION (MALES) |
15.05 DAYS |
TABLE 2 – Sex frequency
| |
Frequency |
Percent |
Valid Percent |
Cumulative Percent |
| Female |
585 |
41.9 |
41.9 |
41.9 |
| Male |
810 |
58.1 |
58.1 |
100.0 |
| Total |
1395 |
100.0 |
100.0 |
|
TABLE 3 – Frequency distribution of neurologic diseases (also see Fig 1).
| NEUROLOGICDISEASES |
Frequency |
Percent |
Valid Percent |
Cumulative Percent |
| Cord diseases (CD) |
91 |
6.5 |
6.5 |
6.5 |
| Cerebellar lesions (CL) |
4 |
.3 |
.3 |
6.8 |
| Dementia (D) |
11 |
.8 |
.8 |
7.6 |
| Meningitis & encephalitis (ME) |
187 |
13.4 |
13.4 |
21.0 |
| Primary headaches (H) |
6 |
.4 |
.4 |
21.4 |
| Myopathies (MP) |
7 |
.5 |
.5 |
21.9 |
| Parkinson’s disease/Movement disorders (PMD) |
30 |
2.2 |
2.2 |
24.1 |
| Neuropathies (N) |
25 |
1.8 |
1.8 |
25.9 |
| Epilepsies (E) |
53 |
3.8 |
3.8 |
29.7 |
| CNS Tumors (CT) |
15 |
1.1 |
1.1 |
30.8 |
| Stroke (STR) |
859 |
61.6 |
61.6 |
92.3 |
| Tetanus (TET) |
90 |
6.5 |
6.5 |
98.8 |
| Transient ischemic attacks (TIA) |
17 |
1.2 |
1.2 |
100.0 |
| TOTAL |
1395 |
100.0 |
100.0 |
|
TABLE 4 – Sex frequency of Neurologic diseases.
| DIAGNOSIS |
SEX (F) |
SEX (M) |
Total |
| Cord diseases |
33 |
58 |
91 |
| Meningitis & encephalitis |
71 |
116 |
187 |
| Myopathies |
2 |
5 |
7 |
| Parkinson’s disease/Movement disorders |
7 |
23 |
30 |
| Neuropathies |
7 |
18 |
25 |
| CNS Tumors |
5 |
10 |
15 |
| Transient ischemic attacks |
7 |
10 |
17 |
| Cerebellar lesions |
|
4 |
4 |
| Dementia |
6 |
5 |
11 |
| Primary headaches |
5 |
1 |
6 |
| Epilepsies |
26 |
27 |
53 |
| Stroke |
386 |
473 |
859 |
| Tetanus |
30 |
60 |
90 |
| TOTAL |
585 |
810 |
1395 |
TABLE 5 – Age-range distribution of neurologic diseases
| AGE GRP |
CASE NO. |
CD |
ME |
MP |
PMD |
N |
CT |
TIA |
CL |
DEM |
H |
E |
STR |
TET |
TOTAL |
| <15y |
1 |
|
1 |
|
|
|
1 |
|
|
|
|
|
|
|
2 |
| 15-19 |
2 |
8 |
37 |
|
1 |
|
3 |
|
|
|
|
2 |
|
15 |
66 |
| 20-24 |
3 |
6 |
25 |
2 |
|
4 |
1 |
|
|
|
2 |
6 |
2 |
21 |
69 |
| 25-29 |
4 |
12 |
27 |
|
|
4 |
1 |
|
|
|
2 |
5 |
1 |
16 |
68 |
| 30-34 |
5 |
7 |
18 |
1 |
|
4 |
|
|
2 |
|
|
9 |
12 |
8 |
61 |
| 35-39 |
6 |
4 |
14 |
|
1 |
3 |
2 |
2 |
1 |
|
|
2 |
30 |
6 |
65 |
| 40-44 |
7 |
8 |
13 |
1 |
1 |
3 |
|
2 |
|
|
1 |
4 |
53 |
11 |
97 |
| 45-49 |
8 |
8 |
10 |
|
1 |
3 |
1 |
1 |
|
|
|
1 |
71 |
4 |
100 |
| 50-54 |
9 |
5 |
10 |
2 |
2 |
2 |
|
2 |
1 |
|
|
4 |
113 |
1 |
142 |
| 55-59 |
10 |
7 |
7 |
|
2 |
1 |
2 |
2 |
|
|
|
6 |
98 |
3 |
128 |
| 60-64 |
11 |
8 |
8 |
