
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
ORIGINAL PAPERS / ARTICLES ORIGINAUX
OUTCOME AND PROGNOSIS OF MIDDLE CEREBRAL ARTERY OCCLUSIVE DISEASE IN A SAMPLE OF EGYPTIAN PATIENTS: A PROSPECTIVE HOSPITAL-BASED STUDY
RESULTATS ET PRONOSTIC DE LA MALADIE OCCLUSIVE DE L'ARTERE CEREBRALE MOYENNE CHEZ UN ECHANTILLON DE PATIENTS EGYPTIENS. ÉTUDE PROSPECTIVE EN MILIEU HOSPITALIER
E-Mail Contact - ELSAID Nada :
Nada.neurology@gmail.com
ABSTRACT Background and purpose Changes of the flow velocities of transcranial color coded duplex ultrasound (TCCD) in symptomatic middle cerebral artery (MCA) occlusive disease may be related to the occurrence of further vascular events after stroke. The objective of this study was to investigate the outcome and the prognosis of the MCA occlusive disease. Methods Initial TCCD was done to detect MCA stenosis or occlusion in patients with MCA territory infarction. We repeated TCCD examinations 3 months later and recorded any TIA, cerebral stroke or acute coronary syndrome events during this period. The changes of MCA flow velocities were categorized as normalized, regressive, persistent and progressive groups, according to the changes of MCA velocities at 3 months. Results We studied 31 patients with MCA territory infarction classified according to the initial TCCD results into normal MCA flow velocity group (15 patients), and abnormal MCA flow velocity group (16 patients). Eleven patients of the abnormal MCA group were re-evaluated by TCCD after 3 months as 5 patients died within the 3 months of the follow up. Two patients (18.2%) were normalized, 4 patients (36.4%) had persistent degree of stenosis, and 5 patients (45.5%) showed regression. The number of clinical events showed significant difference (p=0.037) between the normal and abnormal MCA groups. Only 1 patient (6.7%) of the normal MCA group had further cerebral stroke, while 7 patients (43.8%) of the abnormal MCA group suffered of further cerebral stroke. Conclusions Symptomatic MCA stenosis is associated with higher risk of recurrent cerebral stroke. Keywords: Middle cerebral artery, Arterial occlusive disease, Intracranial stenosis, Prognosis, Transcranial color coded duplex. RESUME Introduction Les variations des vitesses d’écoulement au Doppler transcrânien (DT) dans la maladie occlusive de l’artère cérébrale moyenne (ACM) symptomatique peuvent être liées à la survenue d’autres événements vasculaires après un AVC. L’objectif de cette étude était d’étudier le résultat et le pronostic de la maladie occlusive de l’ACM. Méthodes Le DT initial a été réalisé pour détecter la sténose ou l’occlusion de l’ACM chez les patients atteints d’infarctus du territoire de l’ACM Nous avons répété les examens DT 3 mois plus tard et enregistré tout AIT, accident vasculaire cérébral ou syndrome coronarien aigu au cours de cette période. Les changements des vitesses d’écoulement de l’ACM ont été classés en groupes normalisés, régressifs, persistants et progressifs, selon les changements des vitesses de l’ACM à 3 mois. Résultats Nous avons étudié 31 patients atteints d’infarctus du territoire de l’ACM classés selon les résultats initiaux du DT dans le groupe de vitesse d’écoulement de l’ACM normale (15 patients) et le groupe de vitesse d’écoulement de l’ACM anormale (16 patients). Onze patients du groupe ACM anormal ont été réévalués par DT après 3 mois car 5 patients sont décédés dans les 3 mois de suivi. Deux patients (18,2%) ont été normalisés, 4 patients (36,4%) avaient un degré de sténose persistant et 5 patients (45,5%) ont présenté une régression. Le nombre d’événements cliniques a montré une différence significative (p = 0,037) entre les groupes ACM normaux et anormaux. Seul 1 patient (6,7%) du groupe MCA normal a eu un autre AVC, tandis que 7 patients (43,8%) du groupe ACM anormal ont souffert d’un autre AVC. Conclusions La sténose symptomatique de l’ACM est associée à un risque plus élevé de récidive d’AVC. Mots clés: Artère cérabrale moyenne, Doppler transcrânien, Maladie artérielle occlusive, Pronostic, Sténose intracrânienne. INTRODUCTION Ischemic stroke is the second most common cause of death worldwide. Approximately 25% of ischemic strokes are caused by identifiable atherothromboembolism from large artery disease, 25% by small vessel disease, 20% by cardioembolism, approximately 5% by other rare causes cerebral vasculitis, hematological disorders, arterial dissection, and the remainder is of undetermined etiology.