CLINICAL STUDIES / ETUDES CLINIQUES
NEUROLOGICAL MANIFESTATIONS HIV-INFECTED PATIENTS AROUND VARANASI, INDIA
MANIFESTATIONS NEUROLOGIQUES CHEZ LES PATIENTS INFECTÉS PAR LE VIH DANS LA RÉGION DE VARANASI (INDE)
- Department of Medicine, Institute of Medical Sciences, BHU, Varanasi-221005
- Department of Microbiology, Institute of Medical Sciences, BHU, Varanasi-221005
- Department of Dermatology and STD clinic, Institute of Medical Sciences, BHU, Varanasi-221005
ABSTRACT
Background
Most of the studies on the neurological manifestations in HIV patients in India were cross sectional in design, and focus on the etiological agents. We report data on the frequency of neurological manifestations, associations with CD4 counts, and outcome of its various presentations in a 3-year prospective hospital-based study.
Methods
All HIV-infected patients attending the Infectious Disease clinic for various neurological manifestations between Jan 2001 and December 2003 were included in the study. Their clinical details, treatment received, and response to treatment were accessed and analyzed.
Results
During this period, 57 had some neurological manifestations and made 145 clinic visits, with 158 distinct episodes of neurological related symptoms, giving a crude rate of 307 neurological episodes per 1000 person year of observation
Conclusion
Opportunistic infections were the leading cause of neurological disorders in our study population. Apart from Central nervous system (CNS) tuberculosis, other CNS diseases were good predictor of the advanced HIV infection (CD4<200). CNS tuberculosis cannot be considered as an opportunistic infection in most of the instances as it can be seen in relatively earlier stages of the disease. Cerebrospinal fluid picture was normal in all our patients of CNS toxoplasmosis. All the patients with progressive multifocal leuco encephalopathy had seizures as the initial manifestation. AIDS-dementia complex and CNS malignancies were not observed in our patients. There were equal responses to Amphoterecin B Cholesterol Dispersion (ABCD) and conventional Amphoterecin B therapies, and no significant differences in their side effect profiles.
Key words: infections, HIV, India
Key words: infections, VIH, Inde
INTRODUCTION
India is estimated to have more than 60,000 full-blown AIDS cases by the end of 2005, and this makes it one of its fast growing health problems (13) NACO 2005). The clinical spectrum of HIV infection in India is different from rest of the world, and regional variability has been reported within India (1,2,6,10,11,14,15,16) Central nervous system (CNS) infections are the third commonest cause of morbidity and second commonest cause of mortality in HIV patients (13). There has been no prospective study so far to determine the frequency and pattern of CNS infections in HIV patients in eastern Uttar Pradesh and western Bihar regions. This study was therefore undertaken to provide such baseline information.
