
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
ORIGINAL PAPERS / ARTICLES ORIGINAUX
DEFINITIVE SARS-COV-2 INFECTION & COVID 19 VACCINATION IN MOVEMENT DISORDER PATIENTS: EXPERIENCE FROM A TERTIARY CARE CENTER IN ETHIOPIA
INFECTION DÉFINITIVE PAR LE SARS-COV-2 ET VACCINATION CONTRE LA COVID-19 CHEZ LES PATIENTS ATTEINTS DE TROUBLES DU MOUVEMENT : EXPÉRIENCE D'UN CENTRE DE SOINS TERTIAIRES EN ÉTHIOPIE
E-Mail Contact - AMOGNE Wondwossen :
wonamogne@yahoo.com
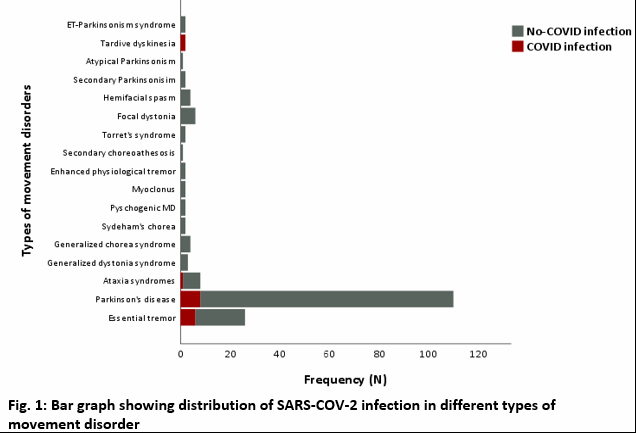
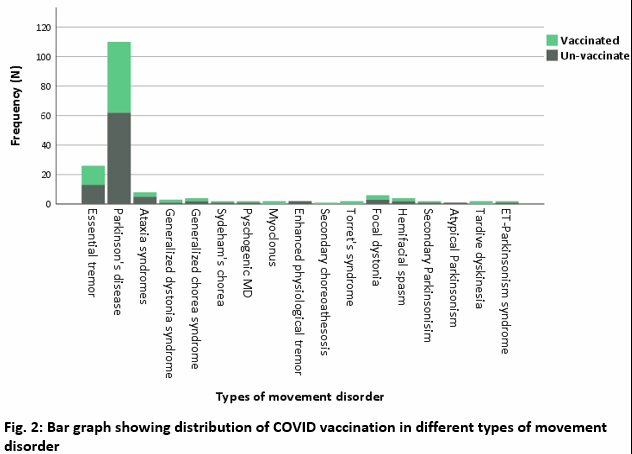
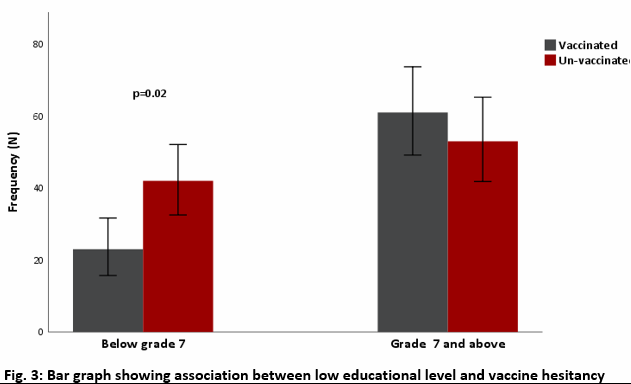
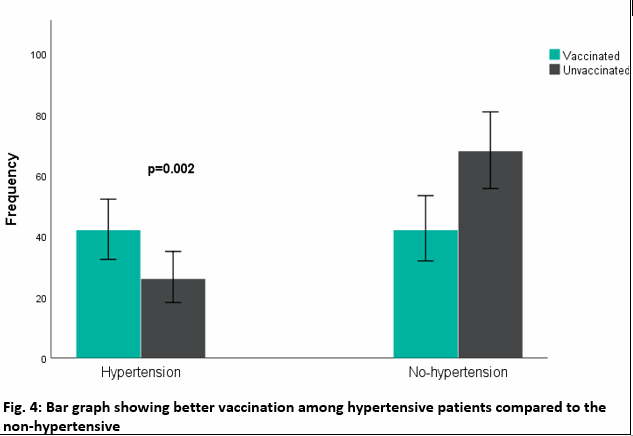
ABSTRACT Background: The magnitude of the SARS-COV-2 pandemic and COVID 19 vaccine uptake in patients with neurological disorders such as movement disorders (MD) such as Parkinson’s disease (PD) is largely unknown in Ethiopia. There is urgency in understanding the burden of COVID-19 infection and vaccination uptake and associated factors in African patients with MD. Method: An observational cross-sectional facility-based study was conducted at Tikur Anbessa Specialized Hospital (TASH) in Addis Ababa, Ethiopia. Convenient sampling technique was used, and the study was conducted between March 01, 2022, and April 30, 2022. Both descriptive and inferential statistics were used. Results: A total of 179 patients with movement disorders were included for the analysis. The median age was 62 (IQR 50 – 70) years. Males accounted for 62.6%. The median duration of illness was 5 (IQR 2 – 10) years. The commonest MD was Parkinson’s disease (61.4%) followed by essential tremor, ataxia syndromes, and dystonia syndromes respectively. Hypertension was the most common comorbid disorder, followed by other comorbid neurological disorders and type diabetes mellitus. Five (2.8%) patients have HIV infection. The point prevalence of definitive SARS-COV-2 infection was 9.5% (n=17/179). COVID 19 vaccine intake was 46.9%. Hyperkinetic MD was associated with COVID-19 infection when adjusted for age, gender, economic status, and duration of MD diagnosis (AOR 3.53 95% CI 1.14 – 10.87 p=0.03). Comorbid hypertension was positively associated with COVID vaccination (AOR 2.04 95% CI 1.01 – 14.13 p=0.04). Lower educational status was associated with COVID vaccine hesitancy (COR 0.48 95% CI 0.25 – 0.89 p=0.02). Conclusion: The present study shows high burden of definitive SARS-COV-2 infection and low COVID vaccine uptake in movement disorders patients attending TASH. Hyperkinetic MD was associated SARS-COV-2 infection. Lower educational level was independent predictor of low vaccine uptake. Keywords: Movement disorders; Parkinson’s disease; SARS-COV-2; COVID 19 vaccine; Vaccine hesitancy; Ethiopia RÉSUMÉ Contexte: L’ampleur de la pandémie de SARS-COV-2 et l’adoption du vaccin COVID-19 chez les patients atteints de troubles neurologiques tels que les troubles du mouvement (MD), tels que la maladie de Parkinson (PD), sont largement inconnues en Éthiopie. Il est urgent de comprendre le fardeau de l’infection à la COVID-19 et l’adoption du vaccin, ainsi que les facteurs associés chez les patients africains atteints de MD. Méthode: Une étude observationnelle transversale basée sur les installations a été menée à l’hôpital spécialisé Tikur Anbessa (TASH) à Addis-Abeba, en Éthiopie. Une technique d’échantillonnage pratique a été utilisée, et l’étude a été menée entre le 1er mars 2022 et le 30 avril 2022. Des statistiques descriptives et inférentielles ont été utilisées. Résultats: Au total, 179 patients atteints de troubles du mouvement ont été inclus dans l’analyse. L’âge médian était de 62 ans (IQR 50 – 70). Les hommes