
|
|||
|
CASE REPORT / CAS CLINIQUE
INVASIVE DISSEMINATED ASPERGILLOSIS WITH MULTIPLE INTRACRANIAL LOCALIZATIONS ASSOCIATED TO CHRONIC GRANULOMATOUS DISEASE: CASE REPORT.
ASPERGILLOSE INVASIVE DISSEMINEE AVEC LOCALISATIONS CEREBRALES MULTIPLES: A PROPOS D'UN CAS.
E-Mail Contact - BAKHTI Souad :
bak-sou@hotmail.com
ABSTRACT Invasive disseminated aspergillosis with intracranial localization is a rare disease. It often affects immunocompromised patients. Most aspergillosis cases are caused by Aspergillus fumigatus; in very rare instances Aspergillus nidulans can be the cause. Management of intracranial lesions associated with invasive aspergillosis involves surgery with medical treatment. Overall prognosis of cerebral aspergillosis is poor. We report the case of an eight-year-old girl with history of recurrent infections who presented an invasive disseminated aspergillosis with multiple intracranial localizations. This patient had surgery and medical treatment but died of hepatitis B infection after 40 months follow-up. RESUME L’apergillose invasive disséminée avec localisation cérébrale est une pathologie rare. Elle survient le plus souvent dans le cadre d’une immunodépression. Le type d’aspergillus responsable de ce tableau est le plus souvent l’Aspergillus fumigatus ; il peut s’agir exceptionnellement d’un Aspergillus nidulans. La prise en charge des lésions cérébrales entrant dans le cadre de cette pathologie comprend la chirurgie et le traitement médical. Le pronostic est très sombre. Nous rapportons le cas d’une fillette âgée de 8 ans, ayant dans les antécédents une histoire d’infections répétées, qui a présenté une aspergillose invasive disséminée avec localisations cérébrales multiples. Cette patiente a été traitée par chirurgie et traitement médical. Elle est décédée d’une hépatite B au bout de 40 mois. Key words: Invasive aspergillosis. Aspergillus nidulans. Intracranial localizations. Chronic granulomatous disease. INTRODUCTION Invasive disseminated aspergillosis is a rare mycosis infection (1). Cases with intracerebral localization are very uncommon. Aspergillosis is generally caused by Aspergillus fumigatus and Aspergillus flavus (11, 14). The most common portal of entry is respiratory system (1, 11, 14). These mycosis infections are most often present in immunocompromised patients (10). Morbidity and mortality rates are high (7). Infections caused by Aspergillus nidulans are extremely rare and morbidity and mortality rates are higher than those observed in cases infected by Aspergillus fumigates (15). Infections by Aspergillous nidulans appear to occur mainly in patients with chronic granulomatous disease (15). We report a case of an eight-year-old girl with invasive disseminated aspergillosis and multiple intracerebral localizations caused by an Aspergillus nidulans. CASE REPORT An eight-year-old girl was referred to our department on February 2009. This child has presented 3 years previously with Kala Azar infection followed by pulmonary tuberculosis one year later. She developed subcutaneous abscesses on the chest and the right arm 4 months prior to her referral to our department. Cytopuncture of these lesions revealed mycelial filaments and aspergillar serology was positive. Subcutaneous nodule communicating with lungs and mediastinal nodules were present on chest CT scan (Fig. 1). The child was treated by Caspofungine because Voriconazole was not available at this time in Algeria. Two months later, she developed seizures and intracranial hypertension. Cranial CT scan revealed a right parietal multi lobular lesion with cystic areas and high enhancement with contrast iodine solution; there was also a moderate edema (Fig. 2) and bone erosion was noted (Fig.3). Three other small nodular lesions were present in the left temporal lobe (Fig. 4 A), the left parietal lobe (Fig. 4 B) and the posterior fossa (Fig. 4 A). At admission the patient was conscious (Glasgow Coma Scale at 15) in poor conditions with a significant weight loss, a polypnea with 27 cycles / mn; she was febrile (T° at 38.9° C). Pulmonary exploration revealed a severe restriction syndrome with significant anomalies of perfusion. Neurological examination revealed a right spastic hemiplegia without facial involvement. The main lesion was operated on. Intra-operatively, we noted a dural tear with exteriorization of the lesion causing bone erosion. The lesion consisted of fleshy and abscessed