CLINICAL STUDIES / ETUDES CLINIQUES
PITUITARY METASTASES
METASTASES DE LA GLANDE PITUITAIRE
- Division of Neurosurgery, Groote Schuur Hospital, University of Cape Town, South Africa
E-Mail Contact - DE VILLIERS Jacques C. :
ABSTRACT
Introduction
Metastatic disease of the pituitary is an uncommon clinical problem, although autopsy findings on patients who die of disseminated carcinoma suggest that it occurs more frequently than is clinically evident. Pituitary metastases are often difficult to distinguish from pituitary adenomas both clinically and radiologically.
Materials and Methods: Between 1967 and 2001 six patients with histologically proven pituitary metastases were treated surgically by the Division of Neurosurgery at Groote Schuur Hospital.
Results
The mean age of patients was 55.5 years. Four patients had carcinoma of the lung, 1 of the breast and 1 ‘epithelial’. Clinical presentation included headaches (3 patients), visual deficits (4 patients) and ophthalmoplegia (3 patients). No endocrine dysfunction was found. Radiological investigation was non-specific. The patients all had palliative improvement following surgery but the prognosis was poor with an average survival of 7 months.
Conclusion
Pituitary metastasis is an uncommon diagnosis, the most common primary cancers being breast and lung. The clinical and radiological diagnosis is usually non-specific although diabetes insipidus in a patient with a known malignancy may raise the suspicion. The treatment whether surgical or radiotherapy offers good palliation of symptoms, but the outcome is determined by the metastatic disease and is poor.
Keywords: Africa, pituitary metastasis, diabetes insipidus, transsphenoidal approach, South Africa
RESUME
Introduction
Les métastases de la glande pituitaire sont peu fréquents, même si les résultats d’autopsies pratiquées sur des patients décédés des suites de carcinomes généralisés suggèrent qu’elles sont moins rares que leur expression clinique ne l’indique. Les métastases pituitaires sont souvent difficiles à distinguer des adénomes hypophysaires, tant du point de vue clinique que radiologique.
Matériel et méthodes
De 1967 à 2001, six patients atteints de métastases pituitaires, confirmées par des examens histologiques, ont bénéficié d’un traitement chirurgical dans le service de neurochirurgie de l’hôpital de Groote Schuur, Le Cap.
Résultats
La moyenne d’âge des patients était de 55.5 ans. Quatre d’entre eux présentaient des carcinomes du poumon, un du sein et un « épithélial ». Les symptômes cliniques étaient les suivants : céphalées (3 patients), déficits visuels (4 patients) et ophtalmoplégie (3 patients). Aucun trouble endocrinien n’avait été constaté. Les examens radiologiques avaient été non spécifiques. Dans tous les cas, les procédures chirurgicales ont entraîné des améliorations palliatives, mais le pronostic vital était toujours médiocre puisque le décès est survenu en moyenne 7 mois plus tard.
Conclusion
Les métastases pituitaires constituent un diagnostic rare. Les cancers du poumon et du sein étant les origines primitives les plus fréquents. Habituellement, le diagnostic clinique et radiologique est non spécifique, bien qu’un diabète insipide chez un patient souffrant d’une maladie maligne puisse éveiller les soupçons. Les deux formes de traitement (chirurgie ou radiothérapie) représentent de bons moyens palliatifs au niveau des symptômes . Toutefois, l’issue, fonction du degré métastatique, est généralement fatale.
Mots clés : Afrique, Hypophyse, Métastases, Diabète insipide, Voie transsphénoïdale, République Sud -Africaine
INTRODUCTION
Metastatic deposits in the pituitary are uncommon and this apparent exemption of the pituitary gland from metastatic tumor invasion was first questioned by Benjamin (1857). The first clinical documentation was by Simmonds (1914), and Cushing’s case report in 1923 was the first contribution in English (6). It has become a well-described entity but despite this, it is not frequently recognized clinically.
The incidence ranges from 1.8% – 26.6% in autopsy series (14,22,24), in patients treated by hypophysectomy for advanced breast cancer 3.8% – 5.5% (9,22), and the clinical incidence ranges from 6.8% – 15% (16,24).
MATERIALS AND METHODS
The records of patients with pituitary tumours admitted to the Division of Neurosurgery at Groote Schuur Hospital, University of Cape Town, between 1967 and 2001 were scrutinised for those patients who were operated on for histologically proven metastasis of the pituitary. Six patients were identified and during the same period 582 patients were operated on for pituitary tumours. Pituitary metastases therefore constituted 1% of surgically treated pituitary tumours. The pathology, clinical presentation, diagnostic investigation, management and outcome of these patients were reviewed.
