NEUROEPIDEMIOLOGY
RE – APPRAISAL OF RISK FACTORS FOR STROKE IN NIGERIAN AFRICANS – A PROSPECTIVE CASE – CONTROL STUDY
REEVALUATION DES FACTEURS DE RISQUES DES ACCIDENTS VASCULAIRES CEREBRAUX DANS UNE POPULATION NIGERIANE. ETUDE PROSPECTIVE
- Department of Medicine, University Teaching Hospital, Benin City, Nigeria
- Dept. of Medicine, LUTH, Lagos
E-Mail Contact - AMU E. :
ABSTRACT
Stroke is one of the major challenges facing medicine with a frightening statistics of being the second leading cause of death and the leading cause of physical disability worldwide. Identification and management of risk factors remains the key to reducing morbidity and mortality from stroke.
Eighty patients with clinical presentation of stroke were recruited consecutively from the Emergency Departments of the University Teaching Hospital and Specialist Hospital – both situated in Benin City, Nigeria. The patients were followed up for a two year period (June 2000 – June 2002) and risk factors analysis was done on all patients. The patients were compared with eighty age and sex matched subjects without stroke (controls).
Hypertension remained the dominant risk factor with an odds ratio of 2.68 (95% CI 1.29 – 5.59). Diabetes mellitus independently conferred a risk of 3.23 (95% CI 1.09 – 5.71) and in combination with hypertension enhanced stroke risk (odds ratio 7.21; 95% CI 5.79 – 13.27; p<0.05).
Cigarette smoking, obesity, atrial fibrillation and physical inactivity significantly increased stroke risk (p<0.05). On the other hand, dietary habits, alcohol consumption and serum cholesterol were not important risk factors in Nigerians.
This study emphasized the significance of optimal blood pressure and glycemic control in stroke prevention. The message for all is to exercise, maintain a healthy weight, avoid smoking and monitor blood pressure and glucose levels regularly.
RESUME
Introduction
En étant la deuxième cause de mortalité et l’une des causes majeures de handicap dans le monde entier, les accidents vasculaires cérébraux (AVC) représentent un défit médical majeur. L‘identification et la maîtrise des facteurs de risque restent la clé de la réduction de la mortalité et de la morbidité.
Materiel et Methode
80 patients présentant des signes vasculaires cérébraux ont été recrutés consécutivement au niveau du service des urgences et du service de neurologie du centre hospitalier universitaire ; Benin (Nigeria). Les patients ont été suivis pendant une période de deux ans (juin 2000 – juin 2002) et les facteurs de risque ont été analysés chez tous les patients . Les patients ont été comparés avec un groupe témoin de 80 personnes sains, sans notion d’AVC.
Résultat
L’hypertension artérielle reste le facteur dominant avec un odds ratio de 2,68 (95 % CI 1,29 – 5,59) le diabète sucré confère indépendamment un risque de 3,23 (95 % CI 1,09 – 5.71) et en combination avec l’hypertension artérielle le risque de survenu d’un AVC est plus élevé (odds ratio 7,21 ; 95% CI 5,79 – 13,27 ; P inférieur à 0,05, la consommation de cigarette, l’obésité, la fibrillation auriculaire et l’inactivité physique augmentent de manière significative le risque d’AVC (P inférieur à 0,05) Par ailleurs, les habitudes diététiques, la consommation d’alcool et l’hypercholestérolémie n’était pas un facteur de risque important.
Conclusion
Cette étude insiste sur la nécessité de contrôler la pression artérielle et la glycémie dans le cadre de la prévention des AVC. Il importe dans cette optique de veiller également au poids, à éviter la consommation de tabac avec pratique d’un exercice physique. La pression artérielle et la glycémie devront être contrôlés régulièrement.