1 |
10 |
|
2 |
3 |
|
2 |
|
5 |
123 |
3 |
165 |
| 65-69 |
12 |
7 |
8 |
|
3 |
1 |
|
3 |
|
4 |
|
1 |
110 |
1 |
138 |
| 70-74 |
13 |
7 |
4 |
|
2 |
|
1 |
|
|
|
1 |
7 |
109 |
|
131 |
| 75-79 |
14 |
1 |
2 |
|
3 |
|
|
2 |
|
4 |
|
|
70 |
|
82 |
| >79 |
15 |
3 |
3 |
|
4 |
|
1 |
|
|
1 |
|
1 |
67 |
1 |
81 |
| TOTAL |
|
91 |
187 |
7 |
30 |
25 |
15 |
17 |
4 |
11 |
6 |
53 |
859 |
90 |
1395 |
CD=cord diseases
ME=meningitis & encephalitis
MP=myopathies, PMD=Parkinsonu2019s disease/movement disorders
N=neuropathies
CT=CNS tumors
TIA=transient ischemic attack
CL=cerebellar lesions
DEM=dementia
H=primary headaches
E=epilepsies
STR=stroke
TET=tetanus
TABLE 6 – Frequency of admissions and deaths of neurologic diseases in relation to medical and hospital admissions and deaths.
| DISEASE |
ADMS |
%NA |
DTHS |
%ND |
%MA |
%MD |
%HA |
%HD |
| STROKE |
859 |
61.6 |
331(38.5%) |
65.0 |
20.4 |
18.8 |
0.93 |
2.37 |
| MENINGITIS & ENCEPHALITIS |
187 |
13.4 |
95(50.8%) |
18.7 |
4.4 |
5.4 |
0.20 |
0.68 |
| CORD DISEASE |
91 |
6.5 |
15(16.5%) |
2.9 |
2.2 |
0.9 |
0.10 |
0.11 |
| TETANUS |
90 |
6.4 |
43(47.8%) |
8.5 |
2.1 |
2.4 |
0.10 |
0.31 |
| EPILEPSIES |
53 |
3.8 |
10(18.9%) |
1.9 |
1.3 |
0.5 |
0.06 |
0.07 |
| PD/MD |
30 |
2.2 |
5(16.7%) |
1.0 |
0.7 |
0.3 |
0.03 |
0.04 |
| NEUROPATHIES |
25 |
1.8 |
2(8.0%) |
0.4 |
0.6 |
0.1 |
0.03 |
0.01 |
| TIA |
17 |
1.2 |
0 |
0 |
0.4 |
0 |
0.02 |
0 |
| CNS TUMORS |
15 |
1.1 |
7(46.7%) |
1.4 |
0.4 |
0.4 |
0.02 |
0.05 |
| DEMENTIA |
11 |
0.8 |
1(9.1%) |
0.2 |
0.3 |
0.1 |
0.01 |
0.01 |
| HEADACHES |
6 |
0.4 |
0 |
0 |
0.1 |
0 |
0.01 |
0 |
| MYOPATHIES |
7 |
0.5 |
0 |
0 |
0.1 |
0 |
0.01 |
0 |
| CEREBELLAR LESIONS |
4 |
0.3 |
0 |
0 |
0.1 |
0 |
0.004 |
0 |
| TOTAL |
1395 |
100% |
509(36.5%) |
100% |
33.1% |
28.9% |
1.51% |
3.65% |
ADMS=admissions
DTHS=deaths
NA=neurologic admissions
ND=neurological deaths
MA= medical admissions
MD=medical deaths
HA=hospital admissions
HD=hospital deaths
TABLE 7 – Outcome of all neurologic diseases
| |
|
Frequency |
Percent |
Valid Percent |
Cumulative Percent |
| Valid |
|
608 |
43.6 |
43.6 |
43.6 |
| |
Discharged |
787 |
56.4 |
56.4 |
100.0 |
| |
Total |
1395 |
100.0 |
100.0 |
|
| |
|
Frequency |
Percent |
Valid Percent |
Cumulative Percent |
| Valid |
|
886 |
63.5 |
63.5 |
63.5 |
| |
Died |
509 |
36.5 |
36.5 |
100.0 |
| |
Total |
1395 |
100.0 |
100.0 |
|
| |
|
Frequency |
Percent |
Valid Percent |
Cumulative Percent |
| Valid |
|
1298 |
93.0 |
93.0 |