METHODS
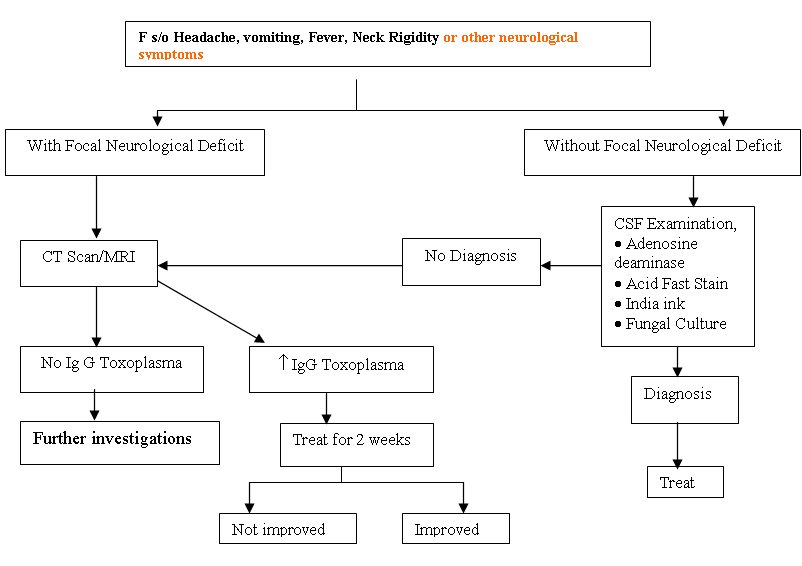
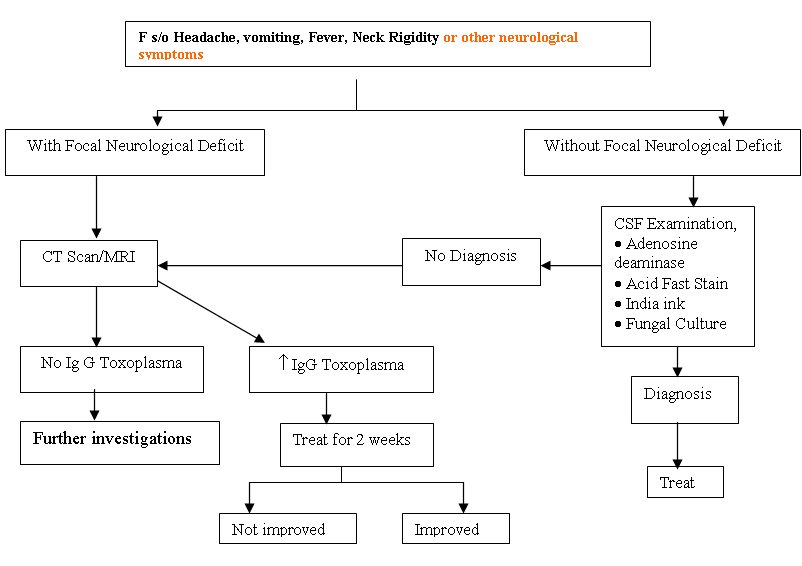
All HIV infected patients attending the Infectious Disease clinic for various neurological manifestations were included in the study. Sir Sunderlal hospital, affiliated to Institute of Medical Sciences, Banaras Hindu University is a tertiary care teaching hospital with catchments area of five states (Uttar Pradesh, Madhya Pradesh, Bihar, Jharkhand, and Chattisgarh) with 1000 beds. The annual attendance of new HIV cases is approximately 150. HIV related CNS diseases, clinical characters and the treatment outcomes were registered. An informed consent was taken from all the subjects of study prior to investigative procedures. The general work up protocol followed in this study was outlined as below.
Diagniostic criteria followed
Diagnosis of tubercular meningitis was based on history of sub acute or chronic meningitis, cerebrospinal fluid (CSF) showing increased protein levels, lymphocytic pleocytosis along with raised Adenosine deaminase levels above 7 IU/L, and presence of acid fast tubercular bacilli (AFB). Cryptococcal meningitis was diagnosed by India ink method, or culture demonstrating Cryptococcus or both. Toxoplasmosis was diagnosed by CT/MRI showing multiple ring enhancing lesions, raised Ig G levels and response to treatment. Progressive multifocal leukoencephalopathy was diagnosed by MRI. However we did not perform neuropathological studies of biopsied brain tissue owing to cultural and ethical constraints. Individuals who had no specific identifiable diagnosis were classified as Undiagnosed
CD4 / Viral load estimation
Immuno phenotype of lymphocytes was carried out by FACS count (Becton Dickinson, Singapore (BD). Viral load was not done due to economic constraints.
RESULTS
The study population of 375 patients consisted of individual who had come forward, with the HIV related symptoms. There were no differences in age sex, or clinical stage between patients with and without neurological deficits therefore further comparison was not made. All the patients in the present study were on HAART as all of them have AIDS. During this period, 57 had some neurological manifestations and made 145 clinic visits, with 158 distinct episodes (defined as any visit for the symptoms, for which the etiology or the outcome could be attributable to nervous system), giving a crude rate of 307 neurological episodes per 1000 Person years of observation. The clinical profile of the patients is shown in Table 1.