Keywords: Africa, Nigeria, risk factor, stroke, Afrique, Nigeria, facteur de risque, accidents cardio-vasculaires cerebraux
INTRODUCTION
Cerebro-vascular accident or stroke has remained a major challenge to physicians worldwide. It is still the third leading cause of death in the United States[4,9] and the leading cause of serious long – term disability[7,14]. It is estimated that 700,000 American residents experience a new or recurrent stroke, with an estimated 500,000 having their first stroke[9]. This disease was believed to be rare in the black Africans five decades ago[15], but is now as common in developing countries such as Nigeria and other African countries as in the Western world. Recently, there are reports indicating that stroke is the leading cause of neurological admissions in most tertiary hospitals in Nigeria, taking over from central nervous system infections reported in earlier studies[29,32]. This is an indication that it is assuming a significant dimension among the non-communicable diseases in African countries, including Nigeria. It accounted for 0.92 – 4% of hospital admissions and 2.83 to 4.52% of total deaths[28,33]. Though the actual incidence of stroke in Nigeria has not been established but reports indicate that the incidence is likely to be high and the mortality increasing, as in other African countries[13,27].
Stroke accounted for 10 – 12 percent of all deaths in industrialized countries and about 88% of the deaths attributed to stroke are among people over 65 years[4]. In 1999, a total of 167,000 deaths from stroke occurred in the United States; of these approximately half occurred out of hospital[9]. Though it appeared death rates from stroke have fallen dramatically in recent decades in most industrialized nations, with Japan experiencing the most precipitous fall[6]. Yet these trends in stroke mortality cannot be fully explained but they are not unlikely to be related to the changing risk factor levels over time.
The modification and treatment of risk factors such as hypertension, diabetes mellitus, hyperlipidemia and atrial fibrillation directly influence incidence and indirectly affect case fatality of stroke, as the natural history of the disease is altered[23]. The identification and understanding of the magnitude of these risk factors will go a long way in stroke prevention, notwithstanding reports of lack of risk factors in young Africans[3].
In Nigeria, however, there are very few reports that have adequately addressed this issue in recent times. Studies in Nigerian Africans have shown that hypertension is the dominant risk factor for stroke8,16,26,33-35 and its control has been associated with reduction in risk in other populations[10,44]. Diabetes mellitus[33,35] and homozygous sickle cell disease (in children only)[1,16] have also been reported as major risk factors, though the latter has not been shown to be important in more recent reports.
Other identifiable risk factors reported in most western countries have not been investigated extensively among Nigerians, though some reports have mentioned obesity, anemia, dehydration, infections (including HIV infection[16,24]), under-nutrition and congestive heart failure[36]. Smoking has not been reported as a major risk factor for stroke in Nigerians[31].
This analytical case – control study was designed to re-evaluate the risk factors for stroke in Nigerians with the objective of determining their significance and relative magnitude, and thus improving our understanding of the roles of these factors in our stroke patients. This will, in turn, aid in prevention of this disease.
METHODOLOGIE
Eighty consecutive patients with clinical diagnosis of stroke and above 14 years of age were recruited from the Emergency departments of the University Teaching Hospital and State Specialist Hospital in Benin City, Nigeria and followed up between June 2000 and June 2002. Eighty consecutive age- and sex- matched subjects without clinical evidence of stroke were recruited within the study period as controls. Informed consent was sought from subjects and/or relatives when necessary, and approval was received from the Hospital Ethics committees.
All newly admitted cases of stroke were seen, interviewed, clinically evaluated and investigated using a questionnaire and management plan by authors. The questionnaire was designed to obtain information on demographic data (age, gender marital status), social factors (level of education, occupation, income, smoking, alcohol consumption, physical exercise and dietary habits), clinical factors (blood pressure; past history of hypertension, stroke, and diabetes mellitus; family history of hypertension, diabetes mellitus and stroke, presence of heart disease, obesity (body mass index (BMI) calculated and waist circumference measured), carotid artery bruit, cardiomegaly, cardiac murmurs and fundoscopic changes; neurological status (level of consciousness, pattern of deficit) and investigation outcomes (fasting blood sugar, serum cholesterol, hemoglobin levels, hemoglobin genotype, erythrocyte sedimentation rate and CT brain scans).