93.0 |
| |
DAMA |
81 |
5.8 |
5.8 |
98.9 |
| |
Referred |
16 |
1.1 |
1.1 |
100.0 |
| |
Total |
1395 |
100.0 |
100.0 |
|
TABLE 8 – Stroke outcome
| |
|
Frequency |
Percent |
Valid Percent |
Cumulative Percent |
| Valid |
|
528 |
61.5 |
61.5 |
61.5 |
| |
Died |
331 |
38.5 |
38.5 |
100.0 |
| |
Total |
859 |
100.0 |
100.0 |
|
| |
|
Frequency |
Percent |
Valid Percent |
Cumulative Percent |
| Valid |
|
391 |
45.5 |
45.5 |
45.5 |
| |
Discharged |
468 |
54.5 |
54.5 |
100.0 |
| |
Total |
859 |
100.0 |
100.0 |
|
| |
|
Frequency |
Percent |
Valid Percent |
Cumulative Percent |
| Valid |
|
801 |
93.2 |
93.2 |
93.2 |
| |
DAMA |
52 |
6.1 |
6.1 |
99.3 |
| |
Referred |
6 |
.7 |
.7 |
100.0 |
| |
Total |
859 |
100.0 |
100.0 |
|
TABLE 9 – Cord diseases outcome
| |
|
Frequency |
Percent |
Valid Percent |
Cumulative Percent |
| Valid |
|
30 |
33.0 |
33.0 |
33.0 |
| |
Discharged |
61 |
67.0 |
67.0 |
100.0 |
| |
Total |
91 |
100.0 |
100.0 |
|
| |
|
Frequency |
Percent |
Valid Percent |
Cumulative Percent |
| Valid |
|
76 |
83.5 |
83.5 |
83.5 |
| |
Died |
15 |
16.5 |
16.5 |
100.0 |
| |
Total |
91 |
100.0 |
100.0 |
|
| |
|
Frequency |
Percent |
Valid Percent |
Cumulative Percent |
| Valid |
|
76 |
83.5 |
83.5 |
83.5 |
| |
DAMA |
8 |
8.8 |
8.8 |
92.3 |
| |
Referred |
7 |
7.7 |
7.7 |
100.0 |
| |
Total |
91 |
100.0 |
100.0 |
|
TABLE 10 – Epilepsies outcome
| |
|
Frequency |
Percent |
Valid Percent |
Cumulative Percent |
| Valid |
|
43 |
81.1 |
81.1 |
81.1 |
| |
Died |
10 |
18.9 |
18.9 |
100.0 |
| |
Total |
53 |
100.0 |
100.0 |
|
| |
|
Frequency |
Percent |
Valid Percent |
Cumulative Percent |
| Valid |
|
13 |
24.5 |
24.5 |
24.5 |
| |
Discharged |
40 |
75.5 |
75.5 |
100.0 |
| |
Total |
53 |
100.0 |
100.0 |
|
| |
|
Frequency |
Percent |
Valid Percent |
Cumulative Percent |
| Valid |
|
50 |
94.3 |
94.3 |
94.3 |
| |
DAMA |
3 |
5.7 |
5.7 |
100.0 |
| |
Total |
53 |
100.0 |
100.0 |
|
TABLE 11 – Tetanus outcome
| |
|
Frequency |
Percent |
Valid Percent |
Cumulative Percent |
| Valid |
|
47 |
52.2 |
52.2 |
52.2 |
| |
Died |
43 |
47.8 |
47.8 |
100.0 |
| |
Total |
90 |
100.0 |
100.0 |
|
| |
|
Frequency |
Percent |
Valid Percent |
Cumulative Percent |
| Valid |
|
45 |
50.0 |
50.0 |
50.0 |
| |
Discharged |
45 |
50.0 |
50.0 |
100.0 |
| |
Total |
90 |
100.0 |
100.0 |
|
| |
|
Frequency |
Percent |
Valid Percent |
Cumulative Percent |
| Valid |
|
88 |
97.8 |
97.8 |
97.8 |
| |
DAMA |
1 |
1.1 |
1.1 |
98.9 |
| |
Referred |
1 |
1.1 |
1.1 |
