|
|
|
CASE REPORT / CAS CLINIQUE
WALLENBERG SYNDROME SECONDARY TO BILATERAL VERTEBRAL ARTERY DISSECTIONS AND THROMBOSIS.
SYNDROME DE WALLENBERG SECONDAIRE A UNE THROMBOSE ET UNE DISSECTION VERTEBRALE BILATERALE.
E-Mail Contact - ANAYO Komla Nyinèvi :
anayokomla2@gmail.com
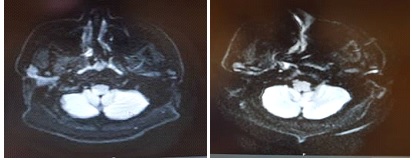
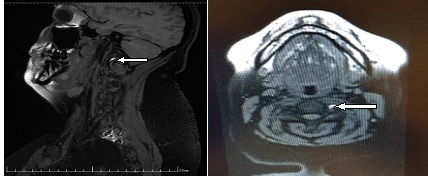
ABSTRACT The Wallenberg syndrome or lateral medullar syndrome (LMS) is also known as posterior inferior cerebellar artery syndrome. It’s a dangerous affection because of his gravity for vital prognostic by the paralysis of cranial nerves. Occlusion of these vessels may be due to stenosis from arteriosclerosis/emboli or arterial dissection. The artery dissection may be spontaneous or after trauma is an important and often treatable cause of the stroke in younger people. The Magnetic Resonance Imagine diffusion weighted inversion (MRI-DWI), the Magnetic Resonance Angiography (MRA) sequence FAT/SAT and the computed tomography (CT) angiography of the brain allow quickly to the diagnosis. The antithrombotic treatment (antiplatelet drug) and low-molecular weight heparins allow to reduce the neurological sequelea. So we report two cases of Wallenberg’s syndrome caused by spontaneous bilateral vertebral dissection and vertebral thrombosis and their clinical, prognostic and therapeutic aspects. A 34-years-old woman, no cardiopathy factors only obesity, no trauma, admitted for acute vomiting, vertigo, neck pain and weakness earlier in themorning and MRA FAT/SAT showedbilateral vertebral artery dissections without an evident posterolateral medulla infarct on MRI-DWI. A 48-year-old man, cumulated cardiopathy factors risks, admitted with sudden vertigo, disequilibrium and neck pain. The MRI-DWI showed an acute left posterolateral medulla infarct and the CT angiography revealed thesevere left vertebral artery thrombosis. They were treated by the antithrombotic drugs (antiplatelet drugs) and low-molecular weight heparins. In front of a sudden neck pain and vertigo, think about Wallenberg’s syndrome and do quickly an imaging. Key words: Antithrombotic, artery, dissection, thrombosis, Wallenberg, MRI. Mots clés : Antithrombotique, artère, dissection, thrombose, Wallenberg, IRM. INTRODUCTION Wallenberg syndrome or Lateral medullary syndrome (LMS) is also known as posterior inferior cerebellar artery syndrome. It results an occlusion of posterior inferior cerebellar artery (PICA) or the vertebral artery. Occlusion of these vessels may be due to stenosis from arteriosclerosis/emboli or arterial dissection [5]. This affection is dangerous because of his frequency as a cause of stroke and his gravity for vital prognostic [4]. Approximately 10% of strokes occur in patients <50 years of age [13]. The vertebral artery dissection (VAD) is a common and important cause of stroke in younger people, but, often treatable [7]. The Wallenberg syndrome manifests as various degrees of cerebellar dysfunction in relation of location of the lesions [15]. So we report here two cases of Wallenberg syndrome caused by spontaneous bilateral vertebral artery dissections and vertebral thrombosis. A 34 years-old woman, admitted for sudden posterior headache, vomiting, vertigo, weakness and left-side body paresthesia when she was wake-up to toilet in the night. The magnetic resonance angiography (MRA) FAT/SAT revealed the bilateral vertebral dissections without an evident posterolateral medulla infarct on brain magnetic resonance imaging diffusion weighted inversion (MRI-DWI). A 48 years-old man, admitted for sudden dizziness and vertigo, left facial paresthesia and posterior headache in morning at six o clock. The MRI-DWI showed an acute left posterolateral medulla infarct and the CT angiography revealed a severe left vertebral thrombosis. We describe clinical, etiological and therapeutic aspects and review of the literature. Case report 1 A 34-year-old woman without medical history of cardiopathy, admitted in our hospital with sudden dizziness and tendency to fall without loss of consciousness during the attack while she was going to toilet earlier the morning, vertigo, vomiting and left-side body paresthesia, right facial loss sensitivity associated with severe right neck pain without veritable trauma. Her physical examination showed general weakness with anxiety, normal blood pressure (blood pressure : 130/80 mmhg), no loss of consciousness with Glasgow coma scale (GCS) at 15,obesity (body mass index at 34.52kg/m²), incomplete right Claude Bernard Horner syndrome, rotatory and horizontal nystagmus, right facial sensory deficit, left thalamic syndrome with left body paresthesia. The National Institutes of Health Stroke Scale (NIHSS) was 2. The brain MRI-DWI showed no evident lateral medulla infarct (figure 1A). Axial and sagittal MRA sequence FAT/SAT showed a bilateral vertebral artery anomalies (left V2 side and right V3-V4 vertebral dissections) (figure 1B, figure 1C). Electrocardiogram (ECG) was normal, and blood test showed LDL-cholesterol elevated (1.22 g/l). She was treated with preventive low-molecular weight heparin