RESULTS
There were 4 female and 2 male patients whose ages ranged from 35 years to 69 years with the mean age of 55.5 years.
In 3 patients the pituitary metastasis was the primary presentation of malignancy. In the other three patients a previous diagnosis of malignancy had been made and the pituitary lesion was a manifestation of metastatic disease. Two of the patients had previously been treated for lung carcinoma three years prior to the presentation of the pituitary metastasis and the other patient had undergone surgery, radiotherapy and chemotherapy for breast carcinoma 14 months earlier. One patient had undergone surgery and radiotherapy for a pituitary adenoma 10 years prior to the presentation of the pituitary metastasis.
The average length of symptoms was 3.25 weeks, which is in keeping with a rapidly growing tumour. Three of the patients complained of headaches, typically frontally or localised behind one eye. Three of the patients also complained of diplopia and three patients experienced fairly rapid deterioration of vision over a period of weeks.
On clinical examination 3 patients were found to have diminished visual acuity: bilaterally in 2, and unilaterally in one. Temporal field defects were demonstrated in 4 of the patients. A complete ophthalmoplegia was found in 2 patients and one patient had bilateral VI nerve palsies with a unilateral IIIrd nerve palsy. One patient with a complete ophthalmoplegia also had bitemporal hemianopia but the two patients with opthalmoplegia had normal visual acuity and fields. None of the patients presented with any evidence of endocrine abnormality, although the patient who had a previous pituitary adenoma was on replacement therapy (Fig.1).
Records of skull x-ray were obtained on 3 patients: one was normal, one showed destruction of the anterior clinoid process and one had destruction of both the anterior clinoid processes and sphenoid body. Cerebral angiography was done on 2 patients: one was normal and the other revealed a highly vascular tumour occupying the sella and cavernous sinus. Four patients had CT scans, of which all showed pituitary tumours with suprasellar extension as well as cavernous sinus and sphenoid sinus invasion in one patient (Fig.2). One patient had multiple lung metastases on chest x-ray, and another had intrabdominal metastases on ultrasound as well as multiple bone metastases on skeletal survey. Endocrine function was found to be normal in all the patients (one patient was on replacement therapy).
All the patients underwent surgery for the purpose of biopsy and decompression of the tumours; 3 by a subfrontal approach and 3 transsphenoidally. Histology of the lesions identified lung carcinoma in 4 cases, breast carcinoma in 1, and epithelial but of uncertain origin’ in 1 case. Three patients had postoperative radiotherapy to the pituitary region, one radiotherapy and chemotherapy and one only received chemotherapy. Five of the patients required no postoperative replacement therapy and one patient continued with his preoperative replacement. All the patients showed clinical improvement following operation.
One patient was lost to follow up but the other five patients all succumbed to metastatic carcinoma with an average survival time of 7 months, and the range being 2 to 18 months (Fig.3).
DISCUSSION
Breast carcinoma is the commonest tumour to metastasise to the pituitary accounting for 50% of pituitary metastases (16). In females, breast, lung and GI tract are the commonest and in males lung and then GI tract (24). Metastases from kidney, bladder, ileum, pancreas, gallbladder, liver, thyroid, stomach, mouth, soft palate, paranasal sinuses, tonsil, nasopharynx, cervix, endometrium, ovary, penis, myeloma, lymphoma and leukaemia have all been described (1-20).
These secondary tumours usually occur in the setting of widespread metastases (5,12,14,27) ranging from 2 – 27 metastatic deposits (24). No cases of pituitary involvement by extension from adjacent osseous metastasis have been reported (24). Pituitary metastases may also be the first manifestation of malignancy (1,12,14,16).
Ntyongo-Pono et al, in their review of the literature, found that 57% of patients were men, 43% women and the mean age of the patients 57.2 years (20).
The posterior lobe of the pituitary is the commonest location for pituitary metastases hence the frequency with which diabetes insipidus has been described as a common presenting clinical feature.
Teears and Silverman (1975) (24), reporting on an autopsy series of 88 cases of carcinomatous metastases to the pituitary gland, found the distribution of lesions as follows: posterior lobe 56.8%, posterior and anterior lobe 12.5%, anterior lobe 13.6%, capsule 12.5% and stalk 2.3%. The posterior lobe receives a direct systemic blood supply, which may explain the greater incidence of its involvement. The anterior lobe being supplied by the portal system of vessels is involved by extension of metastatic tumour from the posterior lobe.
