
|
|
|
CASE REPORT / CAS CLINIQUE
SURGICAL MANAGEMENT OF PRIMARY OSSEOUS THORACIC SPINE HEMANGIOPERICYTOMA IN A LOW RESOURCE SETTING: A CASE REPORT.
PRISE EN CHARGE CHIRURGICALE DE L'HEMANGIOPERICYTOME OSSEUX THORACIQUE PRIMITIF DE LA COLONNE VERTEBRALE DANS UN CONTEXTE DE RESSOURCES LIMITEES : A PROPOS D’UN CAS ET REVUE DE LITTERATURE.
E-Mail Contact - MEUGA Munkado Wilfried :
Landrix07@gmail.com
ABSTRACT Hemangiopericytoma is a rare vascular neoplasm that arises from pericytes (Zimmermann cell) around the capillary wall. Primary osseous hemangiopericytoma is even rarer, with a high propensity of recurrence and distance metastasis. The management of this tumor is challenging in limited resource setting. We present a case of a 45 years old patient who presented at our clinic complaining of worsening of a chronic back pain, without any neurological impairment. CT scan and MRI revealed a heterogeneous lesion of the vertebral body and left isthmus of T11, with lysis of the posterior wall of the vertebral body and dural sac compression. Piecemeal total spondylectomy of T11 was performed in a two-stage operation through anterior and posterior approaches. The postoperative course was uneventful, with satisfactory clinical outcome and no recurrence 12 months following surgery. In resource limited setting, where total en bloc spondylectomy is very challenging, piecemeal total resection with adjuvant radiotherapy is a reliable option. Keywords: Hemangiopericytoma, thoracic spine tumor, total resection, primary osseous tumor, surgery. RÉSUMÉ L’hémangiopéricytome est une rare tumeur vasculaire qui provient des péricytes (cellules de Zimmermann) situés autour de la paroi capillaire. L’hémangiopéricytome osseux primitif est encore plus rare, avec une forte propension à la récidive et aux métastases à distance. La prise en charge de cette tumeur est difficile dans un contexte de ressources limitées. Nous rapportons le cas d’un patient de 45 ans qui a présenté une douleur dorsale, d’aggravation chronique, sans aucune atteinte neurologique. Le scanner et l’IRM ont révélé une lésion hétérogène du corps vertébral et de l’isthme gauche de T11, avec une lyse de la paroi postérieure du corps vertébral et une compression du sac dural. La spondylectomie totale fragmentaire de T11 a été réalisée en deux temps par voie antérieure et postérieure. L’évolution postopératoire s’est déroulée sans incident, avec des résultats cliniques satisfaisants et aucune récidive 12 mois après la chirurgie. Dans un contexte de ressources limitées, où la spondylectomie totale en monobloc est très difficile, la résection totale fragmentaire avec radiothérapie adjuvante est une option fiable. Mots-clés : Hémangiopéricytome, tumeur thoracique, résection totale, tumeur osseuse primitive, chirurgie. INTRODUCTION Hemangiopericytoma (HPC) is a rare tumor that was first described by Stout and Murray in 1942 (11). Formally known as a rare vascular neoplasm that arises from pericytes of Zimmermann around the capillary wall, it is believed to arise from fibrolastic cells and has been reclassified as being a variant of solitary fibrous tumor (SFT) (1). The World Health Organization (WHO) in 2016 introduced the combined term solitary fibrous tumor/hemangiopericytoma (SFT/HPC) as SFT and HPS share common inversions at 12q13 leading to STAT6 nuclear expression (8). HPCs usually occur in the subcutaneous soft tissue and skeletal system and rarely in the central nervous system and even less common in the spine (2). Primary osseous HPC represent only 0.08% of all primary bone tumors and 0.1% of primary malignant bone tumors and seldom affects the spine (2,6,10,12). HPC exhibit local aggressiveness, with high potential of distant metastases and local recurrences (4,7). Because of the rarity of primary osseous HPC, the clinical features, and the optimal treatment remains unknown. We present a rare case of thoracic spine primary osseous HPC which was treated in our institution. CASE REPORT A 45 years old male, without any family history of neoplastic disease presented with a five months history of back pain, worsened over the last 5 days prior to consultation. The back pain was exacerbated on movement. He denied recent falls or trauma to the back, and had no issues passing urine nor changes to bowel habit. On physical examination, there was a slide kyphosis at T11, associated to a paravertebral and spinal tenderness at level T10-L1. Neither sensory abnormalities nor muscle weakness was noted in his lower extremities. Deep tendon reflexes were normal, and pathological reflexes were not observed in his lower extremities. There was no saddle anesthesia and anal tone was intact on rectal examination. CT