Table 1: Neurological manifestations
| Symptoms/sign (number of patients) |
CCM (n=16) |
TBM (n=25) |
Toxoplasma (n=5) |
PML (n=3) |
Undiagnosed (n=8) |
| Fever (42) |
12 (75%) |
23 (92%) |
1 (20%) |
0(0%) |
6 (75%) |
| Headache (40) |
14 (87.5%) |
20 (80%) |
2 (40%) |
0(0%) |
4(50%) |
| Focal Neurological Deficit (13)[barring cerebellar signs] |
2 (12.5%) |
6 (24%) |
5 (100%) |
0(0%) |
0(0%) |
| Cerebellar signs (5) |
1 (6.25%) |
1 (4%) |
0 (0%) |
3 (100%) |
0(0%) |
| Increase Intracranial Tension with meningeal signs (40) |
14 (87.5%) |
21 (84%) |
1 (20%) |
0 (0%) |
4 (50%) |
| Seizure (26) |
8 (50%) |
7 (28%) |
2 (40%) |
3 (100%) |
6 (75%) |
| Altered sensorium (18) |
6 (37.5%) |
9 (36%) |
3 (60%) |
0(0%) |
0(0%) |
| Papilloedema (20) |
8 (50%) |
10 (40%) |
0 (0%) |
0(0%) |
2 (25%) |
CCM = Cryptococcal Meningitis
TBM = Tubercular Meningitis
PML = Progressive Multifocal Leucoencephalopathy
All the patients of PML had seizures and cerebellar symptoms only at presentation there by making PML as one of the important differential diagnosis in all patients with those symptoms in our population. In a similar way presence of fever indicates either CCM or TBM, as most of our patients have either of them. Headache is fairly common in all the patients barring those having PML. Presence of focal neurological deficits (probably secondary to the toxoplasm bodies) strongly argue in favor of toxoplasmosis, the second commonest diagnosis being TBM.
Cerebrospinal fluid examination results were expressed in the below table
Table 2: Cerebrospinal fluid (CSF) findings
| CSF finding |
CCM (n=16) |
TBM (n=25) |
Toxoplasma (n=5) |
PML (n=3) |
Undiagnosed (n=8) |
| Cells (/mm3) |
20±6 |
97.4±49.4 |
6.8±1.3 |
6.8±1.3 |
8±2 |
| Neutrophils (%) |
0 |
4±6 |
0 |
0 |
0 |
| Lymphocytes (%) |
100 |
95±6 |
100 |
100 |
100 |
| Protein (mg/dl) |
68.6±26.2 |
186±67 |
81±14 |
81±14 |
42±2 |
| Sugar (mg/dl) |
10.3±7.2 |
30±8 |
29±8.9 |
29±8.9 |
68±24 |
| India ink |
+ve in 15/16 |
– ve |
-ve |
-ve |
-ve |
| ADA (IU/L) |
3 |
8 |
2 |
3 |
0 |
| CD4 (Mean ± SD) |
135± 64 |
190 ± 170 |
115 ± 82 |
104 ± 61 |
– |
| CD4 Range |
12-245 |
30-610 |
12-241 |
35-153 |
– |
All the patients with tubercular meningitis had marked lymphocytic pleocytosis (mean cell count of 97.4±49.4) along with raised protein levels (mean 186+67). ADA levels were raised markedly in all the cases (8). In CCM although pleocytosis was seen, it was not so high as in cases of tuberculosis (20+6). There was a mild elevation in protein content, but CSF sugar levels were extremely low (10.3+7.2. CNS toxoplasmosis was suspected in 5 patients with focal neurological deficits. In all the patients, MRI/Double contrast CT showed multiple ring enhancing lesions and IgG levels for Toxoplasma was markedly raised. Four patients responded to therapy. All the patients of progressive multifocal leuco encephalopathy had cerebellar signs, and seizures. Diagnosis was made by MRI. In 8 patients the etiology could not be made out as the patients expired on the very same day of admission and were labled as undiagnosed.
