
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
NEUROEPIDEMIOLOGY / NEUROEPIDEMIOLOGIE
THE COST OF TREATING STROKE IN URBAN AND RURAL TANZANIA: A 6-MONTH PILOT STUDY.
LE COUT DU TRAITEMENT DES ACCIDENTS VASCULAIRES CEREBRAUX EN TANZANIE URBAINE ET RURALE : UNE ETUDE PILOTE 6 MOIS
E-Mail Contact - KABADI Gregory S. :
gkabadi@ihi.or.tz
ABSTRACT Background Economic evaluations have significant roles in informing funding decisions. They provide the means to choose which programme of care to fund among the many competing for resources. Unlike in higher-income countries, published studies on economic evaluations of stroke in Sub-Saharan Africa are rare. Objective To pilot a method for estimating the cost of treating stroke in rural and urban Tanzania that will assist with future economic evaluations of stroke. Methods The pilot study was conducted as part of the Tanzania Stroke Incidence Study. Incident cases were reported by resident community informants. Cost data were summarised from project documents and data on out-of-pocket payments were collected by interviewing patients/carers. Productivity losses relating to post-stroke occupations were also estimated in monetary terms using standard monthly salary estimates by job category and gender. Results Sixteen incident cases (11 rural and 5 urban) were identified and followed-up for six monthsin 2005/2006. The overall mean cost per case was TZS 256,338 (USD 220) and included diagnostic tests (blood, ECG, echocardiogram, chest X-ray, CT scans), hospitalisation cost (registration, inpatient stay and drugs), transport cost to designated hospitals, physiotherapy and out-of-pocket payments to other points of care. Costs were more than four-fold higher in the urban district than in the rural district. Mean productivity loss per patient was TZS 247,930 (USD 213) and was more than double in the urban district than in the rural district. Conclusion This is the first published research investigating the cost of treating stroke in Tanzania. A bigger sample, long-term follow up and modeling are required for better estimates of stroke economic burden. Key words: Cost analysis, Stroke, Tanzania, Sub-Saharan Africa, Populations Rural/Urban BACKGROUND Stroke is a major public health problem in high-income countries and is a major contributor to mortality, disability and cost (Di Carlo). Available data suggest that stroke is an emerging problem in Sub-Saharan Africa (SSA) (Walker et al, 2000). Even though HIV/AIDS has been ranked the overall leading cause of death in SSA, cardiovascular disease, including stroke, ranks second and is the leading cause of mortality among those over the age of 45 (Lopez et al). Unlike in higher-income countries, where economic evaluations have contributed greatly to policymaking around stroke management, published studies suggest that very few countries in SSA have explored the cost of treating stroke in SSA (Guinhouya et al). Documented costs of treating stroke help governments to estimate the economic burden of the disease thereby aiding budgeting and planning for health care costs. Costs of treating stroke can be extremely high and sometimes unbearable for low-income families. These costs can either be direct or indirect; direct costs being healthcare costs related to prevention and treatment of stroke and its risk factors that involves individuals, governments, and the private sector. Indirect costs come in the form of lost productivity of working individuals as well as lost savings and assets that families forego to meet other healthcare expenditures such as stroke rehabilitation (Gaziano). In this pilot study, we sought to estimate the cost of treating stroke in one rural and one urban district of Tanzania. This will potentially provide a model for future economic evaluation studies on stroke in SSA. METHODS Recruitment and data collection This pilot study was conducted as part of the Tanzania Stroke Incidence Study (Walker et al, 2010). The main projectrecruited incident stroke cases in two demographic surveillance sites: rural Hai site with a population of 159,814 and urban Dar-es-Salaam (Dar) site with a population of 56,517. Stroke patients were identified by community key informants who were in contact with local hospitals: Kilimanjaro Christian Medical Centre (KCMC) for the Hai area and Muhimbili National Hospital for Dar area. None of the standard sampling procedures were performed to obtain the sample. The sample for this study included all recorded incident cases in the two districts from mid-June to mid-December 2005. All patients recorded during this period were followed up to monitor their status for six months (up to mid June 2006). Ethical clearance for the main study was received from the Tanzanian National Institute for Medical Research, and the Newcastle and North Tyneside Joint Ethics Committee, United Kingdom. 