CASE REPORT / CAS CLINIQUE
PRIMARY INTRACRANIAL MYXOMA – REPORT OF A RARE CASE AND REVIEW OF LITERATURE
MYXOME INTRA-CRÂNIEN PRIMITIF. PRESENTATION D'UN CAS RARE ET REVUE DE LA LITTÉRATURE
- Department of Neurosurgery, Sanjay Gandhi Post Graduate Institute of Medical Science, Lucknow, India
E-Mail Contact - KUMAR Ashish :
ABSTRACT
Myxomas are benign primary tumors of the heart of mesenchymal origin. Neurological complications attributed to atrial myxoma occurs in 10% to 12% of patients, with ischemic presentation due to cerebral infarct in 83%-89% of cases. Few case reports are available of multiple metastatic myxomas from primary in the heart, despite its slow growing and innocuous histological appearance. Primary intracranial myxomas are extremely rare and only six cases have been reported in literature till date, out of which four were supratentorial in location. As on account of its benign nature, complete surgical resection of the tumor is the recommended treatment.
Key-words: Primary myxoma, intracranial tumor
INTRODUCTION
Myxomas are benign primary tumors of the heart of mesenchymal origin. Neurological complications attributed to atrial myxoma occurs in 10% to 12% of patients, with ischemic presentation due to cerebral infarct in 83%-89% of cases. 1, 2, 3 Few case reports are available of multiple metastatic myxomas from primary in the heart, despite its slow growing and innocuous histological appearance 4. Primary intracranial myxomas are extremely rare and only six cases have been reported in literature till date, out of which four were supratentorial in location 1. As on account of its benign nature, complete surgical resection of the tumor is the recommended treatment.
CASE HISTORY
This 24 year old male presented with two and a half months history of holocranial headache, recurrent episodes of vertigo and visual deterioration. He does not have other complaints related to cardiovascular system.
On neurological examination higher mental function was intact. His visual acuity on his right side was 6/18 with left ocular prosthesis. Fundoscopy revealed late stage of papilloedema. Left sided facial hypoesthesia was there in the distribution of V1, 2, & 3 branches of mandibular nerve, but there was no evidence of any motor involvement. There was mild hemiparesis on the left side (4+/5), with intact sensations all over the body. He had left sided cerebellar lobar signs with wide based gait and tendency to fall towards left. There were no cutaneous stigmata.
His routine investigations were normal including echocardiography. On Computerized Tomography scan head, there was large 5x5cm hypodense lesion present in the region of the middle fossa with extension anteriorly up to temporal tip and posteriorly up to the occipital horn. Lesion was compressing the midbrain and cerebral peduncle medially with effacement of ipsilateral lateral ventricle and third ventricle. Superior extension was up to the sylvian fissure and inferior up to the temporal base. It had irregular lobulated margins with perilesional edema and midline shift. The lesion had mild, homogenous contrast enhancement.
Magnetic resonance imaging brain revealed a T1W isointense and T2W hyperintense lesion of size 6x5x4 cm with lobulations. The lesion was attached on the left side of the tentorium with evidence of dural tail. There was significant perilesional edema with mass effect in form of effacement of the ipsilateral lateral ventricle and dilatation of the contralateral lateral ventricle with compression of the midbrain and midline shift towards right side. Whole enhancing lesion was well demarcated from surrounding parenchyma. [Figure 1] According to these clinico-radiological features, a diagnosis of left superior tentorial based lesion was made.
Left temporal craniotomy was done with complete excision of the tumor. Intraoperatively, the tumour was encountered in the middle fossa region. It had both solid and cystic components with soft to firm consistency, with soft part easily suckable. There was no evidence of any brain invasion. No dural attachment was evident during surgery. Intraoperative impression was of meningioma. Whole of the tumor was excised. Postoperative recovery was uneventful without any fresh neurological deficit. There was gradual improvement in his headache and vertigo, and he was discharged on 7th postoperative day.
