TECHNIQUES
REVIEW OF SURGICAL SCALP WOUNDS CLOSURE IN ILE-IFE, NIGERIA
TRAITEMENT DES PLAIES DU SCALP A ILE-IFE, NIGERIA
- Neurosurgical Unit, Department of Surgery, College of Health Sciences, Obafemi Awolowo University, Ile-Ife, NIGERIA
- Plastic Surgery Unit, Department of Surgery, College of Health Sciences, Obafemi Awolowo University, Ile-Ife, NIGERIA
SUMMARY
Background and Objective:
Low cost and reduced time of closure have compelled us to adopt single layer closure in many of our surgical wounds. This article was designed to review the different methods of scalp wounds closure in our neurosurgical unit in relation to wound edge complications and cosmetic outcome.
Setting and Design: Tertiary Hospital; retrospective analysis.
Materials and Methods:
We retrospectively reviewed 61 patients who had closure of scalp wounds in our centre from July 2000 to December 2003. Wound edge related complications like significant wound edge bleeding, wound edge necrosis, wound infection, cerebrospinal fluid fistula, and implantation cyst as well as cosmetic complaints were taken as outcome measures. Fisher’s exact test was used to test level of significance
Results:
The most common incision was question mark incision in 14 (26.4%) patients, followed by linear incision in 13(24.5%) patients. 80.5% of the patients had single layer closure and multilayered closure was performed in 19.5% of the patients. Minor wound infection occurred in 6 patients who had single layer closure; there were no such complication in patients who had multilayered closure (P = 1.000, Fisher’s exact test mid P). None of the patients developed significant wound edge bleeding, wound edge necrosis, implantation cyst or complained of the cosmetic appearance of the scar. Cerebrospinal fluid fistula occurred in one patient.
Conclusion:
Single layer scalp closure is the most common type of surgical scalp wound closure in our center. It is associated with minimal morbidity. Our patients also seem to be satisfied with the outcome cosmetically. A prospective randomized controlled trial is needed to confirm our findings.
Keywords : Africa,Cosmetics, Cost, Nigeria, Scalp wounds, Afrique, Nigeria, Plaies du scalp
INTRODUCTION
Several attempts have been made over the ages by man to close wounds he created during surgical procedures. The use of insect ticks, animal sinews and other materials have been documented.(2) However, over the ages his attempt at not just closing the wound effectively but also cosmetically with minimal complications and reduced cost has become a major consideration.(1,5,3,9,4) The closure of scalp wound can either be done in layers wherein the galea aponeurotica is first closed with suture before the skin and its subcutaneous layer is sutured.(7) There are various options for the skin closure including the use of absorbable sutures,(10) non-absorbable sutures like nylon, staples or tissue adhesives.(4,11,8) Scalp wound can also be closed in a single layer involving the three structures – skin, subcutaneous layer and the galea aponeurotica.(7)
The double layer closure is favoured in contemporary neurosurgical practice because of presumed less immediate postoperative wound related complications and better cosmetic outcome. The evidence for these advantages are, however, lacking in the literature. We have adopted both single and double layer closure in our practice. Low cost and reduced time of closure are potential attributes of single layer closure and these have made us to use the technique in many of our patients.
In this study, we audit the different methods of scalp wound closure in our center.
MATERIALS AND METHODS
This is a retrospective study conducted to review the methods of scalp wound closure in our neurosurgical unit. Records of the patients who had scalp wound closure between July 2000 and December 2003 were retrieved and information about the type of incision, indication for surgery, suture materials used, duration of suture before removal, method of scalp wound closure and complications related to the scalp wound were documented. The wound related complications like significant bleeding from the wound edge, wound edge necrosis, cerebrospinal fluid fistula, wound infection, implantation cyst and poor cosmetic appearance of the scar were taken as outcome measures. For the purpose of this retrospective study, poor cosmetic appearance was determined by any complaint related to the appearance of the scar by the patients. Significant wound edge bleeding was taken as any bleeding requiring resuturing of the wound or change of dressing soon after surgery. Statistical analysis was performed with SPSS version 11.
RESULTS
There were sixty two procedures in sixty one patients; one patient had surgery twice. The most common incision was question mark incision in 14(26.4%) patients, closely followed by linear incision in 13(24.5%) patients (Table 1). Records of type of incision used were not found in 9 case notes.