100.0 |
| |
Total |
90 |
100.0 |
100.0 |
|
TABLE 12 – Meningitis & Encephalitis outcome
| |
|
Frequency |
Percent |
Valid Percent |
Cumulative Percent |
| Valid |
|
92 |
49.2 |
49.2 |
49.2 |
| |
Died |
95 |
50.8 |
50.8 |
100.0 |
| |
Total |
187 |
100.0 |
100.0 |
|
| |
|
Frequency |
Percent |
Valid Percent |
Cumulative Percent |
| Valid |
|
108 |
57.8 |
57.8 |
57.8 |
| |
Discharged |
79 |
42.2 |
42.2 |
100.0 |
| |
Total |
187 |
100.0 |
100.0 |
|
| |
|
Frequency |
Percent |
Valid Percent |
Cumulative Percent |
| Valid |
|
174 |
93.0 |
93.0 |
93.0 |
| |
DAMA |
13 |
7.0 |
7.0 |
100.0 |
| |
Total |
187 |
100.0 |
100.0 |
|
TABLE 13 – Neuropathies outcome
| |
|
Frequency |
Percent |
Valid Percent |
Cumulative Percent |
| Valid |
|
3 |
12.0 |
12.0 |
12.0 |
| |
Discharged |
22 |
88.0 |
88.0 |
100.0 |
| |
Total |
25 |
100.0 |
100.0 |
|
| |
|
Frequency |
Percent |
Valid Percent |
Cumulative Percent |
| Valid |
|
24 |
96.0 |
96.0 |
96.0 |
| |
DAMA |
1 |
4.0 |
4.0 |
100.0 |
| |
Total |
25 |
100.0 |
100.0 |
|
| |
|
Frequency |
Percent |
Valid Percent |
Cumulative Percent |
| Valid |
|
23 |
92.0 |
92.0 |
92.0 |
| |
Died |
2 |
8.0 |
8.0 |
100.0 |
| |
Total |
25 |
100.0 |
100.0 |
|
TABLE 14 – Parkinson’s disease/movement disorders outcome
| |
|
Frequency |
Percent |
Valid Percent |
Cumulative Percent |
| Valid |
|
25 |
83.3 |
83.3 |
83.3 |
| |
Died |
5 |
16.7 |
16.7 |
100.0 |
| |
Total |
30 |
100.0 |
100.0 |
|
| |
|
Frequency |
Percent |
Valid Percent |
Cumulative Percent |
| Valid |
|
6 |
20.0 |
20.0 |
20.0 |
| |
Discharged |
24 |
80.0 |
80.0 |
100.0 |
| |
Total |
30 |
100.0 |
100.0 |
|
| |
|
Frequency |
Percent |
Valid Percent |
Cumulative Percent |
| |
|
29 |
96.7 |
96.7 |
96.7 |
| |
DAMA |
1 |
3.3 |
3.3 |
100.0 |
| |
Total |
30 |
100.0 |
100.0 |
|
TABLE 15 – CNS tumors outcome
| |
|
Frequency |
Percent |
Valid Percent |
Cumulative Percent |
| Valid |
|
9 |
60.0 |
60.0 |
60.0 |
| |
Died |
6 |
40.0 |
40.0 |
100.0 |
| |
Total |
15 |
100.0 |
100.0 |
|
| |
|
Frequency |
Percent |
Valid Percent |
Cumulative Percent |
| Valid |
|
8 |
53.3 |
53.3 |
53.3 |
| |
Discharged |
7 |
46.7 |
46.7 |
100.0 |
| |
Total |
15 |
100.0 |
100.0 |
|
| |
|
Frequency |
Percent |
Valid Percent |
Cumulative Percent |
| Valid |
|
13 |
86.7 |
86.7 |
86.7 |
| |
DAMA |
1 |
6.7 |
6.7 |
93.3 |
| |
Referred |
1 |
6.7 |
6.7 |
100.0 |
| |
Total |
15 |
100.0 |
100.0 |
|
TABLE 16 – Duration of hospitalization of all neurologic patients.