Pathologically, small infarcts may be seen in the anterior lobe, usually not of sufficient size to cause clinically apparent loss of hormonal function. Teears and Silberman (24) found these infarcts in 22 of 24 cases of posterior pituitary involvement or where the stalk was involved. In these cases the portal vessels arising in the posterior lobe, and supplying the anterior lobe, were probably occluded.
Of note is the fact that of the 88 pituitary glands examined by Teears and Silverman, 64 were macroscopically normal and only careful histological examination revealed the carcinoma. The true incidence of metastatic disease to the pituitary is, therefore, largely unknown as judged by standard post-mortem technique.
Max et al (14) found 27 pituitary metastases in 500 autopsy cases of patients with carcinoma in one year (incidence 5.4%). Seventy-one percent presented with diabetes insipidus as the initial symptom, with 82% over their entire course. Fifteen percent presented with cranial nerve palsies; 7% presented with anterior pituitary insufficiency while 11% developed this during the course of their disease. All had widespread metastases.
Hauck et al found diabetes insipidus in 6 out of 639 (0.95%) women with breast carcinoma (9). In his series of 11 patients with posterior pituitary metastases, he observed that diabetes insipidus developed late in the course of breast carcinoma, but earlier in 2 patients with other tumours.
Metastases may present with diabetes insipidus, chiasmal compression, opthalmoplegia or more rarely anterior pituitary insufficiency. Diabetes insipidus has been described by some authors as the most common presenting complaint (5,14), but, Ntyonga-Pono et al in their review of 72, cases found the main clinical signs to be visual disorders in 40.3% and diabetes insipidus in 29.1% (20).
The infrequent occurrence of anterior pituitary insufficiency may be related to the fact that adenohypophyseal destruction must be nearly complete to produce clinical insufficiency, and most patients have widespread metastatic disease and hence a short survival time. It must be noted that anterior pituitary insufficiency may mask the true severity of diabetes insipidus, as polyuria may worsen after cortisone replacement therapy (1,3) due to an increase in renal water clearance following increased glomerular filtration.
Carcinomatous metastasis to the pituitary may simulate a pituitary adenoma (1,14,16) and metastases to a pre-existing pituitary adenoma has also been described (10,12,13,17,26,27). Leramo et al (13) report a case of a 68 year old male, with chiasmal compression, hypopituitarism and hyperprolactinaemia (prolactin 149ng/ml). Biopsy revealed a metastasis from the colon. They suggest that prolactin levels of less than 200ng/ml should lead one to suspect the diagnosis of metastasis, especially in patients who present in an unclassical fashion.
Van Seters et al (26) report a case of a 66 year old female, with a metastasis from an occult gastric carcinoma to a prolactinoma, which when treated with bromocriptine, resulted in a decrease in the serum prolactin, despite progressive growth of the pituitary mass. Zager et al (27) report a case of metastatic breast carcinoma to a pituitary adenoma, presenting with bilateral VI nerve palsies. James et al (10) report a case of an adenoma co-existing with a metastasis from a renal cell carcinoma, which appeared nine years after curative nephrectomy.
The clinical manifestations may provide a clue to the differential diagnosis. Patients presenting with a sellar mass who have a previous history of malignancy, or have a positive skeletal survey, the possibility of metastasis should be entertained. The history of malignancy may be remote e.g. 9 years (12), 31 years (10). Juneau felt that the rapidly progressive visual loss, extraocular movement disorders or facial sensory loss might help distinguish it from a benign adenoma (12).
Radiological studies are often unhelpful in the differentiation between metastases to the pituitary gland, and adenomas (13,14,27). Evidence of bony or soft tissue involvement is not diagnostic, as pituitary adenomas may be invasive or co-exist with metastases (14).
The first evidence of bony metastasis may be found on skull x-ray. Enlargement of the sella without evidence of destruction, sclerosis of the sphenoid bone, destruction of the sella and clivus (12), lytic destruction of the floor of the sella and clivus, and double density of the sella floor (27) have all been described with pituitary metastases but do not necessarily differentiate them from adenomas.
CT scan alone is also not specific for the diagnosis of metastases (7). Both adenomas and metastases are hyperdense compared to brain, often with a mottled appearance, which is thought to represent areas of cystic degeneration or necrosis. Both lesions usually enhance homogeneously with the administration of intravenous contrast material (10,27).