Forty one (66.1%) patients had surgeries for cranial and intracranial lesions including sellar, cerebellar and pineal region tumors; meningiomas; skull lesions like fibrous dysplasia; cerebral abscesses and intracranial hemorrhages such as intracerebral, subdural and extradural hemorrhages. Fifteen (24.2%) of the cases were associated with scalp lesions such as scalp masses, dermoid cysts, sebaceous cysts and open depressed skull fractures. Six patients (9.7%) had surgery for hydrocephalus. Six patients had open depressed skull fracture without preoperative evidence of infection. One patient had chronic osteomyelitis of the frontal bone. None of these seven patients developed postoperative wound infection.
All the patients had perioperative antibiotics.
Sutures used included delayed absorbable and monofilament non-absorbable types of different strengths. Nylon -00- was the most common type used in this study in about 23(37.1%) patients. Nylon -0- was used in 14 patients representing 22.6% of cases. The delayed absorbable sutures were used mainly for the first layer in those patients who had multilayered closure.
Records of type of closure were found in 41 patients (66.1%). Thirty three (80.5%) of these had single layer closure while 8 (19.5%) had multilayered closure. Four patients who had multilayered closure had it for suboccipital wounds (Table 2). There were 6 (14.6%) wound related complications among those who had single layer closure. None of the patients who had multilayered closure developed wound related complications. The difference in the frequency of wound related complications for single and multilayer closure was not statistically significant (P = 1.000, Fisher’s exact test mid P).
None of the patients complained about the cosmetic appearance of the scar. There were no records in six (9.7%) patients.
There was documented evidence of wound related complications in only eight (12.9%) of cases (Table 3). Method of closure was not certain in two of these eight patients. Thirty four (54.8%) of the patients had no complications. There were no records in 19(30.6%) patients.
DISCUSSION
Question mark, linear and curvilinear incisions were the most common scalp incisions in our unit (Table 1). The choice of these incisions was largely determined by the pathology and its location as well as the preference and experience of the surgeon.
The choice of monofilament nylon for most of the scalp closure was due to its low tissue reaction and low incidence of allowing microorganisms within its lattices as in multifilament sutures. This was the suture of choice for the skin in both single and multilayer closure. We used absorbable suture like polyglactic acid (vicryl) for the deeper layers of multilayer closure. The latter was only performed in 8 patients and 4 out of these had suboccipital incisions which can only be effectively closed in layers because of multiple tissue planes and nature of the tissues involved. The cost of these sutures for the deeper layers is obviously an additional expense for the patients.
None of our patients developed a major complication related to the wounds. Scalp necrosis occurred only in one patient. The method of closure in this patient was not certain from the record. We often perform a continuous simple suturing for our scalp closure. This has the potential for compromising the vasculature at the edge of the wound leading to skin necrosis.(2) The technique of avoiding too much tension at the wound edge and the rich blood supply of the scalp may explain the rarity of wound edge necrosis among our patients.
Six of the eight complications were minor wound infection.(6) This may suggest a better outcome for those who had multilayer closure because none of the patients who had this method of closure developed wound infection (Table 2). However, this may not be so because the number of patients who had multilayer closure in the series is small. The difference in infection rates was also found not to be statistically significant (P=1.000, Fisher’s exact test mid P). Furthermore, none of the infection constituted a significant morbidity for the patients: none required antibiotics or wound drainage; wound dressing sufficed in all the cases.
Another potential complication of scalp closure is bleeding from the edge of the wound. This was not documented in any of our patients.
The fact that none of the patients complained of the cosmetic appearance of the scars may be because many of our patients are usually very satisfied with their primary problems solved and the scar becomes secondary to them and therefore are not usually bothered by its outcome. There will certainly be a need to do a prospective study to look into our patients’ perspective of their scar.
Poor technique including unnecessary tension may in addition to wound edge necrosis lead to overlapping of the edges of the wound. The buried skin appendages may predispose the patient to implantation cyst later. None of our patients have so far developed this complication.
CONCLUSION
Single layer scalp closure with non absorbable suture is the most common type of surgical scalp wound closure in our center. It is probably cheaper and faster to do compare to multiple layer closure. It is also associated with minimal morbidity. Our patients also seem to be satisfied with the outcome cosmetically. A randomized controlled study will be needed to validate our findings.