Controls were recruited from the general outpatient department and these were patients without stroke or past history of stroke. They were similarly interviewed, clinically assessed and investigated. Benin City is a cosmopolitan region in southern Nigeria with a population representative of Nigerian ethnic groups.
Clinical Case Definition
The diagnosis of stroke was made based on the abrupt onset of focal neurological deficit (hemiparesis, hemiplegia, aphasia, facioparesis, or homonymous hemianopia with or without alteration in level of consciousness)45. Hypertension is defined as systolic blood pressure of > 140mmHg and /or diastolic pressure > 90mmHg or a blood pressure below this figure in previously diagnosed individuals on therapy37. Diabetes mellitus is defined as fasting blood sugar > 119mg% or previous history of diabetes with or without therapy37. Obesity was defined as Body Mass Index > 30kg/m2 and/or waist circumference > 40 cm. Smoking was graded as light < 10 Sticks/ day; moderate 10 - 40 sticks/ day and heavy > 40 sticks/day.
Alcohol consumption was categorized as (i) Heavy > 100gm ethanol / day; (ii) Moderate 50 – 100gm ethanol /day; (iii) Light < 50 gm ethanol/day and (iv) Non - drinker.
Socio-economic stratification was based on income and occupation [22].
STATISTICAL ANALYSIS
This was done with the aid of the Epi – Info software version 6.04, using the Mantel-Haenszel chi-square test for matched analysis and the odds ratios (OR) to express the level of significance and magnitude of risk factors. The multivariate logistic regression analysis was used to measure the relative contributions of various risk factors.
RESULTS
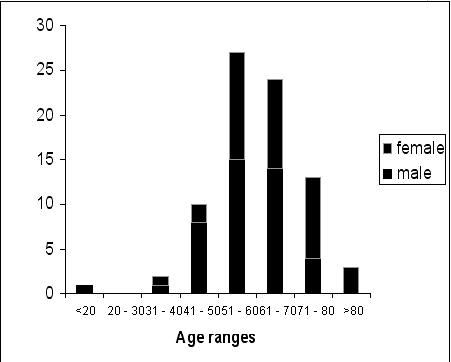
A total of 160 subjects comprising eighty stroke patients and eighty controls were studied. The mean ages of the patients and controls were 60.58+ 12.42 years and the male/female ratio was 1.2:1 for both groups to ensure one to one matching. Every stroke patient was matched for age and sex with a control (individual matching). The age group 51 – 60 years accounted for majority of stroke patients (33.70%) followed by 61 – 70 years (30%) refer figure 1.
STROKE TYPES
The stroke types were classified using the clinical indices (i.e. level of consciousness, headaches, vomiting, nuchal rigidity, presence of Kernig’s sign and presence of atherosclerosis) and the CT brain scan findings. Majority of the patients had ischemic type (73.75%) while intra-cerebral hemorrhage was found in 23.50% and sub-arachnoid hemorrhage in 3.75%.
RISK FACTOR ANALYSIS
There was no statistical difference between the patients’ and the controls’ levels of education (p > 0.05). Most of the patients belonged to the low socio – economic group (63.75%) but this factor, when compared with the controls, was not a strong factor in predisposing to stroke (OR = 1.37; 95% CI 0.87 – 3.18).
Hypertension was more common in the stroke group (82.50%) than the control group (63.75%). This same trend was observed for diabetes and other risk factors (table I). Thirty four patients, comprising 23% of all patients with both hypertension and diabetes, had both risk factors while only 5 (3%) of the controls had both.
Twenty four (30%) of the patients took alcohol in appreciable amounts compared to fourteen (17.15%) control subjects. This difference did not reach statistical significance (OR=1.9, 95% CI 0.96 – 4.27; X^2= 2.84: p> 0.05). Cigarette smoking was a strong risk factor with odds ratio of 10.01 (95% CI 1.23 – 81.06, X^2=5.23; p< 0.05), though only 11.25 percent of the patients smoked compared to 1.25 percent of the controls. Thirty four (42.50%) of the patients admitted to sedentary life style (with little or no physical exercise) and this increased the risk of stroke about three fold compared to controls (OR 3.2, 95% CI 1.57 - 6.55 ; X^2 =10.62, p < 0.05).
