ORIGINAL PAPERS / ARTICLES ORIGINAUX
PAINFUL NEUROPATHY IN H.I.V. PATIENTS: ITS RESPONSE TO ORAL PREDNISOLONE
E-Mail Contact - ADAM A.M. :
SUMMARY
Painful neuropathies due to any diseases, cause a lot of morbidity since in most cases they respond poorly to various therapies. It was decided to study the clinical features, electrophysiology and response to a short course of oral prednisolone in H.I.V. patients.
Between 1988 and 1992 seven cases of neuropathies presenting primarily as a painful syndrome in Human Immunodeficiency Virus positive patients were seen in Nairobi, Kenya there were five males and two females. Their age ranged from 45 to 57 years. Four patients had their H.I.V. diseases presenting for the first time as a painful neoropathy. They did not have any clinical feature to suggest related acquired Immunodeficiy state. The other three patients were known H.I.V. related acquired immunodeficiency cases (AIDS). Two of these AIDS cases had neurophysiological evidence of diffuse sensory neuropathy of axonal type. In the rest of the patients nerve conduction studies were normal. All patients had been given various analgesics with carbamazephine and amytryptilline without response. None were given narcotic analgesics. All patients were first given placebo for one week followed by Oral prednisolone at 0.6mg/kg daily. There was no response to placebo but there was remarkable resolution of pain within one week of oral prednisolone.
Therefore a short course of oral prednisolone is useful in the short term management of painful H.I.V. neuropathy.
RESUME
Les neuropathies douloureuses liees a certaines maladies sont la cause d’une morbidite importante, et repondent mal a de nombreuses therapies. Il a ete decide d’etudier les caracteristiques cliniques, electrophysiologiques et les reponses a un traitement de courte duree par la prednisolone chez les patients seropositifs pour le VIH.
Entre 1988 et 1992, 7 cas de VIH (5 hommes et 2 femmes) presentant une neuropathie douloureuse ont ete suivis a Nairobi, Kenya. Leu age variait entre 45 et 57 ans; chez 4 de ces patients le premier signe de la maladie etait une neuropathie douloureuse; il n’existait aucune caracteristique povant suggerer le stade du sydrome d’immunodeficience acquise (SIDA). Les 3 autres patients etaient connus comme ayant un SIDA; 2 de ces patients avaient une neuropathie sensitive diffuse de type axonal, caracteristique a I’examen neurophysiologique. Les enregistrements des vitesses de conduction etaient normaux chez les autres patients. Tous les patients ont ete traites par des analgesiques associes a la carbamazepine et a l’amytryptilline, mais sans resultat favorable. Aucun n’a pris d’analgesique narcotique. Tous les patients ont d’abord ete traites par placebo pendant une semaine, puis par un traitement oral de prednisolone a la dose de 0,6 mg/kg/jour. Il n’y a pas eu de reponse favorable au placebo, mais une remarquable resolution de la douleur avant la fin de la premiere semaine de traitement oral par la prednisolone.
Par consequent, un court traitement oral par la prednisolone est utile a court terme dans la prise en charge de la neuropathie douloreuse du VIH.
Keywords : Neuropathy, HIV, Pain, Prednisolone
Human Immunodeficiency Virus (H.I.V.) can cause a variety of neuropathies as a complication at different stages in the natural history of the disease (1,2). However a distal symmetrical predominantly sensory axonal neuropathy which is often painful is most commonly associated with late stages of H.I.V. infection. The sensory symptoms may be severe with little, if any, sensory or motor signs. This condition may be so painful that the patient is unable to walk because of burning dysethesias. The pathogenesis is not clear. It may be related to direct H.I.V. infection of the nerve or dorsal root ganglia (4). The treatment of such a neuropathy is symptomatic. The tricyclic antidepressants sometime in combination with flupheazine have been the main drugs given over long periods of time (5,6). However many patients obtain no pain relief with these drugs and only occasionally is complete pain relief achieved. The cardiac and central nervous system side effects of tricyclic antidepressants greatly limit their use over prolonged periods of time especially in elderly patients. Therefore as is generally the case of neuropathic pains the treatment of painful neuropathies in H.I.V. remain unsatisfactory.
Most of the research work in H.I.V. is geared to the development of an effective vaccine and more potent anti viral drugs. This is the correct direction of research if the pandemic is to be halted. However as practising neurologists these miserable patients do end up with us and we have to help in putting some sunshine into their bleak life or whatever remains out of it. This study was inspired by an elderly male patient who was otherwise healthy with severe burning pain in the lower limbs and a very painful band-like pain in his epigastrium spreading to the lumbar spine. He had consulted several orthopaedic surgeons and gastroenterologists with several myelograms, barium meals enemas and endoscopies virtually through all his orifices which were all normal, before landing with the author, who did his elisa for H.I.V. which was positive. Various drug regimes did not help him, but his pain resolved within one week of oral prednisolone 40mg O.D. This was tailed off in another three weeks. His pain recurred a year later and he again responded to the same treatment.