The positive predictive value of the various neurological disorders in predicting the CD4 levels of less than 200 were represented in the table 3 and was compared with other AIDS defining illnesses.
Table 3: Specificity and positive predictive value of few neurological conditions
| Disease |
Specificity (%) |
Positive predictive value (%) |
| PML |
100 |
100 |
| Cryptococcal Meningitis |
98.1 |
81.25 |
| CNS Toxoplasmosis |
99.3 |
80 |
| Tubercular meningitis |
93.86 |
73.4 |
| Candidiasis |
69.3 |
38.27 |
| Recurrent Herpes Zoster |
97.5 |
66.6 |
| Molluscum Contagiosum |
99.3 |
83.3 |
| Tubercular Lymphadenitis |
87.1 |
8.6 |
| PCP |
97.5 |
71.4 |
Table 4: Treatment outcome in different neurological conditions
| Disease |
Treatment |
No. of patients |
Response: Improved |
Response: Not improved |
Response: Lost in follow up |
Response: Expired |
| CCM |
Ampho B |
6 |
4 |
0 |
0 |
2 |
| |
ABCD |
6 |
4 |
0 |
1 |
1 |
| |
fluconazole alone |
4 |
0 |
0 |
4 |
0 |
| TBM |
RHEZ+Q+S |
18 |
9 |
2 |
5 |
2 |
| |
RHEZ+S |
7 |
3 |
2 |
1 |
1 |
| Toxoplasma |
Pyremethamine +Clindamycin |
5 |
4 |
1 |
0 |
0 |
| PML |
HAART |
3 |
1 |
0 |
2 |
0 |
ABCD= Amphotericin B Cholesterol Dispersion
RHEZ = Rifampicin +Isoniazide +Ethambutol +Pyrazinamide
S=Streptomycin
Q= Quinalone (ciprofloxacin)
HAART = Highly active antiretroviral Therapy
Most of the patients with TBM in the present study who had a high GCS at presentation improved better with treatment (10/15) when compared with those who came with low GCS (2/10). Out of the 16 patients who presented with the CCM, 4 patients refused any treatment so they were prescribed oral fluconazole desperately. 12 patients were offered Amphoterecin B (6 patients received ABCD + 6 patients received conventional Amphoterecin B). 4 patients from each group survived (total of 8 patients). Out of them 3 patients are still in follow up for more than 13 months. The remaining 5 patients were lost to follow up. Out of the 4 patients who did not respond, 3 patients expired during the treatment and 1 patient left against medical advice. All the patients of PML were prescribed HAART. Single patient is on follow up after 1 year, but 2 patients were lost to follow up after a median period of 5 months. Only a single patient of toxoplasmosis did not responded favorably to the therapy rest all showed complete response to therapy.
DISCUSSION
HIV infection of the CNS results in damage to the nervous tissue and there has been a geometrical increase in the incidence and recognition of neurological disorders in HIV infected individuals over the past decade (14). Majority of the present study population were in advanced stage of HIV disease (AIDS), confirmed by clinical staging and CD4 level. In India the HIV prevalence in males is higher than females (13) so as in the present study where the male female ratio was 3.7:1. Therefore, females and early HIV infection were under represented in the present study. The CNS involvement is broadly classified into three groups viz by HIV, by opportunistic infections and by malignancies.
Opportunistic infections:
With the advent of HAART the incidence of opportunistic infections decreased remarkably in west with non infectious etiologies leading the list of neurological manifestations. However in countries like India where the prevalence of opportunistic infections is high, it is not surprising to see them leading the list of etiology of neurological conditions (1,2,6,10,11,14,15,16) as observed in our study (46/57 i.e. 81%).
CNS Tuberculosis
CNS tuberculosis can be seen at all stages of the disease (5). Associated intracranial mass lesions suggestive of tuberculoma are more commonly reported in HIV positive individuals (60% vs 14%) as compared to those with seronegative TBM (14) But in the present study only single patient (4%) had tuberculoma which is far less compared to the literature. We found that ADA is a better marker to predict response as the mean levels in patients who responded to anti tubercular therapy (ATT) were 9 IU/L compared with those who did not respond (mean level was 6 IU/L). The level of sensorium was also an important marker of outcome. Most of the patients in the present study who had a high GCS at presentation improved better with treatment (10/15) when compared with those who came with low GCS (2/10).