associated with antiplatelet drug, statin, paracetamol and addressed for neurological reeducation. She continued with aspirin. On follow-up examination after three months ago, her symptoms had resolved but it had persisted left body paresthesia and middle right loss sensitivity. Case report 2 A 48-year-old, medical history of hypertension, cerebellar stroke in 2015, monocular diplopia and hyperlipidemia treated with perindopril, kardegic and statin, admitted in hospital two days after the symptoms with the sudden sense of disequilibrium, posterior and frontal headache, left facial paresthesia, dysphonia, dysphagia and right-side body paresthesia. His physical examination revealed anxiety, weight gains (body mass index at 27.6kg/m²), his blood pressure was 178/95 mmhg, no loss of consciousness (GCS 15), left Claude Bernard Horner syndrome,left lateralized Romberg, left cerebellar ataxia, hiccup or hoquet and right-side body paresthesia and sequelea monocular diplopia. His NIHSS was 3. The Magnetic resonance imaging (MRI-DWI) showed an acute infarction in the left posterolateral medulla may be due to the thrombosis and explained the symptoms (figure 2A) and computed tomography (CT) angiography revealed left vertebral thrombosis (figure 2B). His ECG showed an ischemia and his blood test was normal only the hyperlipidemia. He was put on curative lovenox therapy for three days and continued with double antiplatelet drugs for three months, statin, perindopril and paracetamol drugs and addressed for neurological reeducation. In control after three months, it persisted low dysphonia and mile left facial paresthesia, his continued with only clopidogrel as antithrombotic treatment. The following figure showed the bilateral vertebral artery dissections on MRA FAT/SAT and no evident lateral medulla infarction MRI-DWI.  Figure 1B: MRA (sagittal and axial) FAT/SAT revealed the third and fourth (V3- V4) right vertebral artery dissection.
The following figures showed the left vertebral thrombosis andan acute infarction in the left posterolateral medulla in our case report 2. 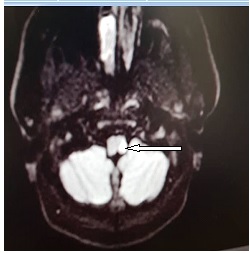 Figure 2A: Magnetic resonance imaging (MRI-DWI) showed an acute infarction in the left posterolateral medulla may be due to the thrombosis  Figure 2B: Computed tomography (CT) scan angiography of brain proved the severe left vertebral artery thrombosis.
DISCUSSION Wallenberg syndrome or lateral medullar syndrome (LMS) occurs after occlusion of the vertebral artery or its branches such us the posterior inferior cerebellar artery (PICA). Generally, the LMS happens to the patients who have much comorbidity such hypertension, hypercholesterolemia, diabetes and arteriosclerosis. But in our case report 1, the patient has any comorbidity like reported in some papers [5, 12]. Clinically, we observed typical Wallenberg syndrome in our two cases reports. We observed the Horner’s syndrome, nystagmus, dysphonia, body paresthesia, facial loss sensibility, dysphagia, vomiting, and nausea. All these symptoms are described in the literature in various situations [9, 8]. The authors recognized that the symptoms help to locate the damaged region. However, all of symptoms are not present to the same patient like our patient in case report 1 from whom we hadn’t a dysphasia. We can explain this absence of some symptoms by the absence of an evident infarction in lateral medullary territory because the severe dysphagia is probably based on impaired swallowing reflex related to sensory dysfunction [3]. In our case report 1, the patient has an incomplete Claude Bernard-Horner syndrome probably due to the suffering of neuron cells only in posterolateral medullar area because of the absence of the infarction. The spontaneous bilateral vertebral dissection was the cause of LMS in our case report 1. Similarcases weredescribed in the literature confirmed that the VAD is the cause of stroke in young people [4, 5]. It is spontaneous vertebral disease because our patient of 34-year-old has no trauma history. Chang BS and al reported the same case [4]. But in our observation, the MRI FAT/SAT showed the bilateral vertebral dissections no trauma context. So it is difficult to be sure that there is no trauma, because it can be the minor trauma like hyperextension of the neck when she was raised to the bed. This hyperextension of her neck could be the cause of the dissection in our case 1 andreported in the literature in the minor trauma situation [5]. Many papers reported that the vertebral artery dissection without preceding trauma history is quite rare in young ischemic stroke patient [16]. And the authors to agree that in young adult, the most common etiology of acute ischemic brain infarction are arterial dissections and cardiogenic embolic stroke [5, 16]. Our patient presented the symptomatic LMS but we have no evident infarctionin the lateral medullary area in MRI-DWI. That ranges from asymptomaticocclusions, transient ischemic attacks to lateral medullary syndromes as reported in the literature with normal MRI-DWI [11]. Our patient was treated with preventive