The dietary habit of the patients was not a significant risk factor (OR 1:3, 95% CI 0.78 - 3.09; X^2 = 0.66, p>0.05). Hypertension and diabetes independently increased the risk for stroke by three fold (OR 2.68; 95% CI 1.29 – 5.59 and 3.23; 95% CI 1.09 – 5.71 respectively, p < 0.05) and the presence of both further increased the risk seven fold (OR 7.21; 95% CI 2.61 - 19.75). Obesity, present in 30% of the stroke patients, was associated with eight fold risk (OR 8.53, 95% CI 2.02 - 13.80; X^2 =16.9, p < 0.05).
Though the presence of atrial fibrillation increased the risk of stroke in these patients (OR 2.74; 95% CI 0.60 - 26.16), the observation was not statistically significant, but family history of stroke was significantly associated with increased risk (OR 3.0, 95% CI 1.01 - 5.37; X^2 =6.25, p < 0.05). Furthermore, significant differences were observed in the means of the fasting blood sugar (means for stroke patients and controls were 126.42±67.47mg/dl and 93.20±30.10mg/dl respectively) and the hematocrit levels (means for the stroke patients and controls were 38.49±6.23 and 33.87±9.09 respectively) of the two groups (p< 0.05) but the serum cholesterol levels (means for stroke patients and controls were 174.64±47.75mmol/l and 172.55±34.15mmol/l respectively) were not significantly different (p>0.05). None of the patients or controls had received treatment for hypercholesterolemia. Using multivariate regression analysis, hypertension was the most potent risk factor (p = 0.003) followed by cigarette smoking (p = 0.017), obesity and diabetes mellitus (p=0.023 and p=0.035 respectively).
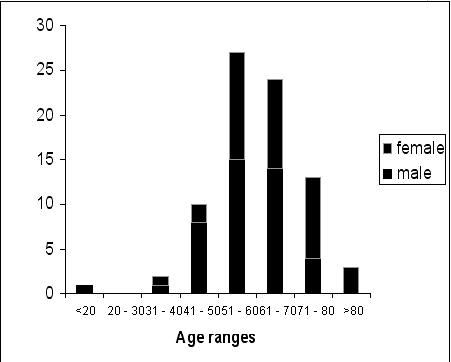 Fig 1 – AGE DISTRIBUTION OF STROKE PATIENTS
| Risk factors |
Patients |
Controls |
|
| Hypertension |
66 (82.5%) |
51 (63.75%) |
OR 2.68; (95% CI 1.29 – 5.59) p<0.05 |
| Diabetes |
21 (26.25%) |
10 (12.5%) |
OR 3.23; (95%CI 1.09 – 5.71) p<0.05 |
| Obesity |
24 (30%) |
6 (7.5%) |
OR 8.53 (95%CI 2.02 – 13.80) p<0.05 |
| Atrial fibrillation |
5 (6.25%) |
1 (1.25%) |
OR 2.74 (95% CI 0.60 – 26.16) p>0.05 |
| Family history of stroke |
20 (25%) |
10 (12.5%) |
OR 3.0 (95% CI 1.01 – 5.37) p<0.05 |
| Cardiac lesion (1 cardiomyopathy, 1 rheumatic valvular disease) |
2 (2.5%) |
0 (0%) |
P >0.05 |
DISCUSSION
Despite significant advances in the understanding of its underlying pathophysiology and the development of more effective methods of its management, stroke continues to be a leading cause of mortality and physical disability worldwide [4,7,9,34,41,42]. The basic risk factors for stroke are well known; they include age hypertension, diabetes mellitus, family history of stroke, racial-ethnicity, obesity and hyperlipidemia (dyslipidemia)[39]. Most of information on risk factors has been from developed countries.
