
|
|
|
ORIGINAL PAPERS / ARTICLES ORIGINAUX
INTRAOPERATIVE USE OF THE MICRO-DOPPLER PROBE IN INTRA CRANIAL ANEURYSM SURGERY : IS THERE ANY IMPACT ON TREATMENT RESULT?
UTILISATION PRE-OPERATOIRE DE LA SONDE MICRO-DOPPLER DANS LA CHIRURGIE DES ANEVRISMES INTRACRANIENS : QUEL IMPACT SUR LE RESULTAT DU TRAITEMENT !
E-Mail Contact - THIOUB Mbaye :
thioubmbaye@gmail.com
ABSTRACT Context and objective: Intracranial aneurysm surgery can lead to clip-related complications. The use of intraoperative monitoring tools can help to limit complications and therefore the morbidity of the procedure. In this study, we analyse the impact of the intraoperative use of microvascular Doppler on the results of intracranial aneurysm surgery, and more specifically on the functional outcome of patients. Methods: A 7-year retrospective study from January 2013 to December 2019 was conducted in neurosurgery department of Fann National Hospital in Dakar, Senegal. We included all patients operated for exclusion of an intracranial aneurysm during this period. These patients were divided into two groups on the basis of intraoperative use of microvascular Doppler; and their evolutionary parameters were the subject of a comparative study. Results: Our cohort included 266 patients with 287 aneurysms; the mean age of the patients was 46 and the sex ratio was 2.20. Of all the patients, 27% had a Doppler check at the time of exclusion of their aneurysm and the remaining 73% were operated on without this technique. In the group of patients operated on without Doppler we noted 23.4% new deficits and 12% post-operative ischaemia; 11% deaths and 7.3% poor mRS at one month follow-up. In patients operated on under Doppler control, we noted 28.4% new deficits, 14.8% post-operative ischaemia, 12.3% death and 2.7% poor mRS at one month follow-up. Conclusion: The use of microvascular Doppler during aneurysm surgery does not reduce patient mortality but significantly improves quality of life, with a better Rankin score at one month. Keywords: Intracranial aneurysm, microdoppler, clipping, intraoperative.
RESUME Context et objectif : Le traitement des anévrysmes intracrâniens peut induire des complications liées à la pose du clip. L’utilisation d’outils de contrôle peropératoire peut permettre de limiter les complications ; et par conséquent la morbidité du geste. Nous analysons dans cette étude, l’impact de l’utilisation peropératoire du doppler microvasculaire sur les résultats de la chirurgie des anévrysmes intracrâniens ; plus particulièrement sur le pronostic fonctionnel des malades. Méthodes : Une étude rétrospective sur 7 ans allant de Janvier 2013 à Décembre 2019 a été menée au service de neurochirurgie de l’hôpital Fann de Dakar, Sénégal. Nous avons inclus tous les patients opérés pour l’exclusion d’un anévrysme intracrânien durant cette période. Ces patients ont été répartis en deux groupes sur la base de l’utilisation peropératoire du doppler microvasculaire ; et leurs paramètres évolutifs ont fait l’objet d’une étude comparative. Résultats : Notre cohorte comportait 266 patients et 287 anévrysmes ; l’âge moyen des patients était de 46 ans et le sex-ratio de 2,20. Sur l’ensemble des patients, 27% ont eu un contrôle doppler lors de l’exclusion de leur anévrysme et les 73% restants ont été opérés sans cette technique. Dans le groupe de patients opérés sans doppler nous avons noté 23,4% de nouveaux déficits et 12% d’ischémie post-opératoire ; 11% de décès et 7,3% de mauvais mRS à un mois de suivi. Chez les patients opérés sous contrôle doppler on notait 28,4% de nouveaux déficit, 14,8% d’ischémie post-opératoire ; 12,3% de décès et 2,7% de mauvais mRS à un mois. Conclusion : L’utilisation du doppler microvasculaire lors de la chirurgie des anévrysmes ne réduit pas la mortalité des patients mais améliore significativement la qualité de vie, avec un meilleur score de Rankin à un mois. Mots clés : Anévrysme intracrânien, microdoppler, clippage, peropératoire