représentaient 62,6%. La durée médiane de la maladie était de 5 ans (IQR 2 – 10). Le MD le plus courant était la maladie de Parkinson (61,4%), suivie par le tremblement essentiel, les syndromes d’ataxie et les syndromes dystoniques respectivement. L’hypertension était le trouble comorbide le plus courant, suivi d’autres troubles neurologiques comorbides et du diabète de type. Cinq (2,8%) patients étaient infectés par le VIH. La prévalence ponctuelle de l’infection définitive par le SARS-COV-2 était de 9,5% (n = 17/179). La prise du vaccin COVID-19 était de 46,9%. Le MD hyperkinétique était associé à l’infection à la COVID-19 après ajustement pour l’âge, le sexe, la situation économique et la durée du diagnostic du MD (RA 3,53 IC à 95% 1,14 – 10,87 p = 0,03). L’hypertension comorbide était positivement associée à la vaccination COVID (RA 2,04 IC à 95% 1,01 – 14,13 p = 0,04). Un niveau d’éducation plus bas était associé à l’hésitation à se faire vacciner contre la COVID (COR 0,48 IC à 95% 0,25 – 0,89 p = 0,02). Conclusion: La présente étude montre une forte charge d’infection définitive par le SARS-COV-2 et une faible adoption du vaccin COVID chez les patients atteints de troubles du mouvement fréquentant le TASH. Le MD hyperkinétique était associé à l’infection par le SARS-COV-2. Un niveau d’éducation plus bas était un prédicteur indépendant d’une faible adoption du vaccin. Mots-clés: Troubles du mouvement ; Maladie de Parkinson ; SARS-COV-2 ; Vaccin COVID-19 ; Hésitation vaccinale ; Éthiopie INTRODUCTION In Ethiopia, as of this writing (23 May 2022), there have been 471,227 confirmed cases of SARS-COV-2 infection and 7,512 deaths [1] Likewise, a total of 29,373,478 vaccine doses have been administered, 24,769,870 persons vaccinated with at least one dose, and 21,291,403 persons were fully vaccinated [1]. Patients with movement disorders, especially individuals diagnosed with Parkinson’s disease (PD) are at higher risk of SARS-COV-2 infection. A recently published meta-analysis by Reza et al. 2022 [2], showed the pooled prevalence of COVID-19 infection in PD patients to be 5% with 49% hospitalization and 12% mortality. The authors reviewed total of thirty articles where majority of the studies were from United State of America (USA). Furthermore, the prevalence of COVID- 19 infection in PD cases from all included studies ranged between 1 and 43% [2]. SARS-CoV-2 infects the host cells using angiotensin-converting enzyme 2 (ACE2) receptors on the cellular surface; which is highly expressed in respiratory epithelial cells and also dopaminergic neurons in the basal ganglia [3–6]. On the other hand, brain angiotensin system has role in neurodegeneration in PD cases. All of these findings could show that PD patients are at higher risk of catching SARS-Co V-2 infection [3,4,6]. However, there is a great paucity of scientific evidence on SARS-COV-2 infection and COVID 19 vaccine uptake in patients with neurological disorders in Africa. Katoto et al 2022 recently reported on the predictors of COVID 19 vaccine hesitancy in South African population [7]. According to the authors, the following modifiable factors were associated with vaccine hesitancy: concerns about side effects, lack of access to the online vaccine registration platform, distrust of government, belief in conspiracy theories, having no monthly income, and depending on someone else to make vaccination decision [7]. In patients with neurological disorders COVID 19 vaccine uptake will be likely influenced by the vaccine adverse effect, which may worsen the underlying neurological disorders and withholding medications such as antiepileptic