Studies among Nigerians and other populations in developed countries have shown that of the various modifiable risk factors for stroke, hypertension is one of the most powerful and prevalent factors for first stroke and also an independent risk factor for recurrent stroke and stroke after TIA [8,26,28,30,31,34,35,41-43]. The risk of stroke is strongly related to both systolic and diastolic blood pressure[31,42]. Hypertension and diabetes mellitus are independently associated with increased risks in our patients. Hypertension is the most prevalent risk factor, but the presence of both conferred higher risk than the two factors separately. The relationship between blood pressure and risk for first stroke or recurrent stroke appears to be log-linear throughout normal range, with a 10mmHg rise in mean arterial pressure conferring about 20% to 30% increase in stroke risk [6,42]. It is established that stroke risk is reduced with optimal control of blood pressure, especially of the hemorrhagic type.
Increasing age has been reported to be the strongest risk factor for cerebral infarction, primary intracerebral and subarachnoid bleed [5,14]. The risks of stroke increased from 3 per 100,000 by third and fourth decade to 8 – 9 per 100,000 in the eight and ninth decade [42]. Most of our patients were in the sixth and seventh decade with a slight male preponderance. This result confirmed the observations in most other African studies [30,33-35]. Cigarette smoking was reported to be insignificant in earlier studies among Nigerians [30,34] but our study revealed that it is a strong risk factor. This result is consistent with the findings from the MRFIT [17] study in developed western countries. The earlier Nigerian studies had fewer numbers of patients and were retrospective, and it is possible that more Nigerians now indulged in cigarette smoking than before.
Elevated serum cholesterol which has been strongly associated with increased mortality from ischemic stroke in western countries[17] has not been a significant factor among Africans [11,42]. The role of diet is not important in our study and has also not been substantiated in the past. This may be responsible for the relatively lower levels of serum cholesterol of the stroke patients and the controls.
Furthermore, obesity, the presence of atrial fibrillation and sedentary life style (physical inactivity) were all associated with increased risk of stroke in our study as has been previously documented [39]. The family history of stroke was also associated with an increased risk in our study. This may be related to inherent biological traits like gender, physical characteristic, and also the presence of familial risk factors like hypertension, obesity and non-insulin dependent diabetes mellitus.
Though we did not evaluate the role of gender, more males were noted to have suffered stroke during the study period. Earlier studies from developed countries also reported slight preponderance of males, especially in middle-age[2,5,6] similar to our observation. The male sex is a risk factor especially for thrombotic stroke, until the eight and ninth decades when gender plays no role in enhancing risk [2,3,29] but the reason for this is not quite obvious. It may be that the female sex hormones are protective before menopause or that the females tolerate hypertension better than the males. The other possibilities include the influence of cultural factors, like the ready accessibility of males to health care and the greater life expectancy found in women. It is also possible that the sex preponderance may be real.
Significant differences were observed in the hematocrit levels of the patients and controls. The direct relevance of this is unclear, though the hypercoagulable states like polycythemia is a risk factor for stroke, the levels noted in our patients did not reach polycythemic levels.
There are other hypercoagulable states like homocysteinuria and primary coagulopathies (antithrombin III, protein S and C deficiency, factor V Leiden and prothrombin 202A gene mutation)25 that predispose and contribute to pathophysiology of stroke, most of which are not routinely screened for in many developing countries, including Nigeria. The presence of antiphospholipid antibodies is relatively a well established, novel risk factor for ischemic stroke in young females [40], but the extent to which these antibodies augment risk is not well characterized. We lack facility for detecting anti-phospholipid and anti-cardiolipin antibodies in our patients.
It is now recognized that transient ischemic attacks (TIAs) are frequent and important precursors of stroke and other vascular ischemic events [18,40,42]. Coronary heart disease, peripheral vascular disease and presence of carotid bruits have not been shown to be very important[31,42], but there are reports of cases in Africans with obliterative arteritis [2,12]. More recently, high fat and sodium diets 38 have been linked to stroke as well as hypokalemia [19].
CONCLUSION
This prospective, case control study has shown that hypertension is still the dominant risk factor for stroke among Nigerian Africans with significant enhancement of risk in the presence of diabetes mellitus. Cigarette smoking, physical inactivity and obesity were important risk factors as well, but hypercholesterolemia, alcohol ingestion and dietary habits were not important risks.