I- INTRODUCTION: From the early 1990s onwards, the management of intracranial aneurysms (ICA) was revolutionised by the advent of endovascular treatment, which has been continuously improved to this day. (13) Despite all the advances in neuroradiology, surgical treatment has retained its place in the management of ICA, with a better rate of complete occlusion. (19; 20; 14) However, there are complications associated with incorrect placement of the clip during surgery, such as a residual collar exposing the patient to the risk of rebleeding, or ischaemia occurring when one or more branches of the carrier vessel are inadvertently caught in the clip’s bites (6; 9). The morbidity and mortality associated with surgical treatment are therefore increased. The occurrence of these complications, despite meticulous microscopic inspection after clip insertion, has led to the development of techniques such as microvascular Doppler and fluorescein angiography to make the operation safer (8). In Senegal, despite the recent advent of embolisation, the treatment of intracranial aneurysms has remained surgical to date, due to a lack of financial resources for the vast majority of patients. Since the acquisition of microsurgical Doppler by our centre, aneurysmal microsurgeries have been systematically monitored by Doppler after clipping. We conducted a retrospective, descriptive and comparative study based on a prospective register of all patients who underwent surgery for the management of an intracranial aneurysm in the neurosurgery department of Fann national teaching hospital between January 2013 and December 2019. The aim of this study is to establish the impact of intraoperative use of microvascular doppler on outcomes of intracranial aneurysm surgery. II- METHODS II-a Design, setting and period of study: We conducted a retrospective, descriptive and comparative study based on a prospective register of all cases of intracranial aneurysms treated surgically in the neurosurgery department of Fann national university hospital. Based on a prospective register of all patients treated for neurovascular pathologies in the department, we carried out a retrospective selection of patients treated for intracranial aneurysms. We included in this study all patients who underwent surgery for the exclusion of an intracranial aneurysm during the period from January 2013 to December 2019, and whose medical records were complete and usable. II-b Parameters of interest, outcome and operational definitions: The parameters studied covered the following aspects: Epidemiological aspects (age, sex, risk factors, history, etc.). Clinical aspects (time to hospitalisation, length of hospitalisation, classification according to the WFNS clinical severity scale). Paraclinical aspects (results of angioscanner and angio-MRI, Fisher scannographic classification). Therapeutic aspects (time to surgery, type of procedure performed: clipping and/or coating). Evolutionary aspects (post-operative deficit, cerebral ischaemia, death; functional evolution assessed by the modified Rankin score:
We began with an overall descriptive study of this series. We then identified two groups of patients whose evolutionary parameters were the subject of a comparative study: Group 1: patients who underwent intracranial aneurysm surgery between January 2013 and August 2018 and who did not undergo intraoperative microvascular Doppler monitoring of aneurysm exclusion and vascular branch patency. Group 2: patients who underwent surgery between September 2018 and December 2019 and whose surgical procedure was monitored by microvascular Doppler. II-c Statistical analysis From a prospective database of patients hospitalised for intracranial aneurysms, established since 2013, we retrospectively collected the epidemiological, clinical, therapeutic and evolutionary data of our patients. These data were recorded, analysed and formatted using Excel 2016 and SPSS IBM version 