medications (AEDs) in fear of avoiding drug vaccine interaction [8]. For this reason, there is an urgency to investigate the magnitude of SARS-COV-2 infection and COVID vaccination uptake in African patients with movement disorders. METHODS AND MATERIALS Study setting and period The study was conducted at a movement disorder clinic at Tikur Anbessa Specialized Hospital (TASH), a tertiary level university hospital located in Addis Ababa, Ethiopia. The hospital hosts the only neurology department in Ethiopia. The movement disorder clinic at TASH runs on a once weekly schedule on Tuesday morning. On average weekly 15 – 20 patients with movement disorder are evaluated at the clinic. The movement disorder clinic mainly serves patients from Addis Ababa and the surrounding sub-urban area and some referrals from regional hospitals. We have included all consented consecutive patients with movement disorder attending the specialty clinic between March 01, 2022, and April 30, 2022. Study design and sample size This is an observational cross-sectional facility-based study using a convenience sampling technique. Data collection and case ascertainment procedure Data collection was conducted by board certified neurologists. All movement disorder case ascertainment was primarily done by consultant neurologists assigned to the movement disorder clinic. The data were collected using a structured questionnaires prepared for this study. The questionnaire has four sections: 1) demographic and social information; 2) clinical information; 3) SARS-COV-2 infection related data; and 4) COVID 19 vaccination related information. Statistical analysis Demographic data and clinical characteristics were first described by their range, means, and standard deviation. Association between outcome variable and different clinical characteristics were done using chi square and crude odds ratio (OR) with 95% CI. The strength of association was presented using adjusted odds ratio with 95% CI and P-value < 0.05 was considered as statistically significant. RESULTS Baseline characteristics of the study participants In the present study, a total of 179 patients with movement disorders were included in the analysis. The median age was 62 (IQR 50 – 70) years. Males accounted for 62.6% (n=112). The median duration of illness was 5 (IQR 2 – 10) years. Sixty-five (36.3%) attended grade 7 and below. Fifty-four (30.2%) were unemployed and 41.3% of the patients earn less than 1000 Ethiopian birr monthly. Out of 179 participants, 65.4% were married (Table 1). Diagnoses captured included idiopathic Parkinson’s disease (61.4%) followed by essential tremor, ataxia syndromes, and dystonia syndromes respectively (Fig. 1). Hypertension was the commonest comorbid disorder (38%), followed other neurological disorders (18.4%) and diabetes mellitus (15.1%). Five (2.8%) study participants have HIV infection and eleven (7.8%) have comorbid psychiatric disorders (Table 1). SARS-COV-2 infection in individuals with movement disorders In the present study, out of the 179 patients, the total number of patients tested for COVID 19 was not known. Only individuals with confirmed COVID infection by nasopharyngeal PCR test were included. Likewise, definitive SARS-COV-2 infection occurred in 9.5% (n=17/179). The proportion of COVID-19 infection was higher among male patients with movement disorders compared to their female counterparts (8.4% vs. 1.1% p=0.02). Married individuals (p=0.02) and those who have attended above grade 7 (p=0.006) had higher proportion of SARS-COV-2 infection compared to single/ and divorced and those who have attended below grade 7 