(14) Intracranial artery stenosis is a process of dynamic changes. Over a period of time lesions may progress, improve, or not change. The progression of stenosis may lead to increased risk of vascular events. (13) Patients with a recent stroke have an increased long-term risk of new cerebrovascular and cardiovascular events. Estimates of long-term risk of cardiovascular and cerebrovascular events are important for patients who want to know their individual risks, and for the treating physicians because inpatients with increased long-term risk, more expensive or more hazardous interventions could be worthwhile. (16) Transcranial color coded duplex (TCCD) is a noninvasive diagnostic test that is usually used for the diagnosis of intracranial stenosis through visualization of the basal cerebral arteries by color-coding of blood flow velocity. (3) The present study sought to prospectively study the outcome and the prognosis of the middle cerebral artery occlusive disease. PATIENTS AND METHODS In this 1 year prospective study, we selected 31 consecutive stroke patients who were admitted with acute middle cerebral artery territory infarction and who were able to return for a repeated TCCD examination after 3 months. On admission, patients were subjected to thorough history taking including history of previous TIA or stroke, complete neurological examination, evaluation of the severity of neurologic deficits by using the National Institutes of Health Stroke Scale (NIHSS), laboratory investigations (Complete blood count, lipid profile, liver function tests, renal functions tests, coagulation profile, and blood sugar) and electrocardiography. Cerebrovascular ultrasound examination. Transcranial color-coded duplex sonography was done using a Phillips IU22 ultrasound equipment with the use of 2-4 MHz phased array transducer. The hypoechogenic butterfly-shaped mesencephalic brain stem in the midline, surrounded by the hyperechogenic basal cistern is displayed with B-mode ultrasonography y. Subsequently, the color mode can be added to render the basal cerebral arteries visible. The arteries of the circle of Willis can be identified by their anatomical location to the brain stem structures and by the determination of their flow direction based on specific color coding of the blood flow velocity. The middle cerebral arteries (MCA), anterior cerebral arteries (ACA), precommunicating (P1), and postcommunicating (P2) posterior cerebral arteries (PCA) were insonated through the temporal window (Axial plane). Intracranial internal carotid artery (siphon and supraclinoid parts) was also insonated. The peak systolic velocity (PSV) cutoffs for MCA stenosis were 160 cm/s for mild stenosis, 200 cm/s for moderate stenosis, and 280 cm/s for severe stenosis (figure1). (4) Severe MCA stenosis is also detected by dampened flow pattern wave which occur at 85% and 90% degree of stenosis. (19) MCA occlusion was diagnosed if all basal arteries except the MCA were detectable. (8) According to these values, the patients were classified into two groups: normal MCA flow velocity group, and Abnormal MCA flow velocity group in which the patients were further classified into mild stenosis, moderate stenosis, severe stenosis, or occlusion. All patients of the abnormal MCA group were invited to have a repeated TCCD examination 3 months later. Follow-up TCCD examinations were performed with the same TCCD machine and with the use of the same protocol. Categorization of changes in MCA flow velocities at 3 months Follow up TCCD examination after 3 months for patients of the abnormal MCA group. Using the same protocol the patients were categorized into 4 groups based on the initial and repeated TCD findings. In the “normalized” group, patients had initial MCA stenosis or occlusion, but the flow velocities returned to normal after 3 months. The “regressive” group included patients 1) who had lower grading of MCA stenosis, or 2) who initially had an MCA occlusion, which had recanalized but with persistent stenosis. The“persistent” group included patients 1) who had the same grading of MCA stenosis, and 2) who had persistent MCA occlusion, while in the “progressive” group, the initial MCA stenosis was increased in severity or had progressed to occlusion. Clinical Events We followed up the patients of both normal and abnormal MCA flow velocity groups for 3 months for further vascular events; mainly TIA, stroke, and acute coronary syndrome. Statistical