Corticosteroids have been used with benefit in several H.I.V. – associated conditions. Theses include idiopathic thrombocytopenic purpura (8). aphthous ulceration (9). lymphoid interstitial pheumonitis (10). Pheumocystis carinii pheumonia (11). They have also been used in the treatment of cerebral oedema associated with central nervous system infection by Cryptococcus (12) and Toxoplasma (13). They may have a role in the amelioration of symptoms of mycobacterium avium in intracellulare infection and of terminal disease. However corticosteroids may possibly induce clinical cytomegalovirus disease and may induce progression of Kaposi’s sarcoma. (14).
METHODS
Patients: Subjects were eligible if they had severe pain enough to seek medical help. Pain was the presenting symptom at that time. At the time of the study they were of good general health no other symptom except pain in the extremities. There was no clinical or laboratory evidence of active infection in any system of the body and no past history of peptic ulcer disease, diabetes or hypertension. None of the patient was on Zidovudine therapy. Each patient underwent a full neurological and general examination. Blood counts, VDRL, ESR, G.T.T. Urea, electrolytes, creatinine, liver function tests, chest xray, serum protein for electrophoresis, T4, T3 TSH, folate B12 levels, cerebrospinal fluid for protein, sugar, cell count and VDRL and nerve conduction studies. Urine examination including culture and sensitivity stool for ova and cysts, chest xray and serum elisa test for H.I.V. were all done. CD counts were not done.
Placebo was given in the first week. Prednisolone was given at a dose of 0.6mg/kg daily as a single dose to the nearest 5mg thereafter. This was a single blind placebo controlled trail. Pain ratings using a 100mm visual analogue scale (VAS) of pain were completed twice before the placebo at an interval of 24 hours. This was then repeated at the end of each week for the next five weeks.
During the medication period the patients were asked for any new symptoms and symptoms of side effects of the prednisolone. Blood pressure and blood sugar was also checked at each visit. Each pair of VAS ratings was averaged before and after one week of placebo and this average was compared to the mean of VAS ratings one week after prednisolone. Prednisolone was then trailed off in the following three weeks. The mean ratings one week after placebo and one week after prednisolone was compared by two-tailed paired test.
RESULTS
Seven patients were seen between 1988 to 1992 and they presented primarily with peripheral painful sometimes burning dysethesias. They were five males and two females. Their age ranged from 45 to 57 years with a mean of 52 years. Four of the patients had nothing in the way of clinical features to indicate H.I.V. infection. Three patients had in the past been treated for Acquired immunodeficiency conditions (AIDS) with known positive serology for H.I.V. infection. None of the patients suffered from post herpetic neuralgia.
All the tests indicated in the methods section were normal. This included he cerebrospinal fluid studies and nerve conduction studies except in two patients known to have AIDS. These patients had mild axonal diffuse sensory neuropathy. Figure I and II shows the nerve conduction results of these two patients. Figure III shows the mean pain intensity ratings before and after one week of placebo, before and after one week of prednisolone. There was a significant decrease of pain (p = 0.02) one week after prednisolone as compared to placebo.
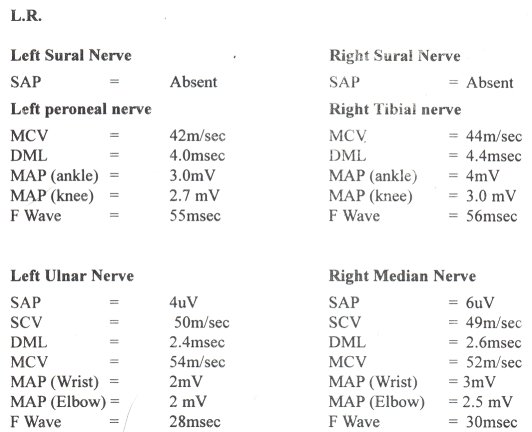
Figure 1
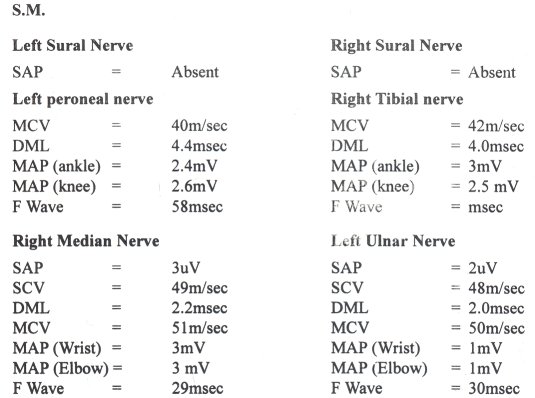
Figure 2
Figure 3
Only one patient complained of ankle swelling during the prednisolone phase. This disappeared on trailing off the prednisolone. No other drug related side effect was recorded during the placebo and prednisolone treatment. There was no symptom or sign to suggest activation of a latent infection.