Histopathology revealed it to be a Myxoma. Immunohistochemistry also revealed positivity for S100 and vimentin, and negative for epithelial membrane antigen (EMA), Glial fibrillary acidic protein (GFAP), CD34 and desmin. [Figure 2] Ki-67 index is <1%.
DISCUSSION
Myxomas are uncommon benign mesenchymal tumors of the heart which affects young individuals and often their neurological presentation is in form of stroke, due to tumor emboli. Thus most of the patients with atrial myxoma have initial manifestation of CNS due to ischemic events 5. Myxoma has been described in literatures at various places as in gingiva, kidney, breast, bone and various others sites 5.
Occurrence of myxoma in CNS is exceptionally rare. These have been described in some case series as metastatic lesions from primary atrial myxoma 6. Lee et al reported that 12% of cardiac myxomas have some form of CNS manifestations2. Most of these are due to embolic phenomenon leading to ischemic cerebral infarct 2, 3. There are few case reports of multiple CNS metastasis due to tumor embolization from previously operated atrial myxoma 7.
On review of literature, we found only 6 previously reported case of primary intracranial myxomas 1. One of those was very similar to our case, as convexity dural based lesion which mimicked meningioma radiologically. Other one was arising from cranium with no distinction from bony tumors 8. In our case, although there was radiological evidence of dural attachment but no dural attachment was seen during surgery. There is wide variation in radiological findings in these lesions (Table 1).
MRI features play a key role to diagnosis for primary as well as secondary myxoma. Myxomas show an expansile growing pattern frequently limited in the inner and outer tables of the bone. They may be hypodense to isodense in CT scans, and show variable enhancement pattern. It usually shows expensile pattern of the mass as seen in our case. The classical MRI pattern is the heterogeneous composition of the lesion. The MRI signal characteristics of myxomas are low signal intensity in T1-WI, and hyperintensity with heterogenicity in T2-WI images. Although in our patient lesion is intense hyperintense in T2-WI, but it shown homogenous. Clinical presentation and demographic data of myxomas may resemble many other neoplasms and vascular lesions at this site. Chondrosarcoma, chordoma, metastatic tumors of the skull, hemangiopericytoma, meningioma and other neoplasms of the dura and skull base are the most frequently encountered lesions in differential diagnosis.
Total surgical resection follow the same principal with removal of attached dura if found during the surgery. Total excision should be done as these are benign lesions and it provides excellent prognosis. Even for atrial myxomas, this surgical principle is followed 8.
Immunohistochemistry offers the basis of identification of this unusual tumor. Histopathology is the key to suspicion with its myxoid material with uniformly scattered spindle shaped cells having scant cytoplasm 9, 10.
CONCLUSION
Myxomas are rare neoplasms and only 6 cases have been identified till date of primary intracranial myxomas. Cardiac myxomas may present as stroke due to embolism. Intracranial location has its own surgical indication with complete resection as a goal of surgery. Correct diagnosis should be based on immunohistochemistry to rule out other malignant tumors or metastasis. Further collaborative studies are needed to identify its origin and to formulate better treatment guidelines.