REFERENCES
- AKINYANJU OO. A Profile of sickle cell disease in Nigeria. Ann NY Acad Sci 1989;565:126 -136.
- AGHAJI MA, NZEWI C. Stroke syndrome in the young due to obliterative arteritis of extracranial carotid arteries. Clinical pathological profiles. J Neurosurg Sci 1989;33(4):333-7.
- BAHEMUKA, M. Cerebrovascular accidents (stroke) in young normotensive Africans: a preliminary report of a prospective survey. E Afr Med J 1979;56:661-4.
- BONITA, R. Epidemiology of stroke. Lancet, Feb. 1992;339: 342 -334.
- BONITA R, BEAGLEHOLE R, NORTH JDK. Event, incidence and case – fatality rates of cerebrovascular disease in Auckland, New Zealand. Am J Epidemiol 1984; 120:236 – 43.
- BONITA R, STEWART AW, BEAGLEHOLE R. International trends in stroke mortality: 1970 – 1985. Stroke 1990; 32:989 – 992.
- BOGOUSSLAVSKY, J. Meeting the Challenge of stroke: On the attack. Medicine Review May/June 2000:12 – 16.
- BWALA SA. Stroke in a sub-Saharan Nigerian hospital – a retrospective study. Trop Doct 1989;19(1):11-14.
- CASPER ML, BARNETT E, WILLIAMS GI JR., HALVERSON, JA, BRAHAM VE, GREENLUND, K.J.: Atlas of Stroke Mortality: Racial, Ethnic and Geographic Disparities in the United States, Atlanta, GA. Department of Health and Human Services, Centers for Diseases Control and Prevention, January 2003: 1 -4.
- COLLINS R, MACMAHON S. Blood pressure, antihypertensive drug treatment and the risks of stroke and coronary artery disease. Br Med Bull 1994;50:272-298.
- CONNOR M, RHEEDER P, BRYER A, MEREDITH M, BEUKES M, DUBB A, FRITZ V. The South African stroke risk in general practice study. S Afr Med J 2005;95:334-339.
- COSNETT JE. Stroke in young people: experience in a Bantu hospital. S Afr Med J 1969;43:501-7.
- GARBUSINSKI JM, VAN DER SANDE MA, BARTHOLOME EJ, DRAMAIX M, GAVE A, et al. Stroke presentation and outcome in developing countries: a prospective study in the Gambia. Stroke 2005;36(7):1388-93.
- GAVRAS I, GAVRAS, H. Progress in Stroke Prevention: Lessons from the Latest Trials. Cardiovas Rev. Rep 2004;25 (5): 229 – 231.
- HUMPHRIES SV. A Study of hypertension in the Bahamas. S Afr Med J 1957;31:694 – 699.
- IMAM I. Stroke: a review with an African perspective. Ann Trop Med Parasitol 2002;96(5):435-45.
- ISO H, JACOBS DR, WENTWORTH D, et al for the MRFIT Research Group. Serum cholesterol levels and six year mortality from stroke in 350,977 men screened for the multiple risk factor intervention trial. N Engl J Med 1989;320:904-910.
- IVAN CS, BEISER A, KELLY-HAYES M, et al. Incidence of transient ischemic attacks and risk of stroke in the community: the Framingham Study [abstract]. Stroke 2005;36:426.
- KHAW KAY-TEE, BARRETT-CONNOR E. Dietary potassium and stroke-associated mortality. N Engl J Med 1987;316:235-40.
- KITTNER SJ, GORELICK PB. Antiphospholipid antibodies and stroke: an epidemiological perspective. Stroke 1992;23(2 Suppl):I19-22.
- LAU SM, ALTER M, FRIDAY G et al. A multifactorial analysis of risk factors for recurrent ischemic stroke. Stroke 1994;25:958-962.
- LINDSEY LL, BEACH S. Social Class in Modern Societies. New Jersey, USA: Prentice-Hall Inc. 2000:258.