areas. Lesion was sometimes tightly attached to the brain (Fig. 5).We achieved gross total resection. Histology revealed granulomas with giant cells in contact with aspergillar bodies (Fig. 6). Parasitic studies showed an Aspergillus nidulans. Surgery was followed by medical treatment (Voriconazole which was introduced in our country especially for this patient). Biologic and immunologic investigations concluded to a chronic granulomatous disease. Evolution was good with persistence of a mild motor deficit. Control CT scans showed a total disappearance of the lesions (Fig. 7). However the patient died of hepatitis B infection after 40 months of follow-up. DISCUSSION Apergillus fumigatus is the most frequent type of aspergillus in invasive disseminated aspergillosis (1, 2, 15). Aspergillus infection is mostly by hematogenous route from the lungs (1, 11, 14). Rate of occurrence in these cases is about 10% (11). There was also lung localization in our patient. In immunocompromised patients, infection can be a sinusitis, a pneumonitis or a localized infection on a chronic disease (1, 7). Our patient had pulmonary tuberculosis. Intracranial localization is rare and occurs mainly in immunocompromised patients (7). However, this disease is reported also in immunocompetent patients mainly those who live in countries with temperate climate (14). Cerebral CT scan may reveal tumoral forms of intracranial aspergillosis and show images of abscess (ring enhancing lesion) or granuloma (nodular images). Our patient presented with both. In many cases, lesions involve the frontal and the temporal lobes (13). Aspergillosis is rarely due to Aspergillus nidulans. This condition is almost exclusively observed in cases with chronic granulomatous disease (8, 15) which is an X-linked genetic condition or autosomal recessive inherited (4). This disease is secondary to defects in the nicotinamide adenine dinucleotide phosphate (NADPH) oxidase which is an enzyme complex responsible for the phagocyte respiratory burst (12).Chronic granulomatous disease (CGD) predisposes patients to recurrent bacterial and fungal infections (15). First documented report of a child with intracranial aspergilloma in association with CGD has been published by Dean in 1993 (6). Our patient had a proven CGD and presented 3 types of infections: parasitic, bacterial and fungal. A combination of surgical and medical treatment is the best management for intracranial tumoral forms of aspergillosis (2, 7, 11, 13, 14). Radical resection is the best option when feasible since it permits to remove areas of low drug penetration which may contain viable fungi (11, 13). Some authors advocate stereotactic aspiration of abscess in eloquent areas (11) and lobectomy in non eloquent areas (13). Prognosis seems to be better in cases operated by radical resection (13). This is confirmed in our case since she survived 40 months and died from another cause. Voriconazole is widely used now because results are better than those observed with Amphotericin B. Moreover side effects of Voriconazole are less severe (3, 9, 11). The exact duration of medical treatment is not defined but it seems that it must be prolonged. However prognosis of invasive disseminated aspergillosis with intracranial localization is poor even with aggressive treatment (1, 2, 7, 10, 11, 15). Rate of mortality reaches100% in immunocompromised patients while it is reported to be near 67% in immunocompetent patients (1, 2, 11) and most deaths are observed during the first year. Our patient had a survival of 40 months. CONCLUSION Invasive disseminated aspergillosis with intracerebral localization caused by Aspergillus nidulans is a very rare condition. Chronic granulomatous disease should be suspected in these cases and appropriate work up sought and performed. Treatment should be aggressive to achieve a mid to long survival while keeping in mind that the prognosis is often bleak. 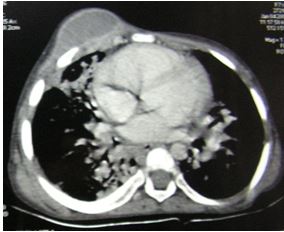 Figure 1 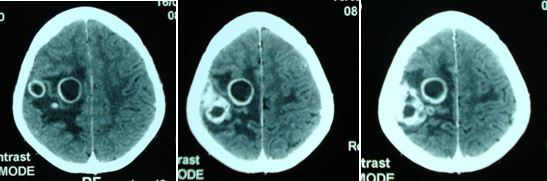 Figure 2 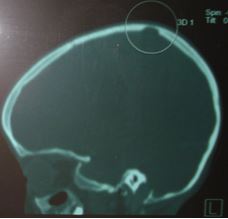 Figure 3 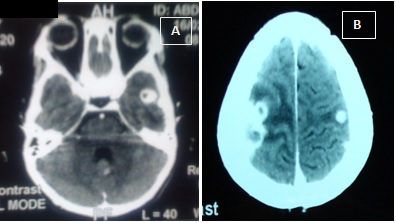 Figure 4 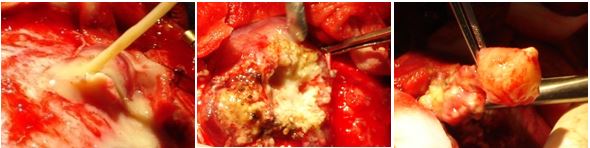 Figure 5 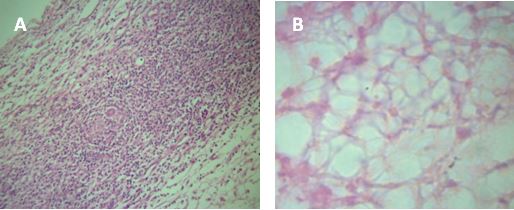 Figure 6 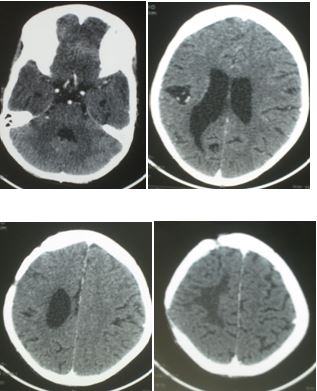 Figure 7
REFERENCES
|
© 2002-2018 African Journal of Neurological Sciences.
All rights reserved. Terms of use.
Tous droits réservés. Termes d'Utilisation.
ISSN: 1992-2647