Table I: Table of incision type, frequency and complication associated with them
| Type of incision |
No. of patients (%) |
No. of complication |
| Elliptical |
3 (5.7%) |
0 |
| Midline suboccipital |
4(7.5%) |
0 |
| U-shaped |
5(9.4%) |
1 |
| Question mark |
14(26.4%) |
3 |
| Curvilinear |
10(18.9%) |
1 |
| Linear |
13(24.5%) |
1 |
| S-shaped |
2(3.8%) |
1 |
| Bicoronal |
2(3.8%) |
1 |
| Total |
53(100%) |
8 |
Table 2: Type of layered closure and associated wound related complications
| Type of wound closure |
No. of patients |
Wound related complication |
| Single layered closure |
33 |
6 |
| Layered closure |
4 |
0 |
| Total |
41 |
6 |
P=1.000 (Fisher’s exact test mid P)
Table 3: Wound related complications and their frequencies
| Wound related complication |
Frequency |
Percent |
| None |
37 |
59.7 |
| Wound edge necrosis |
1 |
1.6 |
| Wound infection |
6 |
9.7 |
| Cerebrospinal fluid fistula |
1 |
1.6 |
| Nil record |
9 |
14.5 |
| *Death |
8 |
12.9 |
| Total |
62 |
100.0 |
*The deaths were not related to the wound


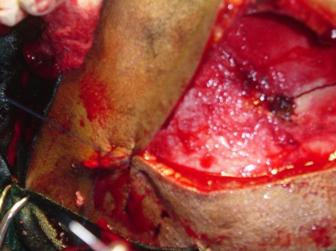
Figure 2: Same patient as in figure 1

Figure 3: Bicoronal scar following surgery for frontal closed depressed skull fracture

Figure 4: Question (?) mark scar following surgery for right frontoparietal extradural haematoma.
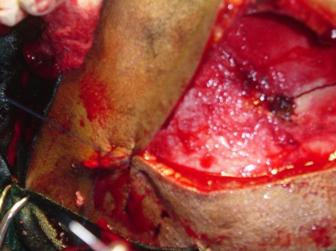
Figure 5 : Intraoperative image showing one layer closure of bicoronal wound in progress
REFERENCES
- BRICKMAN KR, LAMBERT RW. Evaluation of skin stapling for wound closure in the emergency department. Ann Emerg Med. 1989; 18:1122-5.
- HOCHBERG J, MURRAY GF: Principles of operative surgery; antisepsis, technique, sutures and drains. In Sabiston DC, Jr., Editor. Textbook of Surgery; The biological basis of modern surgical practice. Philadelphia. WB Saunders, 1991: 210-290
- JONES JS, GARTNER M, DREW G, PACK S. The shorthand vertical mattress stitch: evaluation of a new suture technique. Am J Emerg Med. 1993; 11: 483-5.
- KANEGAYE JT, VANCE CW, CHAN L, SCHONFELD N. Comparison of skin stapling devices and standard sutures for pediatric scalp lacerations: a randomized study of cost and time benefits. J Pediatr. 1997;130: 808-13.
- KHAN AN, DAYAN PS, MILLER S, ROSEN M, RUBIN DH. Cosmetic outcome of scalp wound closure with staples in the pediatric emergency department: a prospective, randomized trial. Pediatr Emerg Care. 2002; 18:171-3.
- LEAPER DJ. Wound infection. In: Mann CV, Roussell RCG and Williams NS, Editors. Bailey and Love’s Short Practice of Surgery. London: Chapman and Hall, 1995: 63-74
- MEYER CHA. Neurosurgery. In: Rintoul RF, Editor. Farquharson’s textbook of operative surgery. Edinburgh: Harcourt, 2000: 247-268
- MORTON RJ, GIBSON MF, SLOAN JP. The use of histoacryl tissue adhesive for the primary closure of scalp wounds. Arch Emerg Med. 1988; 5: 110-2.
- SCHMIDT DK, MELLETTE JR JR. The dog-ear rotation flap for the repair of large surgical defects on the head and neck. Dermatol Surg. 2001; 27: 908-10.
- START NJ, ARMSTRONG AM, ROBSON WJ. The use of chromic catgut in the primary closure of scalp wounds in children. Arch Emerg Med. 1989; 6: 216-9.
- WANG MY, LEVY ML, MITTLER MA, LIU CY, JOHNSTON S, MCCOMB JG. A prospective analysis of the use of octylcyanoacrylate tissue adhesive for wound closure in pediatric neurosurgery. Pediatr Neurosurg. 1999; 30:186-8.