
|
|
|
CASE REPORT / CAS CLINIQUE
SELLAR TUBERCULOMA: A RARE PRESENTATION IN A 30 YEAR-OLD ETHIOPIAN WOMAN: CASE REPORT
E-Mail Contact - AYELE Biniyam Alemayehu :
biniyam.a7@gmail.com
ABSTRACT Background: Tuberculosis rarely involves the hypothalamo-pitutary axis. Only 1% of CNS Tuberculoma involves sellar and suprasellar structures. It mainly presents with symptoms of chiasmal compression, hypopituitarism and diabetes insipidus due to destruction of pituitary itself. Definitive diagnosis is made by tissue analysis collected by trans-sphenoidal biopsy. Case presentation: We report a 30-year-old female patient from Addis Ababa, who presented with a global headache, blurring of vision, excessive polyuria, constitutional symptoms of tuberculosis and multiple axillary lymph node enlargement. Biopsy from the axillary lymph node showed caseous granulomatous lesions and brain MRI showed mild thickening of the pituitary stalk and mildly enlarged posterior piturary lobe with hypo-sellar extension and mild communicating hydrocephalus. Conclusion: Considering the available evidence a diagnosis of systemic tuberculosis involving pituitary, lung and lymph node was made and a patient was started on anti-tuberculosis medication together with dexamethasone and carbamazepine. Following treatment initiation patient showed significant clinical improvement. After nine months of anti-tuberculosis treatment all brain MRI findings were resolved and patient become symptom free and discharged from care after one year completion of anti-tuberculosis medication. Keywords: Tuberculoma, Polyuria, Pituitary gland, Diabetes Insipidus INTRODUCTION Tuberculosis (TB) is one of the oldest diseases known to affect humans. It is caused by Mycobacterium Tuberculosis which is transmitted through the airborne spread of droplet nuclei produced by patients with infectious pulmonary TB (1). Tuberculous meningitis is the commonest form of CNS TB, but in < 5% Tuberculosis of CNS can present as a granulomatous mass lesion called Tuberculoma. Tuberculoma often involves cerebral cortex, cerebellum and basal ganglia. Tuberculosis involving sellar or supra sellar region is extremely rare, only accounting for 1% of CNS Tuberculoma. The pituitary gland is often affected by tuberculous bacilli either by spread from adjacent brain parenchymal lesions or via hematogenous route. History of concomitant extra sellar or systemic tuberculosis is common among patients with sellar tuberculosis (2). Patients with pituitary tuberculosis present with clinical features related to optic chiasmal compression, hypopituitarism and symptoms of central type of diabetes insipidus (3). CASE PRESENTATION We report a 30-year-old female patient who presented with a productive cough, loss of appetite and significant weight loss of five months duration. Moreover, she had a global headache with occasional blurring of vision and vomiting. Four months before her presentation to the hospital, she developed excessive urination (polyuria) (6-8 liters per day) with associated excessive thirst, for which she drinks more than 6 liters per day. She also reported swelling in her armpit and neck over seven months. She has three children. She denies any complications during any of her pregnancies. The patient is a non-smoker. Upon arrival to the emergency room, she was found to be in hypovolemic shock with an un-recordable blood pressure (BP) and weak radial pulses that improved after fluid resuscitation. The general examination was significant with regard to lymphadenopathy in left cervical and axillary regions. Chest examination revealed bilateral pleural effusions. The neurological examination was unremarkable except mild blurring of the optic disks on funduscopy. Her laboratory results showed mild anemia and an elevated ESR (110mm/hr.). The morning sputum for AFB staining, VDRL and HIV test results were all negative. Serum hypokalemia at admission corrected following parenteral replacement, and all other Serum electrolytes including BUN. Creatinine and liver function testes were in the normal ranges. An upright Chest X-ray showed bilateral pleural effusion without evidences of cardiomegaly. The endocrine work-up was normal, including serum levels of Prolactin, TSH, T3 and T4. The excision biopsy of axillary Lymph node showed caseous granulomatous lesions suggestive of tuberculous lymphadenitis. Three days later the patient was transferred to a medical ward with a working diagnosis of disseminated tuberculosis, involving the pituitary gland, lungs and lymph nodes, and evidences of diabetes insipidus (DI). We performed a water deprivation test for an 8 hour interval during which she produced 5 liters of diluted urine, and normal renal function favoring central DI. The brain MRI revealed, mild thickening of pituitary stalk and an enlarged posterior pituitary lobe with a hyposellar extension and mild enlargement of lateral ventricles (Figure 1a). A transphenoidal biopsy could not be easily performed, but given the clinical presentation