24 software. The main parameters studied related to patient outcomes, namely: post-operative deficit, ischaemia, occurrence of death and Rankin score at discharge and at one month. Bivariate analyses were performed to determine correlations using the Pearson Chi² test and the Fisher test with a significance level of 0.05. The results were then presented in the form of a table of correlations. The results were then presented in the form of tables and graphs. II-d Ethical considerations The study was previously submitted to the ethics committee of national teaching hospital Fann of Dakar for approval and confidentiality was maintained throughout the study period. Informed consent of patients and/or responsible persons was obtained for all patients. III-RESULTS III-a Epidemiological and clinical aspects: Our study included 266 patients, 83 of whom were male (31%) and 183 female (69%), corresponding to a sex ratio of 2.20. Patient age ranged from 5 to 84 years, with an average of 46 years. The 46-55 age group was the most represented, with 26.7% of patients. The paediatric population (5-17 years) accounted for 4.1% of cases (11 patients). The average hospital stay was 15.6 days, with extremes ranging from 0 to 510 days. Thirty-six percent of patients were seen within 3 days, and 29.3% were seen after 10 days. The average length of hospitalisation was 23.3 days, with extremes ranging from 2 to 113 days. Grade I was the most common in the cohort (56.2%), followed by grade III and grade II, which concerned 23% and 11.3% of patients respectively. Grade IV was less represented with only 8.3%; and no patient in our series was grade V. III-b Paraclinical aspects: Cerebral CT scan without injection of contrast medium was performed in all our patients. It revealed subarachnoid haemorrhage. This was associated with a mass effect in 10.9% of patients. With regard to Fisher’s scan classification, score 4, found in 52.6% of patients, was the most common, followed by score 3 (17.3%). (Fig.1) A total of 287 aneurysms were identified in our 266 patients by CT angiography. Aneurysms were single in 249 of our patients (93.6%) and multiple in 17 (6.4%); of these, 12 patients had 2 aneurysms and 5 had 3. The aneurysms were saccular and fusiform in 90% and 7% of cases respectively. The shape of the aneurysms was not specified in 9 cases (3.1%). Aneurysms ranged in size from 2 to 44 mm, with a mean of 7.6 mm. Medium-sized aneurysms (5-9 mm) accounted for 39.4% of all aneurysms. The preferred location was the middle cerebral artery (sylvian), which accounted for 33.1% of all aneurysms. The vast majority of aneurysms were in the anterior circulation, with 268 aneurysms (93.4%) in the anterior circulation and 19 in the posterior circulation (6.6%). (Fig.2) The average delay to surgery was 25.8 days, with extremes ranging from 1 to 510 days. Type of surgery: All patients underwent aneurysm exclusion surgery:
(Fig.3) Among the patients who underwent aneurysm surgery, 72 (27%) had their aneurysm excluded and the patency of the vascular branches checked by microvascular Doppler during the operation, while 191 (73%) did not. (Fig.4) III-d Outcomes (Analytical results) The evolutionary parameters were first studied globally for the entire cohort, then comparatively between two groups of patients. After surgery, 66 patients developed a new deficit, i.e. 24.8% of all patients. Following the operation, 34 patients (12.8%) developed ischaemia. We recorded 30 deaths during our study, giving an overall mortality rate of 11.3%. At the time of hospital discharge, 156 patients (58.6%) had a good mRS and 74 (27.8%) a poor mRS. The mRS was not specified in 6 patients and 30 of them had an mRS of 6 (11.3%). III-d-1 Short-term outcome: immediate post-op A- Post-operative deficit Among the patients who presented a new deficit in the post-operative period, 45 belonged to group 1, i.e. 23.4% of the total number of patients, and 21 belonged to group 2, i.e. 