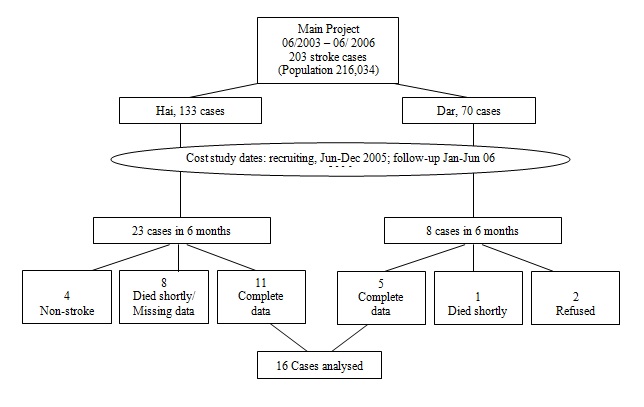 Figure 1 During the six-month period of data collection (June-December 2005), a total of 31stroke patients were recruited (23 from Hai and eight from Dar), (Figure 1). Of the 31 recruited, 16 patients, five from Dar and 11 from Hai had complete datasets on costs required for this analysis. Two patients refused to participate in the study, nine patients either died shortly after having a stroke before the relevant data could be collected or had a stroke during the data collection period but the information required for this study was not available. Four other patients were recruited but later found to have not had a stroke. Medical care costs Cost data were divided into two: costs paid by the project, and patients’ out-of-pocket (OOP) costs. For each stroke patient brought to hospital (admitted or not admitted) relevant data were recorded in the project’s central database. These included: laboratory tests and investigations including full blood picture, echocardiogram, electrocardiogram (ECG), Chest X-rays and Computed Tomography (CT) Head scan and, for those admitted, costs for inpatient care including length of stay and drugs. In addition, project staff recorded all transport expenses paid for patients to be brought back and forth to hospital and during their subsequent visits for further treatment of stroke-related conditions or while attending physiotherapy.Out of hospital settings, cost data (transport cost, upkeep cost and drug costs) were retrospectively collected through interviews with patients/carers at time of admission, at one month follow up and at six months follow up. Employed patients were also asked about any third-party payments such as private or public insurance schemes. All costs were expressed in current year Tanzania Shillings (TZS) in nominal values. Productivity losses The human-capital method was used to estimate the lost earnings due to stroke (Mattke et al, Brouwer et al, van den Hout). In order to value patients’ occupations in monetary terms, first patients’ pre-stroke occupations were recorded by asking patients/carers to state their main source of income over the 12 months prior to hospital admission and whether they spent most of their time on that particular source or on other occupations. Secondly, standard monthly salary estimates by job category and gender were obtained from the Tanzanian National Bureau of Statistics official website (Tanzania National Bureau of Statistics) for which the data were obtained from an Integrated Labour Force survey carried out in 2000/2001. Weights were used to incorporate inflation rates and changes in consumer prices using 2000/2001 estimates adjusted for the analysis year, 2005/2006. Consumer price indices were obtained from the Tanzanian National Bureau of Statistics official website on National Consumer Price Index.. RESULTS Patients Stroke treatment cost Currency is expressed in Tanzanian Shillings for year 2005/2006 (1 USD = TZS 1,162in 2005). Table 1 shows the different categories of costs incurred by patients or those paid by the main research project. The mean cost per patient in project-designated hospitals (registration, hospital stay and drugs) was more than twice as high in Dar (TZS 56,226) as in Hai (TZS 23,021). All patients were charged flat rate for CT-Scan and diagnostic charges (blood tests, ECG, Echocardiogram and chest X-ray), with Muhimbili (urban) hospital charging higher than KCMC hospital for CT-Scans and Echocardiograms. Table 1: Total cost (in TZS) at 6 months post-stroke, by category
Rehabilitation cost From stroke onset to six months follow up, the mean (median) physiotherapy cost per patient was TZS 80,965 (72,000), for Dar patients only. Physiotherapy cost for Dar patients contributed to about 15% of total cost of treating stroke. There was no cost recorded for physiotherapy services for Hai patients as patients had their physiotherapy done at home by their relatives, who had been taught about this in hospital. Transport cost The mean transport cost per patient from home to hospital in the Dar area was more than 10 times that in Hai (TZS 286,313 for Dar; TZS 25,752 for Hai). Patients’ out of pocket payment As Table 1 shows, the mean OOP cost for patients in both areas was similar (TZS 9,682 versus TZS 8,142 on drugs and home care, and TZS 7,144 versus TZS 7,246 on non-hospital transport costs for Dar and Hai respectively). Costs of traditional healers are included in the drugs and home care while travel expenses to traditional healers are included in the non-hospital transport cost category. Overall, the mean cost of treating a patient in Dar was more than four times higher than in Hai (Dar 547,240 versus Hai 124,111). The mean cost of treating a patient in the two areas combined was TZS 256,338. Lost productivity Table 2 shows the monetary estimate of productivity losses during the six-month period following stroke.The mean productivity loss per patient during the six-month period was more than twice in Dar patients compared to Hai patients (TZS159,616 for Hai, TZS 442,219 for Dar) with an overall mean loss of TZS 247,930 per patient. Table 2: Productivity losses (in TZS) at 6 months follow up
DISCUSSION To the best of our knowledge, this pilot study is the first attempt to report findings of the cost of treating stroke in Tanzania. In the six months following an incident stroke, the mean cost of treating stroke wasTZS 256,338 (about USD 220) and was more than four times higher in the urban district than that it was in the rural district (TZS 547,240/USD 471 for Dar patients compared to TZS 124,111/USD 107 for Hai patients).These costs excluded the cost of physiotherapy for Hai patients which were not available. We have also shown that the mean productivity loss in monetary terms per stroke patient during the six-month period of follow-up was more than double in the urban district compared to the rural district (TZS 442,219/USD 380 for Dar patients compared to TZS 159,616/USD 137 for Hai patients). Our pilot study had a small sample size and we did not collect other types of cost data. While the main project had recruited 203 community-based incident cases for three years, we only collected cost data from 16 cases within a period of six months. Treatment costs included diagnostic tests, hospitalisation cost (for Hai patients only), transport cost to the two designated hospitals, physiotherapy (for Dar patients only) and out-of-pocket payment (drugs, home care and travel cost to other points of care). Most of these costs