respectively. Similarly, individuals who have earned above 1000 Ethiopian birr (ETB) monthly were found to have higher proportion of COVID 19 infection compared to those earned below 1000 ETB (8.9% vs. 0.1% p=0.001) (Table 2). Even though statistically not significant, a positive trend of COVID 19 infection and hyperkinetic movement disorders, and the presences of hypertension. Furthermore, no association was found between SARS-COV-2 infection and occupational status, and presences of diabetes mellitus and cardiac illness (Table 2). No difference in the mean age was observed in patients with hypokinetic movement regarding SARS-CVO-2 infection (Fig. Supp.1) COVID 19 vaccination in individuals with movement disorders In the present study, out of 179 individuals, ninety-five (53.1%) were not vaccinated. Of eighty-four (46.9%) individuals who had received at least one or more doses of COVID 19 vaccine, more than two-third received AstraZeneca vaccine, while the rest (23.8%) reported receiving Johnson and Johnson (J & J) (Table 1). More than half of patients diagnosed with Parkinson’s disease and essential tremor have received at least one dose of COVID 19 vaccine (Fig. 2). Significant COVID 19 hesitancy was observed among individuals earning below 1000 ETB (p=0.04) (Fig. Supp. 3) and those who have attended below grade 7 (p=0.02) (Fig. 3). Comorbid hypertension was positively associated with COVID vaccination (AOR 2.04 95% CI 1.01 – 14.13 p=0.04). Lower educational status was associated with COVID vaccine hesitancy (COR 0.48 95% CI 0.25 – 0.89 p=0.02) (Table 4). Logistics regression analysis between SARS-COV-2 infection and covariates In the present survey, COVID 19 infection was associated with hyperkinetic movement disorders when adjusted for age, gender, educational status, monthly income, and duration of MD diagnosis (AOR 3.53, 95% CI 1.14 – 10.87, p=0.03) (Table 3). Nearly significant association was found between earning above 1000 ETB and SARS-COV-2 infection when adjusted other covariates (AOR 0.14, 95% CI 0.02 – 1.34, p=0.08). In univariate regression analysis male gender was associated with COVID 19 infection (COR 5.02, 95% CI 1.11 – 22.17, p=0.04), however, no association was observed when adjusted for the other covariates. In this study, no association was observed between COVID 19 infection and age category, educational level, and duration of MD diagnosis (Table 3). DISCUSSION Even though our cohort includes all patients with movement disorders (MD) including hyper and hypokinetic, majority of them are PD patients. Individuals diagnosed with hyperkinetic MD, being male, married individuals, and those who have attended grade 7 and above have higher prevalence of SARS-COV-2 infection. In this study, high COVID 19 vaccine hesitancy was observed. Vaccine hesitancy was associated with attending grade 7 and below and lower monthly earning. Patients with movement disorder, especially those with PD are at higher risk of acquiring COVID 19 infection; this is because most are elderly individuals with multiple comorbid disorders [2,9–12]. In the present survey, the prevalence of confirmed SARS-COV-2 infection was higher than reports from western countries and meta-analysis which predominantly includes western data [3,9,12,13]. According to Del Prete et al. 2021[9], out of 740 PD patients interviewed, only 0.9% were found to be infected with COVID-19. Similarly, Khoshnood et al. 2022, reported the pooled prevalence of COVID-19 infection in PD cases was 5% [3]. Despite absence of similar studies in Africa for comparison, we have speculated that the present magnitude of COVID 19 infection among our patients could