28.4% of the total number of patients; p=0.403. There was no statistically significant difference in post-operative deficit between the two groups of patients (p>0.05). B- Ischaemia Of the patients with post-operative ischaemia, 23 were in group 1 and 11 were in group 2, i.e. 12% and 14.8% of the respective numbers in the two groups (p=0.486). For post-operative ischaemia, there was also no statistically significant difference between the two groups of patients (p>0.05). C- Death Of the patients who died, 21 were in group 1, representing a death rate of 11% in this group. The remaining 9 patients belonged to group 2, bringing the death rate to 12.3% in this group. (p=0,484). With regard to mortality, there was no statistically significant difference between the two groups. Furthermore, with regard to causes of death: of the 4 patients who died of proven post-operative ischaemia, 3 were in group 1 (75%) and only one was in group 2 (25%). D- mRS at discharge At the time of discharge, the distribution of the modified Rankin score in the two groups is shown in the following table: (Table 1). So in group 1, a good mRS was defined in 111 patients, i.e. 57.8%, and a poor mRS in 56 patients, i.e. 29.1%. On the other hand, in group 2, 45 patients (60.8%) had a good mRS and 18 (24.3%) had a poor mRS, p= 0.067. The use of micro-doppler seems to improve the mRS at discharge in patients in the second group, although the difference is not statistically significant (p>0.05). Fig.5 III-d-2 Long-term evolution A- mRS at 1 month After one month’s follow-up, a good mRS was noted in 31.3% of patients in group 1, compared with 10.8% in group 2; and a poor mRS in 7.3% and 2.7% of patients in groups 1 and 2 respectively. However, the mRS at one month could not be defined in 59.3% of patients in group 1 and 79.7% in group 2; p=0.004. The use of Doppler in the second group of patients significantly improved the mRS at one month in these patients (p<0.05). IV- DISCUSSION The mean age of patients in our study was 46 years, with a peak incidence between 46 and 55 years. This observation is in line with the literature, which shows that the average age of discovery of a stroke is around 50 (i.e. young), leaving significant neurological sequelae (7; 26; 3; 23; 21). Unlike other types of stroke, subarachnoid haemorrhage is predominantly suffered by women, and the excess risk associated with women increases with age. A significantly higher incidence of SAH has been observed in women aged 55 and over (11; 24). In our study, the predominance of women was also noted, with 69% of patients being female compared with only 31% male, corresponding to a sex ratio of 2.20. The same observations were made in the Barrow study, which found a sex ratio of 2.37 (21); as well as in Ahanogbe (Togo) (3) and Waweru (Kenya) (21), who found a sex ratio of 1.33 and 1.36 respectively in their studies. The explanation for this imbalance is still unknown, but it is probably not related to the currently recognised risk factors for subarachnoid haemorrhage, namely smoking, alcohol consumption and a history of high blood pressure, all of which are more common in men than in women. Several theories suggest that this difference in incidence between the sexes may be linked to hormonal factors, although the mechanisms by which these act remain unknown (6; 14). In our series, the average hospital stay was 15.6 days, with extremes ranging from 0 to 510 days (17 months). In contrast to the series by Ahanogbe (Togo) (3), the time to admission was shorter, at 3 ± 3.69 days, as was the case in the study by Hbali (Morocco) (18), in which 78% of patients were admitted within the first 3 days. This delay in diagnosis is mainly due to a lack of knowledge of the disease on the part of many practitioners and, above all, to the unavailability of neurosurgeons and CT scanners in certain areas of Senegal, leading to erroneous diagnoses and delays in treatment. Added to this is the