CCM
The incidence of cryptococcal meningitis varies from 5-28% in different countries (14, 11, 15, 1, 10, 16, 6) In the present study seizures were found more frequently than other studies. Amphoterecin B is the main stay of the treatment in CCM. The introduction of liposome form of Amphoterecin has shown promising results without some of the serious adverse effects (4) though the clinical data are insufficient. We observed similar responses with ABCD and the conventional Amphoterecin B, and interestingly no differences in the side effect profile. In view of the small sample size, further speculation is not made here.
CNS toxoplasmosis
The incidence of toxoplasmosis in different studies has been from 1.33% to 3.3% (15, 11, 15, 1, 10, 16, 6) The incidence in the present study was 1.33%, comparable to rest of Indian studies. One of the interesting features is that CSF picture was normal in all our patients.
PML
PML is one of the rare CNS related disorders observed commonly in HIV patients, caused by JC virus. The favorable prognosis in PML include a CD4+ count >100/ L at baseline and the ability to maintain a HIV viral load of <500 copies per milliliter (7). Similar was our findings and only a single patient out of 3 with PML is doing well as his CD4 levels are 182. All the patients of PML in the present study had seizures as their first manifestation, though it is not a gray matter disease. The possible reasons for seizures could be the demyelinated lesions adjacent to the cerebral cortex acting as irrigative foci, axonal conduction abnormalities, or disturbance of the neuron-glia balance. Moulignier et al also reported 10 HIV patients with PML, presenting with partial or generalized seizures as the first neurological manifestations (12)
Immune Status and CNS diseases:
Opportunistic infections of the CNS, probably with the exception of cryptococcal meningitis usually follow reactivation of latent infections (14). This suggests that a defect in immunoregulation is the principal mechanism leading to the development of opportunistic infections. This was also supported by the finding of the present study that most of the CNS infections (45/57 i.e.79%) occurred at CD4 levels of less than 200. However, a small number of patients (11/57) with a CD4 count between 200 and 500 also had CNS infections (most of them were tubercular meningitis (7 cases), cryptococcal meningitis (3 cases) and a single case of toxoplasmosis). Moreover, the CD4 count in all the patients with cryptococcal meningitis and toxoplasmosis was in the range of 200-250, suggesting a severe immunocompromized state. However CNS tuberculosis cannot be considered as an opportunistic infection in most of the instances as it can be seen in relatively earlier stages of the disease. Barring CNS tuberculosis, any other CNS disease is reasonably good predictor of the advanced HIV infection (CD4<200). Similar observations were made by various other authors across the globe and the inclusion of tuberculosis in clinical case definition of AIDS in countries where the disease is endemic was questioned in prospective and retrospective studies (3).
HIV induced CNS diseases
Primary processes related to HIV infection of the nervous system are reminiscent of those seen with other lenti viruses, such as the Visna- Maedi virus of sheep (9). HIV can affect practically every part of the nervous system ranging from cognitive dysfunction AIDS dementia complex (CNS) to the autonomic neuropathy. It is important to point out that evidence of infection of the CNS with HIV does not imply its role in causation of the disease as 90% of the HIV patients have CNS involvement by HIV though most of them are asymptomatic (9).
The AIDS dementia complex, reported in 66% of the western population is uncommon in India (13%). The rapid improvement in cognitive function noted with the initiation of antiretroviral therapy suggests that at least some component of this problem is quickly reversible (9).We did not encounter even a single case of AIDS dementia complex in our cohort of patients, though majority of our patients were in relatively advanced HIV infection. We could not explain this seemingly paradoxical finding and still studying the cause for the same.