Analysis. Data were analyzed using the SPSS, version 21. At first, the normality of data was tested using one sample Kolmogorov Smirnov test. Parametric data were expressed in mean ± standard deviation. Non parametric data were expressed in median, (minimum–maximum). Numbers and percentages were used to describe qualitative data. The Chis quare test was used to test the association between categorical variables. Fisher exact test was only used when more than twenty five percent of the cells had expected count less than five. Independent t test was used to compare 2 groups of parametric data and Mann Whitney U test was used to compare non parametric data. Statistical significance was set at P < 0.05. RESULTS For the normal and abnormal MCA flow velocity group patients, the demographic data, the vascular risk factors and the NIHSS are shown in table 1. There was no statistically significant difference between the 2 groups regarding the demographic data and the risk factors (diabetes mellitus, hypertension, previous cerebrovascular events, cardiac disease, and smoking). The most common risk factor among both the normal and abnormal MCA groups was hypertension (64.7%, and 62.5% respectively), followed by smoking (40%, and 37.5% respectively) (table 1). Transcranial colour coded duplex Examination results: Initial TCCD results: The MCA peak systolic velocities in the initial assessment of the normal MCA flow velocity group ranged between 55-150 cm/sec in the right MCA with median value of 70, 39-160 cm/sec in the left MCA with median value of 80, while in the abnormal MCA flow velocity group the PSVs ranged between 28-233 cm/sec in the right MCA with median value of 113, and 30-652 cm/sec in the left MCA with median value of 168. There was statistically significant difference between the 2 groups in both right and left middle cerebral arteries; p=0.017, and p=0.003 respectively (table 2). The abnormal MCA flow velocity group (16 patients) initial duplex study showed 4 patients (25%) with mild MCA stenosis, 4 patients (25%) with moderate MCA stenosis, 4 patients (25%) with severe MCA stenosis, and 4 patients (25%) with MCA occlusion (table 3). Six patients had bilateral MCA stenosis, but only the symptomatic side was included in our statistics. Follow up TCCD results: Eleven patients of the abnormal MCA group were re-evaluated by TCCD after 3 months, as 5 patients died. The PSVs ranged from 30-210 cm/sec in the right MCA with median value of 88, and 50-228 cm/sec in the left MCA with median value of 250 (table 2). Among these 11 patients, 2 patients (18.2%) had normal MCA peak systolic velocities, 4 patients (36.4%) had mild degree of MCA stenosis, 1(9.1%) patient had moderate stenosis, 3 patients (27.3%) had severe stenosis, and 1 (9.1%) patient had occluded MCA (table 3). Grouping of the changes of the MCA stenosis based on the initial and follow up TCCD grading: Based on the relation between the initial and follow up MCA flow velocity grading, 2 patients (18.2%) were normalized, 4 patients (36.4%) had persistent degree of stenosis, and 5 patients (45.5%) showed regression. None of our patients showed progression of the degree of the MCA stenosis. Among the initial MCA mild stenosis (4 patients); 2 patients were normalized, and 2 had persistent degree of stenosis. While among the initially moderate MCA stenosis (4 patients): 2 patients showed regression, and 2 patients died. In the initial severe MCA stenosis (4 patients): 2 patients showed regression, 1 patient had persistent degree of stenosis, and 1 patient died. In the case of occlusion 2 patients showed regression without administration of tissue plasminogen activator (rTPA) indicating spontaneous recanalization, 1 patient had persistent occlusion, and 1 patient died (table 4). Clinical events: The follow up of the further vascular events among all the study participants showed significant difference (p=0.037) between the normal and abnormal MCA groups. Only 1 patient (6.7%) of the normal MCA group had further cerebral stroke, while 7 patients (43.8%) of the abnormal MCA group suffered of further cerebral stroke. None of the study participants developed any further extracerebral vascular events (acute coronary syndrome, or peripheral ischemia) within the 3 months of the follow up. Disability and mortality data: Seven patients died within the 3 months of the follow up. Two of the normal MCA group patients (13%) died with no available data about the cause of