problem of access to care, which remains difficult for a section of the population whose average per capita income is not sufficient to cover the immediate cost of a scanner, surgery or hospitalisation. In Senegal, public health policies are much more focused on the fight against infectious diseases and maternal and child illnesses, to the detriment of neurovascular pathologies, which still suffer from a lack of investment (26). The average length of hospitalisation was 23.3 days, with extremes ranging from 2 to 113 days. In our series, one patient died after 2 days in hospital, at 3 hours post-op, of unknown cause. On the other hand, the longer or shorter hospital stay in some patients is mainly due to the complications and serious after-effects that can result from meningeal haemorrhage. In the literature, the average length of hospitalisation varies considerably. Ahanogbe (3) found that the average hospital stay was similar to ours, at 21.8 ± 20.75 days, while Waweru (Kenya) (21) found a shorter average stay of 12 days. The length of hospitalisation therefore probably depends to a large extent on the patient’s initial clinical condition and whether or not there are complications after the operation. Grade I was in the majority, found in 56.2% of patients, followed by grade III which represented 23%. Thus more than half of our patients presented with low-grade SAH in good clinical condition on admission. Only 3.8% were grade IV and no grade V patients were recorded during the study. However, this favourable initial clinical status contrasts with the delay in admission, with 29.3% of patients admitted more than 10 days after initial symptoms. Our results differ markedly from those found in the Ahanogbe (Togo) study (3), where assessment of the WFNS score revealed 45.71% of severe SAH, either grade IV or V. The Fisher score of 4 in 52.6% of patients was the most common, followed by a score of 3 in 17.3%. These results are more or less similar to those of the Sghiouar study (25) in which 42.5% of patients had Fisher grade 4 SAH. The origin of the SAH was diagnosed by cerebral angioscan. In our study, 93.4% of aneurysms were located in the anterior circulation and 6.6% in the posterior circulation, as described in the literature. In our series, 249 patients (93.6%) presented with a single aneurysm and 17 with multiple aneurysms, i.e. 6.4%; 12 of these patients had 2 aneurysms and 5 had 3. These results are comparable to those of Mudjir et al (23), i.e. 3.9%, and contrast with those of Gueye et al (15), who found a slightly higher percentage of multiple aneurysms in their series, i.e. 8.7%, and Vaz G et al (12). This low rate of multiple aneurysms in our series could be explained by the low rate of detection of small aneurysms by angioscan, which can only detect aneurysms of more than 2 to 3 mm, with a sensitivity ranging from 77 to 97% (24); the smallest aneurysms therefore go undetected. Furthermore, angiography, which can explore all the cerebral arteries and thus detect all the aneurysms present, is not available in Senegal. All our patients underwent surgery to exclude their aneurysm; of these, 74.8% underwent clipping alone, 5.6% underwent coating alone and 14.2% underwent clipping combined with coating; the average time to surgery was 25.8 days, with extremes ranging from 1 to 510 days (17 months). In the 1990s, the international ISAT study compared the results of surgical and endovascular treatment of ruptured intracranial aneurysms, revealing a lower rate of adverse clinical outcome after endovascular treatment (23.7%) than after surgical treatment (30.6%). (22) Following this study, endovascular treatment of ruptured intracranial aneurysms has gradually increased, and a recent French study showed that around 80% of ruptured intracranial aneurysms are now treated endovascularly (10). However, in our context, this issue of choice of treatment does not arise, as in Senegal, surgery remains the only