DISCUSSION
Although sensory neuropathy which is often painful is associated with late H.I.V. infection, this study shows that it can occur at any stage of H.I.V. even before the patients have gross features of immunodeficiency. It can even be the presenting symptom of the H.I.V. state.
Most of these patients had been given tricyclic antidepressants, anticonvulsants, (phenytoin and carbamazepine) fluphenazine or combinations of these drugs before they were referred to the neurology service without pain relief (5,6). None had been given morphine and its analogues. This single blind study shows that prednisolone reduces pain in painful neuropathy associated with H.I.V. when the patients finished their prednisolone course the pain relief was sustained. Therefore cross-over studies could not be done.
The effect of prednisolone in relieving pain in these patients could be at several sites. The steroid could reduce the excitability of neural tissue by alteration of the ratios of extracellular to intracellular sodium and intracellular to extracellular potassium, by decreasing the release of arachidonic acid from phospholipids and hence a decrease in prostaglandins which are essential in the mediation of pain in the peripheral nervous system or by its effects on inflammation and its mediators in the peripheral nervous system (7). The later mechanism is thought to be the most important effect of corticosteroids in this study as the therapeutic effect was long lasting even when the corticosteroids was stopped. All the patients received non-steroidal anti-inflammatory drugs prior to this study without pain relief.
This study may have observer bias and obviously the number of patients is small. Therefore it would be important to carry out a larger and double blind study or even a multi-centre study to study the effects of steroids in the painful neuropathy of early and mid-stages of H.I.V. Nerve biopsies with electron microscopy and immunohistochemistry would also be essential in a more detailed study.
| ACKNOWLEDGEMENTS |
| The author would like to thank Jacqueline Agot for the preparation of this paper. |
REFERENCES
- BREW BJ, PERDICES MJ, COOPER DA: Neurological complications of H.I.V. infection in the absence of significant immunodeficiency. III International Conference on AIDS Washington D.C. June 1987 (abstract W.P. 149).
- CORNBLATH DR, MC ARTHUR JC KENNEDY P.G.E., WITTE A.S. GRIFFIN J.W. Inflammatory demyelinating peripheral neuropathies associated with human T-cell lymphotropic virus type III infection Ann. Neurol. 1986.21: 32-40.
- CORNBLATH DR, MC ARTHUR J. RANCE N.E., GRIFFIN J.W Predominantly sensory neuropathy in patients with AIDS and AIDS related complex. Neurology 1988.38: 794-795.
- RANCE N.E. MC ARTHUR J.C., CORNBLATH DR LANDSTROM D.L. GRIFFIN J.W. PRICE D.L. Gracile tract degeneration in patients with sensory neuropathy and AIDS. Neurology 1988, 38: 265-271.
- ARONOW H.A., BRUCE J.B., PRICE P.W. The management of the neurological complications of H.I.V. infection and AIDS 1988. 2 (supp/1): S151-S159.
- SWASH M. OXBURY J: Clinical neurology. Churchill livingstone 1991.
- GOODMAN AND GILMAN: The pharmacological basis of therapeutics 6th Edition. 1980 Macmillan. New York.
- WALSH C, KRIGEL R., LENNETTE E, KARPA. Thrombocytopenia in homosexual patients-prognosis, response to therapy and prevalence of antibody to the retrovirus associated with the acquired immunodeficiency syndrome. Annals Internal Medicine 1985, 103: 542-545.
- BACH MC, VALENTI A J, HOWELL D.A. SMITH J J: Odynophagia from aphthous ulcers of the pharynx and oesophagus in the acquired immunodeficiency syndrome (AIDS) Annals of Internal Medicine 1988, 109: 338-339.
- RUBINSTEIN A Paedtric AIDS current problems in Pediatrics 1986, 16: 361-409.
- GAGNONS, BOOTA A M FISCHL M A BAIER N, KIRKSEY O W LAVOIE L: Corticosteroids as adjunctive therapy for severe Pneumocystis carinii pneumonia in the acquired immunodeficiency syndrome. New England Journal of Medicine 1990. 323:1444-1450.
- DENNING D, ARMSTRONG R W, LEWIS B. H, STEVAS D A: Elevated cerebrospinal fluid pressures in patients with cryptococcal meningitis and acquired immunodeficiency syndrome. American Journal of Medicine 1991, 91:267-272.
- HOROWITZ S.L. BENTSON J R, BENSON D F, DAROS I PRESSMAN B. GOTTLIEB M.S.: C N S toxoplasmosis in acquired immunodeficiency syndrome. Archives of Neurology 1983 40: 649-652.
- NELSON M R, ERSKINE D HAWKINS D A, GAZZARD B G: Treatment with corticosteroids – a risk factor for the development of clinical cytomegalovirus disease in AIDS. AIDS 1993, 7:375-378.