death, while 5 of the abnormal MCA group patients (31%) died due to recurrent ischemic cerebral stroke (19%), non vascular causes (12%) (table 5). There was no significant relation between death and the grade of the initial MCA stenosis, age, or the NIHSS score. DISCUSSION Our findings of the dynamic changes in the MCA flow velocities after 3 months, and the absence of progression of MCA stenosis are almost similar to the findings found by Wong et al., (17) who studied 143 patients with MCA occlusive diseases. The initial TCD findings showed that 75% of the patients had MCA stenosis, while, 25% had MCA occlusion. By analyzing both the initial and repeated TCD findings after 6 months, 29% of the patients were in the normalized group, 62% were in the stable group which included both persistent and regressive grades, and 9% were in the progressed group. Another study conducted by Arenillas et al, (2) on 40 patients who showed an MCA stenosis signal in TCD on admission. An increment or decrement of 30 cm/s in the MCA velocity at the follow up TCD examination compared to the initial one was used to define the stenosis progression and regression respectively. During mean follow-up period of 26.55 months, 32.5% of the symptomatic MCA stenosis progressed, 7.5% regressed, and 60% remained stable. Jeon et al., (7) studied 103 patients with MCA stenosis. After 6 months, 12.6% of the patients showed worsening, whereas 87.4% were stationary or showed regression upon TCD examination. A threshold value of 20 cm/sec for sonographic progression and regression was used. The difference between the results of our study and those 2 studies as regard the changes of MCA flow velocities at the follow up can be attributed to the different definition of these changes among the different studies, the different time interval for the follow up, and the fact that the possibility of the progression depends on the time, and it may be greater as time goes on.(13) Our results suggest that the symptomatic MCA stenosis is associated with higher risk of recurrent cerebral stroke. This comes in line with many other studies that dealt with similar topics, as shown in table 6, and discussed below. Kern et al., (9) observed 102 consecutive patients with significant MCA stenosis or occlusion as demonstrated by TCD and TCCD. Patients with symptomatic MCA disease had an overall stroke risk of 12.5% per year, whereas the annual incidence in primarily asymptomatic MCA disease was only 2.8%. The risk of stroke was significantly lower than that of symptomatic MCA stenosis. This conclusion was also formerly reached by Kremer et al., (10) who followed up 50 white patients with asymptomatic atherosclerotic middle cerebral artery stenosis for mean 27.1 months and came to the conclusions that asymptomatic MCAS of atherosclerotic origin appears to have a benign long-term prognosis. In a prospective study including 138 patients with symptomatic MCA stenosis or occlusion, 23% of patients suffered stroke events during mean follow-up period of 55.8 months. (6) Another prospective study with mean follow-up period of 26.5 months showed that 20% of the patients had cerebral ischemic event in the territory of stenotic MCA.(2) Oh et al., (12) identified 141 first ever stroke patients with symptomatic MCA stenosis or occlusion as revealed by MR angiography. The median follow-up was 27.7 months. The annual recurrence rate of stroke was 4.1%. There was no significant difference between MCA stenosis and MCA occlusion noted for the cumulative probabilities of stroke recurrence or any cause of death. Patients with symptomatic MCA stenosis were regarded as being at high risk for recurrent cerebrovascular events. Miao et al., (11) performed a prospective, randomized, controlled, single-center clinical trial to compare percutaneous transluminal angioplasty and stenting (PTAS) with medical treatment for symptomatic MCA stenosis. The medical treatment group received (aspirin 100 mg plus clopidogrel 75mg/day. The end point events were any kind of ipsilateral stroke or TIA, or death from any origin during 1 year follow up. The 1 year rate of endpoint events was19.4 versus 17.6% (p=0.85) for PTAS and medical group, respectively. Our findings of the dynamic changes and the absence of the relationships between the progression of MCA lesions and clinical events are consistent with previous retrospective reports of ultrasound and angiographic studies conducted by Schwarze et al., (15) and