| |
N |
Minimum |
Maximum |
Mean |
Std. Deviation |
| WARD STAY |
1395 |
1 |
254 |
16.08 |
18.49 |
| Valid N (listwise) |
1395 |
|
|
|
|
| |
|
|
|
|
|
| SEX |
Mean |
N |
Std. Deviation |
| F |
17.49 |
585 |
21.37 |
| M |
15.05 |
810 |
16.04 |
| Total |
16.08 |
1395 |
18.49 |
TABLE 17 -Duration of hospitalization of individual neurologic diseases
| NEUROLOGICDISEASES |
Shortest duration of ward stay (days) |
Longest duration of ward stay (days) |
Mean duration of ward stay(days) |
| Stroke |
1 |
160 |
16.5 |
| TIA |
3 |
32 |
1 |
| Parkinson’s disease/Movement disorders |
1 |
58 |
16.7 |
| Meningitis & encephalitis |
1 |
66 |
10 |
| Cerebellar lesions |
3 |
22 |
14.8 |
| Epilepsies |
1 |
61 |
13.2 |
| Tetanus |
1 |
159 |
13.4 |
| Cord diseases |
1 |
254 |
30.5 |
| Myopathies |
2 |
42 |
11.3 |
| Neuropathies |
1 |
42 |
18.3 |
| CNS Tumors |
1 |
44 |
12.9 |
| Dementia |
4 |
38 |
14 |
| Headaches |
7 |
22 |
13 |
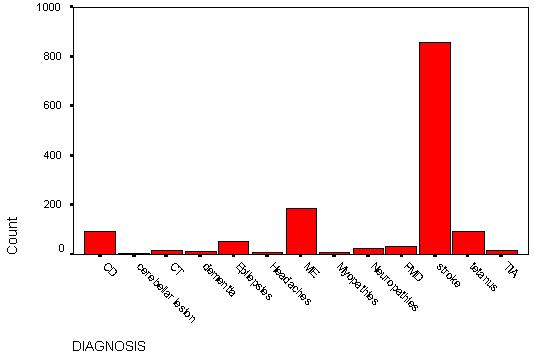
FIGURE 1 – Frequency distribution of neurologic diseases (also see Table 3)

REFERENCES
- http://www.nddconline.org/The NigerDelta/index.shtml
- University of Port Harcourt Teaching Hospital (UPTH) Annual Reports, 1990.
- TALABI OA. A 3-year review of neurologic admissions in University College Hospital Ibadan, Nigeria. WAJM 2003; 2 :
- CHAPP-JUMBO EN. A clinical study on the pattern of stroke in the University of Port Harcourt Teaching Hospital, Port Harcourt, Rivers State, Nigeria. A dissertation submitted to the West African College of Physicians in part fulfillment of the Fellowship of the college in Internal Medicine. 1998.
- BONITA R. Epidemiology of stroke. Lancet 1992; 339: 342-344.
- JAMES PD. Cerebrovascular disease in Uganda. Trop Geo Med 1975; 27: 125 – 131.
- ABRAHAM G, ABDULKADIR J. Cerebrovascular diseases in Ethiopians. A review of 48 cases. E Afr Med J 1981; 58(6): 431-436.
- AHMED A. Common neurological problems in Middle East – Part 4 – stroke. Postgrad Doc – Africa 1988; 10(3): 73-76.
- OSUNTOKUN B.O. Stroke in the Africans. Afr J Med Sci 1977; 6: 39-53.
- ODIA OJ, WOKOMA FS. Mortality patterns in the medical wards of a Nigerian Teaching Hospital. Orient J Med 1992; 4: 96-101.
- ADEGABITE SA, ARABA AB, DADA TO, JOHNSON FA. Cerebrovascular accidents in Nigerians. A review of 205 cases. W Afr J Med 1969; 18:95 -108.
- ADETUYIBI A, AKINSANYA JB, ONADEKO NO. Analysis of causes of death in the medical wards of the University College Hospital, Ibadan over a 14 year period (1960-73). Trans R. Soc Med Hyg 1976; 70: 466-473.
- PETERS EJ, IMMANANAGHA KK, PHILIP EPHRAIM EE, IBANGA IA. Bacterial meningitis in adults at the University of Calabar Teaching Hospital. A5-year retrospective study 1993-97. Globe J Med Sc 2003; 2 :1
- ADEUJA AOG, OSUNTOKUN BO. Tetanus in adult Nigerians (503 patients). East Afr Med J 1971; 48:683-691,