Figure 1
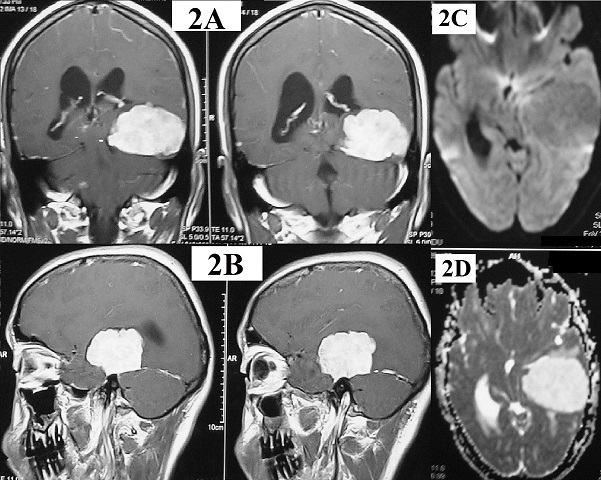
Figure 2
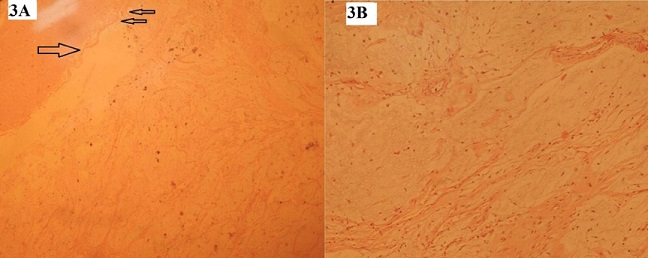
Figure 3
Table 1: Summary of all case reports of intracranial myxoma
| Authors |
Age/sex |
Location |
Radiological findings |
Surgical excision |
| Graham et al (7) |
Adolescent/F |
Right fronto-parietal |
inhomogeneously enhancing mass |
Total excision |
| Menon et al (1) |
25yr / M |
Left parietal |
Isodense enhancing mass |
Total excision |
| Klein et al (13) |
32yr/ F |
Posterior fossa |
inhomogeneously enhancing lesion |
Excision extent not clear |
| Kawatra et al (11) |
12yr / M |
Occipital |
expansile lytic sclerotic lesion arising from the right occipital bone showing prominent trabecular pattern with no soft tissue enhancement |
Near total excision |
| Nagatani et al (5) |
38yr/ M |
Intrasellar & suprasellar |
inhomogeneously enhancing lesion |
Excision extent not clear |
| Oruckaptan et al (12) |
34yr/ M |
Right temoral |
inhomogeneously enhancing mass lesion arising from the temporal bone |
tumor was removed with adjacent invaded dura |
| Ashish et al |
24yr /M |
Left temporal |
Hypodense lesion with mild, homogenous contrast enhancement |
Total excision |
REFERENCES
- MENON RK, GOEL A, SHAH A, GOEL N, RAJASHEKHARAN P. Primary intracranial myxoma of the parietal region: Illustrated case report. J Neurooncol 2008 Jun; 88:157-60.
- LEE VH, CONNOLLY HM, BROWN RD JR. Central nervous system manifestations of cardiac myxoma. Arch Neurol 2007 Aug; 64:1115-20.
- EKINCI EI, DONNAN GA. Neurological manifestations of cardiac myxoma: a review of the literature and report of cases. Intern Med J 2004 May; 34:243-9.
- ALTUNDAG MB, ERTAS G, UCER AR, DURMUS S, ABANUZ H, CALIKOĞLU T, OZBAGI K, DEMIRKASIMOGLU A, KAYA B, BAKKAL BH, ALTUNDAG K. Brain metastasis of cardiac myxoma: case report and review of the literature. J Neurooncol. 2005 Nov;75(2):181-4.
- OSTERDOCK RJ, GREENE S, MASCOTT CR, AMEDEE R, CRAWFORD BE. Primary myxoma of the temporal bone in a 17-year-old boy: case report. Neurosurgery 2001 Apr; 48:945-8.
- GRAHAM JF, LOO SY, MATOBA A. Primary brain myxoma, an unusual tumor of meningeal origin: case report. Neurosurgery 1999 Jul; 45:166-70.
- NG SH, TANG LM, WAI YY, TSAI CC, TEH BC. Primary Myxoma of the cranium: CT findings. J Comput Assist Tomogr 1989 Sep-Oct; 13:903-5.
- SEO IS, WARNER TF, COLYER RA, WINKLER RF. Metastasizing atrial myxoma. Am J SurgPathol 1980 Aug; 4:391-9.
- KAWATRA M, BHANDARI V, PHATAK S, KULKARNI D. Primary occipital myxoma: A rare case report. J Pediatr Neurosci 2013; 8:129-131.
- ORUCKAPTAN HH, SARAC S, GEDIKOGLU G. Primary intracranial myxoma of the lateral skull base: a rare entity in clinical practice. Turk Neurosurg. 2010 Jan; 20(1):86-9.