- MARMOT MG, POULTER NR. Primary Prevention of stroke. Lancet 1992; 339: 344 – 347.
- MOCHAN A, MODI, M, MODI, G. Stroke in Black South African HIV-positive patients – a prospective analysis. Stoke 2003;34:10-15.
- MOONIS M, KOVATS T. Are investigations to look for hypercoagulable states justified routinely in patients with acute ischemic stroke? Ann Neurol 2002;52(suppl 1):S22. Abstract 14.
- NWOSU CM, NWABUEZE AC, IKEH VO. Stroke at the prime of life: a study of Nigerian Africans between the ages of 16 and 45 years. E Afr Med J 1992;69: 384 – 390.
- NYAME PK. Profile of neurological conditions in Accra, Ghana. Ghana Med J 1991;25:342-8.
- ODUSOTE A. Management of Stroke. Nig Med Pract 1996; 32(5/6):54-62.
- OGUN SA, ADELOWO OO, FAMILONI OB, JAYESIMI AEA, FAKOYA EAO. Pattern and Outcome of Medical admissions at the Ogun State University Teaching Hospital, Sagamu – a three – year review. W Afr J Med, 2000; 19: 304 – 308.
- OGUN SA, OJINI FI, OGUNGBO B, KOLAPO KO, DANESI MA. Stroke in south west Nigeria: a 10-year review. Stroke 2005;36(6):1120-2.
- OGUNGBO BI, GREGSON B, MENDELOW AD, WALKER R. Cerebrovascular diseases in Nigeria: what do we know and what do we need to know? Trop Doc 2003; 33: 25 – 30.
- OJINI FI, DANESI M.A. The Pattern of Neurological Admissions at the Lagos University Teaching Hospital. Nig. J Clin Pract. 2003; 5 (1) : 38 – 41.
- OSUNTOKUN BO. Stroke in the Africans. Afr J Med Med Sci 1977;6(2):39-53.
- OSUNTOKUN BO, BADEMOSI O, AKINKUGBE OO, OYEDIRAN ABO, CARLISLE R. Incidence of stroke in an African city: results from the stroke registry at Ibadan, Nigeria, 1973-1975. Stroke 1979;10:205-7.
- OSUNTOKUN BO. Epidemiology of stroke in Blacks in Africa. Hyperten Res Clin Exp. 1994:17 (Suppl 1): S1 – 10.
- OSUNTOKUN BO. Undernutrition and infectious disorders as risk factors in stroke (with special reference to Africans). Adv Neurol 1979; 25; 161 – 74.
- RULAND S, RAMAN R, CHATURVEDI S, GORELICK PB, AAASPS Investigators. Awareness, Treatment and Control of Vascular Risk factors in African Americans with stroke. Neurology 2003; 60(1):64-68.
- STAMLER, J, ROSE G, STAMLER R, ELLIOT P, ET AL. INTERSALT study findings: Public health and medical care implications. Hypertension 1989;14:570-77.
- STRAUS SE, MAJUMDAR SR, MCALISTER FA. New evidence for stroke prevention: scientific review. JAMA 2002;288:1388-95.
- UK – TIA Study Group. The United Kingdom transient ischemic attack (UK-TIA) aspirin trial – final results. J Neurol Neurosurg Psychiatry 1991; 54: 1044-1054.
- WALKER R. Hypertension and stroke in sub-Saharan Africa. Trans R Soc Trop Med Hyg 1994;88:609-11.
- WALKER R. STROKE IN AFRICA: Facing up to a growing problem. Africa Health 1997; 19(4): 28 – 30.
- WALKER RW, ROLFE M, KELLY PJ, GENGE MO, JAMES OFW. Mortality and recovery after stroke in the Gambia. Stroke 2003;34:1604-9.
- 1999 World Health Organization – International Society of Hypertension guidelines for the management of hypertension. J Hypertens 1999;17:151-183.
- WHO MONICA Project, Principal Investigators. The World Health Organization MONICA Project (Monitoring trends and determinants in cardiovascular disease): a major international collaboration. J Clin Epidemiol 1998; 41: 105-114.
|
|