low-molecular weight heparins (Lovenox) associate with antiplatelet drug like aspirin. But some authors used curative heparin drug administration immediately in the process of hospitalization because of the dissection and after seven days from the debut, the patient was transitioned to acenocumarol for long-term anticoagulation until getting the INR therapeutic in the 2-3 intervals [6] or to warfarin [4]. Our patient was put on to warfarin. The patient was not put on acurative heparin because of risk of subarachnoid hemorrhage due to the site of vessel injury as reported in the literature [14]. Although, some authors used intravenous thrombolysis in the four past half hours to the beginning of the symptoms when there is a mismatch diffusion-Flair [14]. However, our patient had not benefited the thrombolysis treatmentbecause firstly due to the unavailability of this treatment in our medical practice and secondary, our patient has no evident posterolateral medulla infarct in MRI-DWI which justifies the intra-venousthrombolysis. Our patient hadn’t severe sequelea probably due to the absence of infarction in posterior territory contrary to some papers which reported that the dissection of the vertebral artery associated with multiple infarcts in the posterior territory had a bad prognosis [2]. In the control three months ago, the symptoms were resolved, only persisting mild paresthesia in right facial. The vertebral thrombosis was perhaps the cause of Wallenberg’s syndrome in our case report 2. This vertebral thrombosis was revealed by CT angiography. But our patient in this case report 2 had others cardiovascular diseasesuch hypertension, dyslipidemia and medical history of stroke. Therefore, it was difficult to know exactly that the thrombosis was the veritable cause. According to Marchand L and al, the vertebral thrombosis as a cause of LMS is rare [12]. It may be the association of causes that lead to lateral medulla infarct observed in MRI-DWI. Most authors were agreed that the unilateral or bilateral vertebral dissection may be spontaneous or after neck trauma was the veritable and important cause of lateral medulla infarct [5, 9]. The monocular diplopia observed in this case was the sequelea of ophthalmologic pathology in the past not due to the recent lesion. In our case report 2, our patient had a severe dysphagia most likely to the presence of lesion on lateral medulla area contrary to the patient of case report 1 from whom we found no infarct. This severe dysphagia can be explained by the paralysis of glossopharyngeal nerve. He presented also a severe dizziness, so severe that he could not walk or stand-up. He was obliged to be always on bed. We observed a severe left Claude Bernard-Horner syndrome. This signs correlated well with cervical sympathetic paralysis caused by the lesion as reported on most papers [17, 1]. The nausea, vomiting can be explained by the damage of nervous system in this area of brain especially the paralysis of glossopharyngeal, vague and hypoglossal nerves. Our patient was treated by curative low-molecular weight heparins (lovenox) four three days and had been put on to double antiplatelet drugs. He was put on curative lovenox because of his medical history of heart disease and high cardiovascular factors. He was put under dual antithrombotic drugs (antiplatelet) because he was in monotherapy antiplatelet (kardegic) before having this recent vascular problem. Concerning the dysphagia, we placed nasogastric tube and continued the orthophonic reeducation even if Kattah C and al proposed the percutaneous gastrostomy [10]. Percutaneous gastrostomy was not veritably indicated in our context because our patient’s dysphagia was revolved with orthophonic reeducation. Concerning dysphasia, Yuichiroand al, Amber E and al proposed the use of pyridostgmine to treat the severe dysphagia in LMS [17, 1]. In control-examination three months ago, our patient dysphagia and dizziness were resolved but it persisted mild disequilibrium. The prognosis of our patient is not severe, possibly due to the detection of only one lesion of infarct in lateral medullary area, as opposed to multiples infarcts with a bad prognosis as reported by Bemasconi A and al [2]. CONCLUSION Wallenberg syndrome or lateral medullary syndrome (LMS) is serious affection because of his vital prognosis. So many causes are incriminated such as vertebral dissection and vertebral arteriosclerosis. Vertebral dissection may be spontaneous or neck trauma is an important, and often treatable, cause of ischemic stroke in young adults. The clinical symptoms are various including vertigo, equilibrium disturbance, neck pain, vomiting and Horner syndrome. It is important to think about LMS the in front of Claude Bernard-Horner syndrome and perform quickly an imaging especially magnetic resonance angiography sequence FAT/SAT. Conflicts of Interest: The authors have no conflicts of interest to declare. REFERENCES
|
© 2002-2018 African Journal of Neurological Sciences.
All rights reserved. Terms of use.
Tous droits réservés. Termes d'Utilisation.
ISSN: 1992-2647