Akins et al., (1) respectively. Wong et al., (17) also recorded the clinical events during a 6-month period, 18 (12.6%) of the patients had further documented vascular events, but in contrary to our data, their data showed that progression of MCA occlusive diseases is associated with an increased risk of vascular events. It is important to point out that the second TCCD in this study was performed after the onset of a recurrent event, if any. This wasn’t feasible in our study and may explain the discrepancy between the results and our inability to find significant correlation between the progression of the MCA stenosis and the increased risk of vascular events. In the present study, the abnormal MCA flow group showed higher yet statistically non significant rate of death compared with the normal MCA flow group. Recurrent cerebral stroke was the most common cause of death (19%) among the abnormal MCA flow group. This was in line with Wong and Li (18) who stated that occurrence of death (20.8%) or cerebrovascular event (29.5%) were more among patients with vascular lesions than those without. In summary, symptomatic MCA stenosis is associated with higher risk of recurrent cerebral stroke. Patients with symptomatic MCA stenosis are regarded as being at high risk for recurrent cerebrovascular events. Therefore, alternative therapies, such as aggressive management of risk factors, other antiplatelet regimens, and intracranial angioplasty/stenting, are needed. The SAMMPRIS (stenting versus aggressive medical management for preventing recurrent stroke in intracranial stenosis) stated that aggressive medical management is superior to percutaneous transluminal angioplasty and stenting (PTAS) with the use of the Wingspan stent system in preventing recurrent stroke in symptomatic intracranial atheroscelerotic stenosis, both because the risk of early stroke after PTAS was high and because the risk of stroke with aggressive medical therapy alone was lower than expected (5). Our study has encountered some limitations. First, the number of the patients was small. Second, the follow up interval was short. Third, the methods, definitions of the degrees of the MCA stenosis, and the MCA serial changes are different among the different studies. These limitations might be the cause of the discrepancy between some of our results and the other studies ‘results. CONCLUSION Our results suggest that the symptomatic MCA stenosis is associated with higher risk of recurrent cerebral stroke in the Egyptian population. Patients with symptomatic MCA stenosis are regarded as being at high risk for recurrent cerebrovascular events. Therefore, alternative therapies, such as aggressive management of risk factors, other antiplatelet regimens, and intracranial angioplasty/stenting, are needed. Further prospective, large sample and observational studies are needed to identify the risk factors leading to advances in intracranial artery stenosis, and find out efficient methods for prevention of further vascular events.
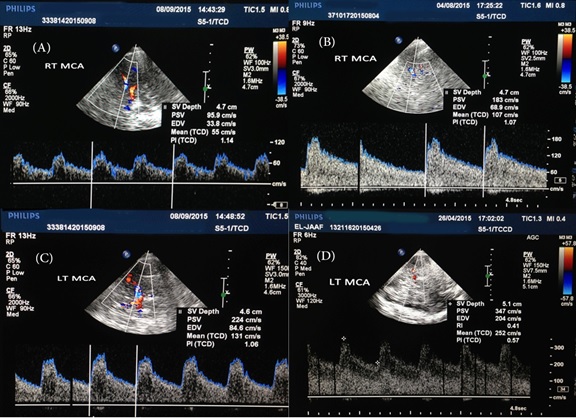 Figure 1: Sample of the TCCD examinations: A) Visualized right MCA and PCA with normal MCA wave form and velocities, B) right MCA mild stenosis, C) left MCA moderate stenosis, and D) left MCA severe stenosis.
Table 1: Demographic characters and risk factors of the study participants
MCA: middle cerebral artery, DM: diabetes mellitus, HTN: hypertension, TIA: transient ischemic attacks, IHD: ischemic heart disease, RHD: rheumatic heart disease, AF: atrial fibrillation, NIHSS: National Institutes of Health Stroke Scale
Table 2: Initial and follow up MCA peak systolic velocities.
MCA: middle cerebral artery
Table 3: Results of Initial and follow up TCCD Findings
MCA: middle cerebral artery, TCCD: transcranial color coded duplex
Table 4: Detailed description of the MCA stenosis changes at the 3 months follow up.
MCA: middle cerebral artery
Table 5: Cause of deaths in the normal and abnormal MCA groups
MCA: middle cerebral artery
Table 6: Trials investigating the risk of further vascular events in symptomatic MCA stenosis
MCA: middle cerebral artery, TCD: transcranial Doppler, TCCD: transcranial color coded duplex, MRA: magnetic resonance angiography, DSA: digital subtraction angiography REFERENCES
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
© 2002-2018 African Journal of Neurological Sciences.
All rights reserved. Terms of use.
Tous droits réservés. Termes d'Utilisation.
ISSN: 1992-2647