supported by a positive lymph node biopsy suggesting tuberculosis, we started the patient on Isoniazid, Rifampin, Pyrazinamide, Ethambutol, and steroids. Three months after initiating anti tuberculosis drugs, the patient showed significant improvement, evidenced by improved appetite, healthy weight gain, resolution of cough, extreme thirst and polyuria. A follow-up brain MRI performed a nine months of anti-tuberculous treatment complete regression of sellar mass and improvement in the size of lateral ventricles (Figure 1b). Finally, the patient was discharged from follow-up clinic with a marked improvement in presenting symptoms after she completed a 12-months course of the anti-tuberculous regimen. DISCUSSION Sellar Tuberculoma is an extremely unusual presentation despite a relatively high prevalence of intracranial tuberculoma in developing countries. They may occur in the absence of systemic tuberculosis. Although 30% of patients have known extra-pituitary tuberculous disease, as seen in our patient, who had concomitant tuberculous lymphadenitis and symptom complex of active tuberculous infection (4). Most of the reported patients with sellar tuberculoma frequently complain of headache and impaired vision. The prevalence of endocrine abnormalities, adenohypophysial hypofunction, hyperprolactinemia, and diabetes insipidus is 77%, 58%, 23%, and 11%, respectively in sellar tuberculosis patients (5). Our patient presented with polyuria and polydipsia with a normal renal profile and was diagnosed with central diabetes insipidus without the evidence of any endocrine abnormalities. Unlike most reported cases thus far, our patient presented with diabetes insipidus of central origin but had normal hormonal profiles. The absences of hormonal abnormalities could be due to isolated involvement of the posterior lobe of the pituitary gland with hyposellar extension and stalk thickening as shown on MRI. A mass in the sellar region has a number of differential diagnoses including, adenoma, cyst of Rathke’s pouch, craniopharyngioma, glioma of the optic chiasm or hypothalamus, meningioma, germ cell tumor, hamartoma, lipoma, dermoid or epidermoid cyst, metastasis; and granulomatous entities like lymphocytic hypophysitis, sarcoidosis, tuberculoma and Langerhans’ histiocytosis. However, a sellar tuberculoma has distinct imaging features on MRI, including multiple coalescing contrast-enhancing lesions, as well as thickening and nodularity of the pituitary stalk. Similarly, the brain MRI in our patient showed thinking of pituitary stalk and heterogeneous mass extending to hyposellar area, which further strengthens the diagnosis of sellar tuberculosis. Definitive diagnosis of pituitary tuberculoma requires confirmation by tissue biopsy, obtained by the transphenoidal route; a procedure that is not available in Ethiopia. The lack of invasive and sophisticated neurosurgical technique for brain biopsy makes diagnosis of sellar tuberculosis more difficult in countries like Ethiopia with limited resources. This is the reason we decided to publish this case, as tuberculosis is endemic in resource-poor setting, where health care professionals needs to have a high index of suspicion, in patients who present with headache, visual complaints, diabetes insipidus, and has imaging finding of a heterogeneous mass in the sellar area, especially with thickening of pituitary stalk. CONCLUSION To our knowledge, this is the first reported case of Sellar tuberculoma from Ethiopia. Although pituitary tuberculosis is rare, it is essential to consider sellar tuberculoma as a possible differential diagnosis in patients who present with a sellar lesion with contrast enhancement and thickening of pituitary stalk. Prompt recognition, rapid diagnosis and early initiation of the anti-tuberculous regimen in such patients result in excellent outcomes with dramatic improvement of clinical symptoms and imaging abnormalities. ACKNOWLEDGMENT We would like to acknowledge the department of neurology. AVAILABILITY OF DATA AND MATERIALS: All are available in the manuscript. AUTHORS’ CONSENT All authors read and approved the manuscript for publication. ETHICS APPROVAL AND CONSENT TO PARTICIPATE Authors’ institution does not require ethical approval for publication of a single case report. Written informed consent was obtained from the patient’s. CONSENT FOR PUBLICATION Written informed consent for publication of clinical details and images was obtained from the patient’s. COMPETING INTERESTS The authors declare that they have no competing interests
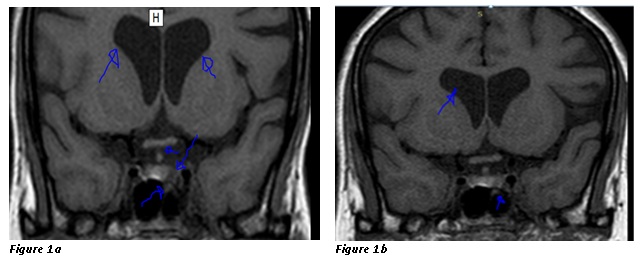 Figure 1a: T1 weighted MRI of the patient taken before Anti-Tuberculous treatment showing mild thickening of pituitary stack and mildly enlarged and heterogeneous posterior piturary lobe with hyposellar extension and moderate enlargement of lateral ventricles.
REFERENCES
|
© 2002-2018 African Journal of Neurological Sciences.
All rights reserved. Terms of use.
Tous droits réservés. Termes d'Utilisation.
ISSN: 1992-2647