be grossly underestimated, as we have only included those with definitive COVID 19 infections. Contrary to our results, report from the King’s center, which has 4000 PD patients in the catchment, the prevalence of COVID 19 infection was 0.002% [14]. Furthermore, the overall low COVID 19 testing in Africa, particularly in Ethiopia may also support our speculation. Considering patients with MD, particularly patients diagnosed with Parkinson’s disease are at highest risk of COVID infection, it is vital to adopt a proactive outpatient’s service including routine screening for SARS-COV-2 infection. In the present study, the commonest comorbid diseases include hypertension, other neurological disorders, and diabetes. This is in congruent with previously reported study from Italy, indicating hypertension and diabetes mellitus as the commonest risk factors of SARS-COV-2 infection in PD patients [9]. This indicates those well-known and studied COVID 19 risk factors at the population level are still relevant to patients with movement disorders. In this study, the proportion of the SARS-COV-2 infection was higher in males, those who are married, in those diagnosed with hyperkinetic MD, individuals who have attended grade 7 and above. This is likely because, in most society male is the bread winner and should keep working even during pandemic period, further increasing the risk of getting infection compared to those individuals stayed at home. Likewise, married individuals tends to live with multiple family members, spouse and children, which may contribute for their increased risk of acquiring infection. These results were consistent with the study from the Kings’ center, out of the total 8 PD patients infected with SARS-COV-2, 6 were men, all are in their 6th decades with advanced diseases stage, and having comorbidities [14]. In this survey, individuals with hypokinetic MD had slightly lower burden of COVID 19 infection compared to those patients diagnosed with hyperkinetic MD. This is likely because, at the beginning of the pandemic all patients with hypokinetic MD, especially PD who were followed at our MD clinic were advised to stay home and the neurological care was shifted to teleneurology via phone clinics [11,15]. This could have contributed to the lower burden of confirmed SARS-COV-2 infection observed in individuals diagnosed with hypokinetic MD. In the present survey, less than half of the patients diagnosed with movement disorders have received one or more doses of COVID vaccine. Majority of the patients received AstraZeneca vaccine, while the rest received J & J vaccine; this shows low COVID vaccination status of the most vulnerable elderly patients with comorbidities. Lower vaccine uptake was observed in the present cohort which is incongruent with the overall high burden of vaccine hesitancy reported in Africa [16–20]. In Africa, vaccine hesitancy is due to multifactorial causes: firstly, the lack of knowledge on the importance of vaccines in reducing mortality and morbidities associated with communicable diseases; secondly, vaccine hesitancy could be rooted to the history of colonial medical and vaccine research abuse in Africa, which significantly pare the public confidence in the existing health care system [17,18]. Furthermore, in Africa the public trust for COVID 19 vaccine was further plummet by sentiments expressed by some scientists in the western countries (eg, by two French doctors in early April, 2020—with regard to conducting COVID-19 vaccine trials in Africa) [18]. In the present survey, COVID vaccine uptake was associated with low socioeconomic. This is consistent with a recent