Magnetic resonance imaging cannot be relied on to differentiate between pituitary adenoma and metastases with any certainty. Mayr et al described useful features on MRI including involvement of the hypothalamus or pituitary infindibulum (15,25).
The definitive diagnosis depends on the histological identification of the tumour found at surgery.
Treatment is largely symptomatic as neither surgery nor radiotherapy increases survival, which is determined by the primary malignancy. Transsphenoidal surgery may be used to reduce the mass effect of a pituitary metastasis and thereby provide palliation or to provide a definitive diagnosis in suspicious lesions (2,18) Radiotherapy has proved a useful palliative tool and may, by providing local control of the malignant disease, afford symptomatic relief (18,23). Vasopressin is effective in those patients who present with diabetes insipidus (23).
Outcome is poor in our patients the mean length of survival was 7 months, which compares with the 6 months found by Morita (18).
CONCLUSION
Pituitary metastasis is an uncommon diagnosis. It occurs most frequently in the older patient in whom metastatic disease is most common. Carcinomas of the breast or lung are most frequently involved. In less than half the patients it is the presenting feature of metastatic carcinoma. Clinical and radiological features are non-specific and frequently the diagnosis is only made on histolgical examination. Features that may suggest pituitary metastases include a short history, diabetes insipidus, known malignancy and involvement of the infindibulum or hypothalamus on the MRI. Treatment is palliative with transsphenoidal decompression, radiotherapy and vasopressin providing symptomatic relief. The survival is poor and is determined by the metastatic disease.
| COMMENTARY |
| This is an excellent paper summarizing the cardinal features of metastatic tumors affecting the pituitary gland. Such lesions are regularly encountered and tend to present with a fairly rapid evolution of symptoms. Because these metastases are blood-borne, they often affect the posterior pituitary which has a rich vascular plexus, thus accounting for the relatively common development of diabetes insipidus. Cavernous sinus involvement with resultant diplopia or ophthalmoplegia may occur. Radiotherapy or radiosurgery may improve the prognosis after surgical resection.
Edward R. Laws, Charlottesville, Virginia, USA |
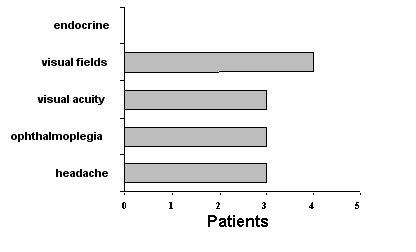
Figure 1. Clinical Presentation
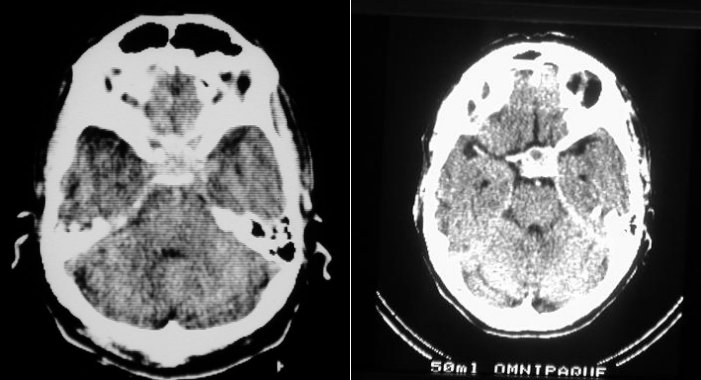
Figure 2. CT scan
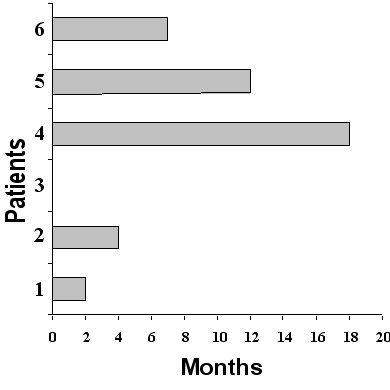
Figure 3. Outcome
REFERENCES
- BOUNAGUIDA R, FERDEGHINI M, FAGGIONATO et al. Intrasellar metastasis mimicking a pituitary adenoma. Surg Neurol 1983; 20: 373-8.
- BRANCH CL, LAWS ER Jr. Metastatic tumours of the sella turcica masquerading as primary pituitary tumours. J Clin Endocrinol Metab 1987; 65(3): 469-74.