scan demonstrated the presence of a heterogeneous lesion of the vertebral body and left isthmus of T11, with lysis of the posterior wall of the vertebral body (Figure 1). On MRI images, the lesion was heterogeneous iso-high intensity signal on T2-weighted (T2W) images with dural sac compression (Figure 2). Cranial and spinal MRI did not show any other lesions in the central nervous system. Abdominal and chest CT showed no abnormalities. The vertebral lesion was biopsied under CT guidance. Subsequently, the pathology examination revealed an HPC. Surgery was indicated to decompress the spinal cord and remove the vertebral lesion for confirmation of the diagnosis. Hence, the surgeon performed a piecemeal total spondylectomy of T11 in a two-stage operation through anterior and posterior approaches. In the first-stage procedure, which was performed using a posterior approach, laminectomy and pediculectomy were performed on T11. The spine from T9 to L1 was stabilized using a pedicle screw and rod system (Figure 3). Autograft from iliac bone was used to secure posterior fusion. One week later, a T11 vertebrectomy of was performed through an anterolateral approach to remove the tumor and anterior reconstruction was performed using a titanium mesh cylindrical cage (Figure 4 A-C). Autograft from the left 11nd rib bone was packed into and around the mesh. The patient’s post-operative course was uneventful, with immediate pain relief after surgery. He was discharged home on post-operative day 10. The thoracic spine CT scan at 2 months post-surgery revealed a complete bone fusion with no implant failure (figure 4 D-E). No recurrence was observed 12 months after surgery. DISCUSSION Primary osseous hemangiopericytoma is a rare and potentially aggressive tumor, with a high recurrence rate and propensity to metastasize (4,6). The recurrence rate for HPC ranges from 50 to 80% and that for metastases from 14 to 30% (6). Solitary segment involvement is found in 50% of cases, commonly occurring in the cervical and thoracic spine. Localized pain is the most common complain, present in up to 80% of cases, and neurological deficit in 65% of cases (4,10). Because of the low incidence of this tumor, it diagnostic features and optimal management are not well defined. However, available evidence suggests that optimal management is through total en bloc resection of the lesion (4,7,10,12). The role of surgery is to relieve pain, preserve functionality, control local recurrence and increase survival. Various surgical techniques have been described in order to achieve the aforementioned goal, including subtotal resection, piecemeal total spondylectomy, and total en bloc spondylectomy (TES). Complete surgical resection with clear margins is fundamental, as extend of resection is correlated with improved long-term and recurrence-free survival (9). This surgery can be a daunting task for the surgeon, due to the anatomy of the spine and neural structures, tumor extension and the risk of excessive bleeding of the tumor during surgery. To reduce the risk of massive hemorrhage during surgery, preoperative embolization of segmental arteries feeding the tumor is recommended whenever feasible (4,6,7,10). This wasn’t done in our case due to the lack of technical support. We performed a piecemeal total resection, with postoperative radiotherapy. Piecemeal total spondylectomy may be associated with tumor cell contamination of the surgical field, with corollary increase in recurrence risk. It is not the case with TES, which enables total resection with clear margins, without surgical field contamination. TES is a procedure with potentially serious complication, especially in resource limited setting where there is poor equipment, absent neurophysiological monitoring and neuronavigation (3,5). Hence, its safety for primary osseous spine HPC should be evaluated. TES can be done with a single posterior approach, which have been made relatively safer and simpler with recent advances. Nevertheless, anteroposterior double approach is safer for the vessels around the vertebral body than TES by a single posterior approach. It has been shown that post-operative radiotherapy may have significant beneficial effects on recurrence, metastases, and survival (6,10). Post operatively, an adjuvant radiotherapy was proposed but declined by the patient. However, the 12 months follow-up CT scan did not show any recurrence. CONCLUSION Primary osseous spine hemangiopericytoma management is challenging in limited resource setting. Because of its high recurrence rate, the goal standard treatment is TES. However, if TES is not feasible, piecemeal total resection with adjuvant radiotherapy is recommended.