study by Katoto et al 2022, who reported the following predictors of COVID 19 vaccine hesitancy: concerns about side effects, lack of access to the online vaccine registration platform, distrust of government, belief in conspiracy theories, having no monthly income, and depending on someone else to make vaccination decision [7]. This is likely explained by the general lack of trust and vaccine related misinformation among those economically disadvantaged community [17–20]. Contrary to this, we found a positive relationship between COVID 19 vaccine acceptance and the presences of comorbid hypertension and diabetes mellitus. Yilma et al. 2022, assessed the COVID 19 vaccine acceptance in health care workers (HCWs) in Ethiopia and found out, about 25.5% of the HCWs would not accept a COVID- 19 vaccine and 20.2% were not willing to recommend COVID- 19 vaccination to others. Female gender, negative perception of vaccine, and perception about the SARS-COV-2 infections were predictors of vaccine hesitancy among HCWs in Ethiopia [16]. The present results mandate, a coordinated and structured COVID 19 vaccine advocacy works to counter the high magnitude of COVID 19 vaccine hesitancy observed in our patients, to keep the pandemic under control and to prevent future waves and viral mutations. The limitation of our study includes small sample size from a single facility, lack of control group, limited information regarding the number of total tested individuals, and absence of data regarding the COVID 19 variants. Other caveat of this study was, due to lack of fund we failed to investigate our patients for evidence of past COVID infection using SARS-COV-2 antibodies using bleed tests. We would have a more accurate burden of COVID 19 infection in our patients. CONCLUSION The present study shows high burden of definitive SARS-COV-2 infection and low COVID vaccine uptake in movement disorders patients attending TASH. Hyperkinetic MD was associated SARS-COV-2 infection. Lower educational level was independent predictor of low vaccine uptake. We recommend conducting a future controlled prospective study to cement our findings. Acknowledgements: We are thankful to Parkinson Patient Support Organization Ethiopia (PPSO-E) for the financial support to cover the data collection and stationary costs. We are grateful to our patients who have agreed to take part in this survey. Abbreviations: ETB: Ethiopian birr; J & J: Johnson & Johnson; PD: Parkinson’s disease MD: Movement disorders; LMIC: Low- and middle-income countries TASH: Tikur Anbessa Specialized Hospital; USA: United States of America Declarations Ethical approval of the study protocol The study received ethical approval from Addis Ababa University, College of Health Science Ethical Clearance Committee (Protocol number: 117/19/Neuro) Availability of data and materials: All data sets on which the conclusions of this manuscript rely are available as spread excel sheet document and available from the corresponding author on reasonable request. Funding: None Conflict of interest: All the authors have declared no conflict of interest. Consent to publication: Not applicable Table 1: Characteristics of movement disorder patients attending TASH (n=179)
*I Table 2: Factors associated with SARS-COV-2 infection in individuals with movement disorder
Table 3: Logistics regression analysis between SARS-COV-2 infection and covariates
Table 4: Logistics regression analysis of COVID 19 vaccination and covariates
    REFERENCES
|
© 2002-2018 African Journal of Neurological Sciences.
All rights reserved. Terms of use.
Tous droits réservés. Termes d'Utilisation.
ISSN: 1992-2647