were paid for by the main project. Patients (and their relatives) contributed only 6% of the total treatment cost and mainly towards seeking care before hospital admission. Nevertheless, our results suggest that even if cost data would have been collected from all 203 patients recruited by the main project, there would have been less notable variations in the average treatment cost as 94% of costs were paid for by the project and, given the results, there were no major overall differences in costs charged by the two hospitals the for project-paid items except for investigation costs. Major differences were only observed in patient-incurred cost which contributed to only about 6% of total cost. We did not collect capital costs and other operating costs such as doctor and nurse hours. It is likely that, subject to recall bias, urban patients (or their relatives) might have underreported cost estimates incurred before they were admitted to hospital. Diagnostic tests in Muhimbili hospital (urban district) were more expensive than in KCMC hospital (rural district). Patients in the urban district had prior appointments with the project’s physician before they were taken to the hospital for investigations. Due to these prior arrangements and close proximity to the hospital, none of the urban patients was admitted, thereby avoiding hospital stays and associated costs. Urban patients were on overall more likely to have first sought care from traditional healers before going to hospital due to beliefs that stroke was associated with ancestral spirits and witchcraft (Mshana et al). Our results are within the range of results reported by other studies in sub-Saharan Africa besides some slight variation in cost categories involved and the number of patients and duration of patient follow-up. For example, in 2006, a study in Congo Brazaville followed 90 stroke patients for over six months and found the mean cost per patient to be about Euros 240 (Gombet et al). Another study in Togo involved 412 patients in 2005 for one year and found that the mean hospitalization cost per patient was about Euros 680 (Guinhouya et al). In Senegal, a study in 1997 involving 383 stroke patients for one year reported the mean direct cost per patient to be about USD 157 (Toure et al). Also, a recent study in Nigeria involving 240 stroke patients found that the mean cost per patient ranged from USD 600 to USD 4,860 for accessing care within the first 36 weeks (over 8 months) following stroke (Birabi et al). Using the human capital approach, we report here the productivity losses from a patient’s perspective as an indirect cost of illness (in addition to direct treatment and management cost) being an indicative estimate of the economic burden of stroke. Other studies have included the employer’s perspective to value and report productivity losses using the friction method. However, there has been controversy on whether valuation of productivity losses should be included in estimating the economic burden due to an illness and in particular, the approach to use in estimating them (Schulpher). Some studies have argued that productivity losses are likely to be undervalued in the estimation process (Zhang et al, Krol et al). To some extent, this may be true in view of our data as most stroke patients did not have formal employment from which actual monetary losses could have been precisely estimated. It is also possible that actual productivity losses could have been underestimated due to recall bias and/or the difficulty in documenting and valuing all gainful activities patients were involved in before stroke. Absence from gainful work’ due to stroke also seems less applicable to patients who own residential houses they rented to tenants. Strengths and limitations of this study The main strength of the study was that it is the first of its kind in Tanzania to report the cost of treating stroke together with estimated productivity losses due to stroke. The study has shown the potential of conducting cost-of-illness studies due to stroke that can be part of economic evaluation studies in the country. Due to its nature, the study piloted a small sample of stroke patients and that it needed a relatively longer period (at least one year) of follow up for better estimates. CONCLUSION We therefore conclude that it is possible to identify, measure and track treatment cost as well as value in monetary terms productivity losses, for future estimation of the total cost of stroke in Tanzania. A bigger sample from both rural and urban districts, with a relatively longer follow up period (of at least one year) and modeling of results, would produce more accurate estimates. AUTHORSHIP GSK and CD conceived and designed the study, GSK collected data, analysed data and wrote the first draft of the article. RW was the principal investigator of the main project: Tanzania Stroke Incidence Study and obtained ethical clearance for the study; RW and CD prepared the grant application for the pilot study; PS supervised the research work. All authors interpreted the results, critically revised and approved the article for publication. ACKNOWLEDGMENTS We would like to thank all key informants, project staff, hospital clinicians and carers and family members for their involvement in entire work. Special thanks to Victor Mponzi and Mary Lewanga for their assistance in collecting data. CONFLICT OF INTEREST We have no conflicts of interest. FUNDING This pilot study work was funded by a grant from The Wellcome Trust (grant number 073150/Z/03/Z). REFERENCE
|
© 2002-2018 African Journal of Neurological Sciences.
All rights reserved. Terms of use.
Tous droits réservés. Termes d'Utilisation.
ISSN: 1992-2647