HIV related CNS malignancies
The exact incidence of the CNS malignancies in HIV patients from various parts of India is largely unknown but defiantly les than the west. The non uniform performance of the neuropathological studies, lack of facilities for the diagnosis in most of the centers might contribute to this to some extent. But in the present study also we couldn’t find even a single case of HIV related CNS malignant condition.
CONCLUSION
1. Opportunistic infections are still the leading cause of neurological disorders in our population
2. CNS tuberculosis cannot be considered as an opportunistic infection in most of the instances as it can be seen in relatively earlier stages of the disease. Barring CNS tuberculosis, any other CNS disease is reasonably good predictor of the advanced HIV infection (CD4<200).
3. CSF picture was normal in all our patients of CNS toxoplasmosis.
_4. All the patients with PML had seizures as the initial manifestation
5. AIDS dementia complex and CNS malignancies were not observed in our population
6 We observed similar responses with ABCD and the conventional Amphoterecin B, and interestingly no differences in the side effect profile
REFERENCES
- AGRAWAL SK, MAKHIJA A, ANURADHA S et al The spectrum of opportunistic infections in HIV/AIDS patients in a tertiary care hospital in New Delhi (abstract No.PeB-7220) XIV International AIDS conference July 7-12, 2002.
- ATTILI VS, SINGH VP, RAI M, VARMA DV, SUNDAR S. Evaluation of the status of tuberculosis as part of the clinical case definition of AIDS in India. Postgrad Med J,): 2005: 81: 404-8.
- BADRI M, EHRLICH R, PULERWITZ T, WOOD R, MAARTENS G. Tuberculosis should not be considered an AIDS-defining illness in areas with a high tuberculosis prevalence. Int J Tuberc Lung Dis 2002; 6(3):231-7.
- BENNETT JE. Cryptococcus: Mc graw hill publications Braunwald etal ed Harrison’s Principles of Internal Medicine, 15th ed. 2001. P.1074
- BERENGUER J, MORENO S, LAGUNA F, VICENTE TT, ADRADOS M, ORTEGA A, et al. Tuberculous meningitis in patients infected with the human immunodeficiency virus. N Engl J Med 1992; 326:668-72.
- CHDHAD S , HANDA A, SHARMAS K et al Seizures in patients with HIV infection JAPI:2000:48:573-6
- CLIFFORD DB, JOHN S et al. HAART improves prognosis in HIV-associated progressive multifocal leukoencephalopathy. Neurology 1999; 52:623.
- DISMUKES WE. Cryptococcal meningitis in patients with AIDS. J Infect Dis 1988; 157:624-8.
- FAUCI AS, LANE HC. HIV disease: AIDS and related disorders: Mc graw hill publications Braunwald etal ed Harrison’s Principles of Internal Medicine, 15th ed. 2001.1852
- GHATE MV, DIVAKAR AD, RISBUD AR. Changing trends in clinical presentations in referred HIV persons in Pune, India. JAPI 2002; 50: 671-73.
- KOTHARI K, GOYAL S. Clinical profile of AIDS. JAPI, 2001: 49; 435-39
- MOULIGNIER A, MIKOL J, PIALOUX G, FENELON G, GRAY F, THIEBAUT JB. AIDS associated progressive multifocal leukoencephalopathy revealed by new-onset seizures. Am J Med 1995; 99:64-68
- NACO REPORT ON AIDS IN INDIA, DEC 2005 www.naco.gov.in
- SATISHCHANDRA P, NALINI A, GOURIE DEVI M. et al, Profiles of neurological disorders in associated with HIV AIDS from Banglore, South India (1986-96). Ind J Med Res 2000; 111: 14-23
- SHANKARNARAYAN S, GAGATE A, SAMANI PH Analytical Study of Clinical case profile of opportunistic infections in people living with HIV/AIDS in Mumbai (abstract No.PeB-8215) XIV International AIDS conference July 7-12, 2002.
- SURANA A, VAJPAYEE N, SETH P. Spectrum of opportunistic infections among HIV infected north Indian patients (Abstract No. PeB-7188) XIV International AIDS conference July 7-12, 2002.