therapeutic option for the management of ICA. As endovascular treatment is very recent, it is not well known and poses a real financial and medium- and long-term follow-up problem for patients who systematically choose the surgical option. The rupture of an intracranial aneurysm is one of the most frequent neurosurgical emergencies; and despite the major advances made in the understanding and management of this pathology over the last 30 years, its prognosis remains unfavourable with an overall mortality rate of around 30%; and less than 50% of patients recover all their functional abilities (2; 1). The remainder of patients suffer numerous complications, ranging from major neurological deficits to subtle cognitive and behavioural difficulties, leading to a reduced quality of life (4). In the postoperative period, the complications recorded in our patients were essentially related to the appearance of a new motor deficit, cerebral ischaemia and death. An overall analysis of these results reveals that the rate of short-term complications is higher in group 2 than in group 1; paradoxically, this is due to the fact that patients in group 2 benefited from intra-operative microvascular Doppler monitoring when their aneurysm was excluded. However, it should be noted that the sample sizes of the two groups were far from proportional, with group 1 alone accounting for almost three times the number of patients in group 2, which may partly explain these unexpected results. Thus the use of Doppler appears neither to improve functional prognosis nor to reduce mortality in these patients, contrary to what might logically be expected. Nevertheless, it is clear that microvascular Doppler seems to provide valuable intraoperative information to guide clip placement (5). At discharge, the first group had 57.8% good mRS and 29.1% poor mRS. On the other hand, in group 2, 60.8% of patients had a good mRS and 24.3% a poor mRS (p= 0.067). Analysis of these results shows that patients in group 2 had a better Rankin score at discharge than those in the first group. However, there was no statistically significant association between the use of the Doppler probe in patients in group 2 and an improvement in their mRS at discharge. At one month’s follow-up, 7.3% of patients in group 1 had an unfavourable Rankin score compared with only 2.7% with a poor mRS in group 2 (p=0.004). This time, there was a statistically significant link between the use of doppler and an improvement in the Rankin score in these patients. However, the mRS at one month could not be defined in 65% of patients, as it was not recorded in the files at the follow-up appointment. The number of missing data relating to patient progress was therefore very high. The main limitation of this study is the inequality of the samples making up the two groups, with the second group being almost three times smaller than the first. V- CONCLUSION The surgical treatment of cerebral aneurysms is currently the preferred therapeutic option for the Senegalese population because of its very affordable financial cost. This treatment is affected by complications such as the infarction of an arterial territory following an occlusion of collateral arterial branches despite a careful intraoperative exploration. The analysis of our results reveals that the use of microvascular doppler during intracranial aneurysm surgery does not reduce mortality; but has a favorable impact on improving quality of life with notably a higher score of Rankin, Both at the hospital discharge and one month post-op. 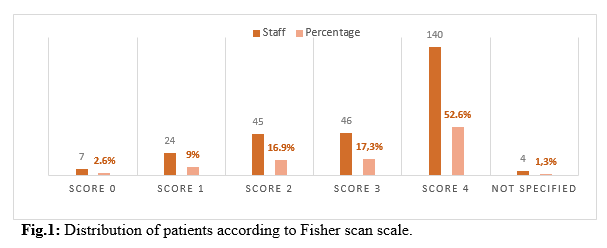 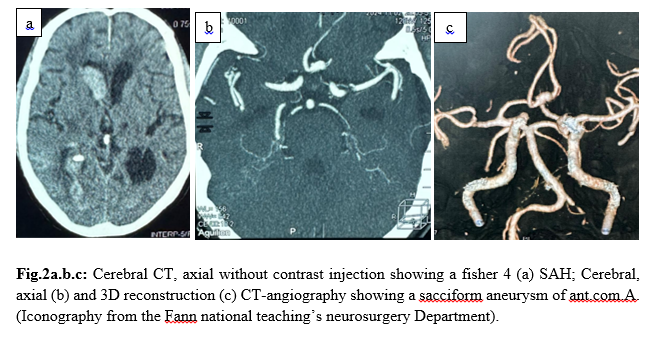 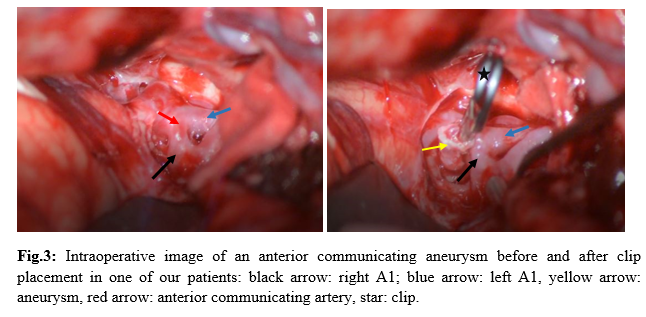 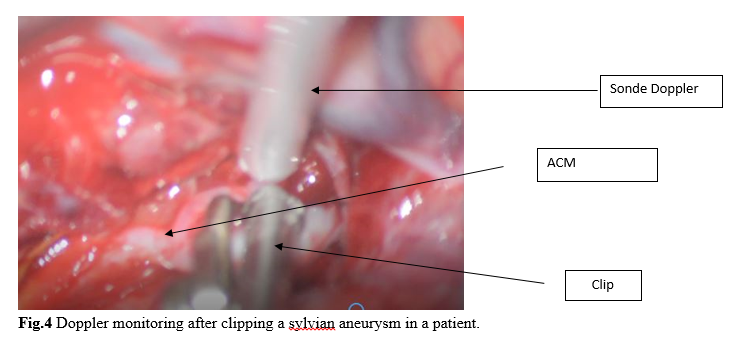 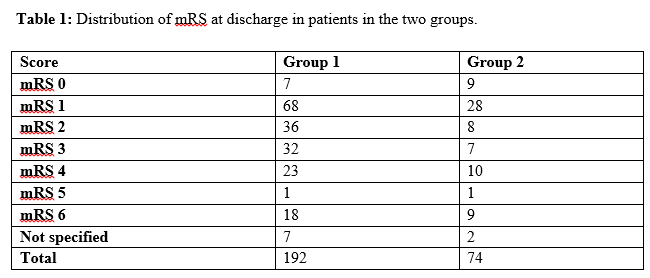 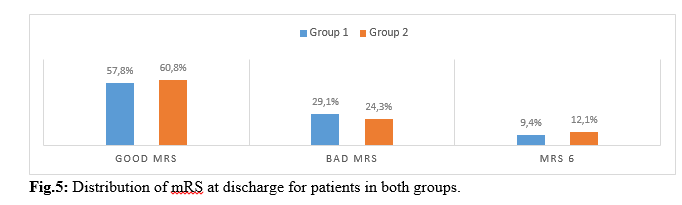 REFERENCES
|
© 2002-2018 African Journal of Neurological Sciences.
All rights reserved. Terms of use.
Tous droits réservés. Termes d'Utilisation.
ISSN: 1992-2647