FIGURES 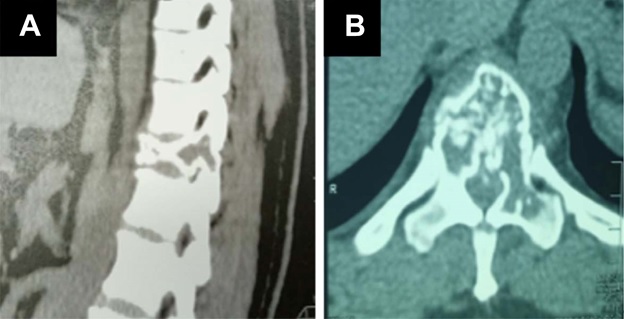 Figure 1: Vertebral compaction at T11 level on a thoracic CT scan. (A) Sagittal plane showing an heterogenous compacted T11 vertebral; (B) Axial plane showing an heterogenous content of the vertebral body with an extention to the left pedicle.
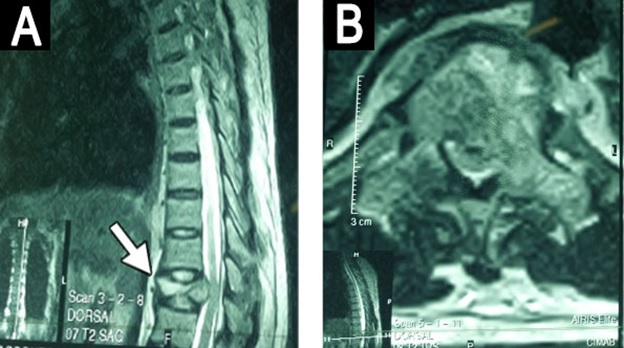 Figure 2: Thoracic spine MRI showing the collapsed T11 vertebra
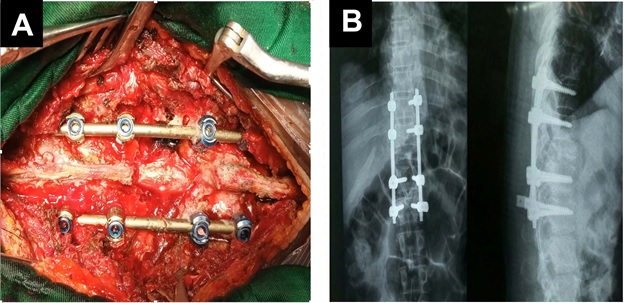 Figure 3: Spinal cord decompression and stabilization through a posterior approach
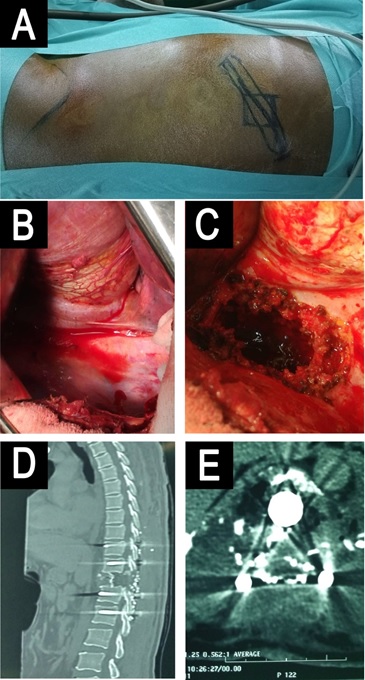 Figure 4: Anterolateral approach for T11 corpectomy and Mesh cage replacement.
REFERENCES
|
© 2002-2018 African Journal of Neurological Sciences.
All rights reserved. Terms of use.
Tous droits réservés. Termes d'Utilisation.
ISSN: 1992-2647