- BYNKE O, OTTOSON AM. Is metastatic breast carcinoma in the pituitary a concealed manifestation? Lancet 1982; 2: 1334-7.
- Case records of the Massachusetts General Hospital (Case 33 1983). N Engl J Med 1983; 309: 418-25.
- COX EV. Chiasmal compression from metastatic cancer to the pituitary gland. Surg Neurol 1979; 11: 49-50.
- CUSHING H. Concerning diabetes insipidus and the polyurias of hypophyseal origin. Boston Med Surg J 1913; 168: 908-912.
- DANIELS DL, WILLIAMS AL, THORNTON RS et AL. Differential diagnosis of intrasellar tumours by computer tomography. Radiology 1981; 141: 697-701.
- EICK JJ, Bell KA, STEPHAN MT et al. Metastatic renal cell carcinoma presenting as an intrasellar mass on computerised tomography. J Urol 1985; 134: 128-130.
- HAUCK WA, OLSEN KB, HORTON J. Clinical features of tumour metastasis to the pituitary. Cancer 1970; 26: 256-69.
- JAMES RL, ARSENIS G, STOLER M, et al. Hypophyseal metastatic renal cell carcinoma and pituitary adenoma. Am J Med 1984; 76:337-40.
- JEDYNAK CP, OPROUI A, DELALANDE O, et al. Non adenomatous intrasellar lesions. In Derome PJ, Jedynak CP, Peillon F (eds) Pituitary adenomas. Paris, Asclepios, 1980: 155-169.
- KISTLER M, PRIBRAM HW. Metastatic disease of the sellar turcica. Am J Roentgenol 1975; 123: 13-21.
- LERAMO OB, BOOTH JD, ZINMAM B, et AL. Hyperprolactinoma, hypopituitarism and chiasmal compression due to carcinoma metastatic to the pituitary. Neurosurg 1981; 8: 477-80.
- MAX MB, DECK MDF, ROTTENBERG DA. Pituitary metastasis: incidence in cancer patients and clinical differentiation from pituitary adenoma. Neurol 1981; 31: 998-1002.
- MAYR NA, YUH WT, MUHONEN MG, et al. Pituitary metastases: MR findings. J Comput Assist Tomogr 1993; 17(3): 432-7.
- McCORMICK PC, POST KD, KANDJI AD, et al. Metastatic carcinoma to the pituitary gland. Brit J Neurosurg 1989; 3: 71-80.
- MOLINATTTI PA, SCHEITHAUER BW, RANDALL RV, et al. Metastasis to pituitary adenoma. Arch Pathol Lab Med 1985; 109: 287-9.
- MORITA A, FREDERIC B, MEYER MD, et AL. Symptomatic pituitary metastases. J Neurosurg 1998; 89:69-73.
- NELSON PB, ROBINSON AG, MARTINEZ AJ. Metastatic tumour to the pituitary gland. Neurosurgery 1987; 21: 941-4.
- NTYONGO-PONO MP, THOMOPOULOS, LUTON JP. Pituitary metastases. Presse Med 1999;28(29): 1567-71
- POON MC, PROHAL JT, MURAD TM, et al. Multiple myeloma masquerading as chromophobe adenoma. Cancer 1979; 43: 1515-16.
- ROESSMAN U, KAUFMAN B, FRIEDE RL. Metastatic lesions in the sella turcica and pituitary gland. Cancer 1970; 25:478-80.
- SIOUTOS P, YEN V, ARBIT E. Pituitary gland metastases. Ann Surg Oncol 1996; 3(1): 94-9.
- TEEARS RJ, SILVERMAN EM. Clinico pathologic review of 88 cases of carcinoma metastatic to the pituitary gland. Cancer 1975:36: 216-20.
- VAN de VALDE A, WASSENAAR H, STRUBBE A, et al. Metastatic breast cancer presenting with diabetes insipidus. JBR-BTR 2000; 83(2): 68-70.
- VAN SETERS AP, BOTS GTAM, DUIKEN H, et al. Metastasis of an occult gastric carcinoma suggesting growth of a prolactinoma during bromocriptine therapy: A case report with review of the literature. Neurosurgery 1985; 16: 813-17.
- ZAGER EL, HEDLEY-WHITE ET. Metastasis within a pituitary adenoma presenting with bilateral abducens palsies: Case report and review of the literature. Neurosurgery 1987; 21: 383-87.