
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
ORIGINAL PAPERS / ARTICLES ORIGINAUX
NEUROLOGIC EMERGENCIES AND RELATED DEATHS: A CALL FOR STROKE MANAGEMENT IN ORGANIZED STROKE UNITS IN TROPICAL HOSPITALS.
URGENCES NEUROLOGIQUES ET DÉCÈS CONNEXES : UN APPEL POUR LA GESTION DES ACCIDENTS VASCULAIRES CÉRÉBRAUX DANS LES UNITÉS NEUROVASCULAIRES DANS LES HÔPITAUX TROPICAUX
E-Mail Contact - NWANI Paul Osemeke :
paul.nwani@yahoo.com
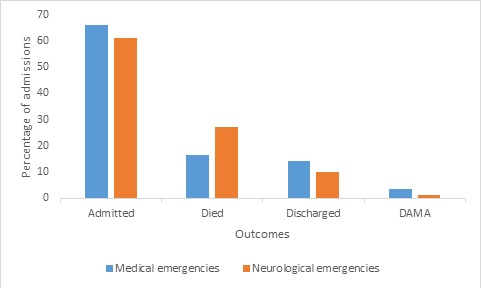
ABSTRACT: Background: Neurologic emergencies are common and often times the outcome is unfavorable. This was a study of the frequency of neurologic emergencies and related deaths in the medical emergency department of a tropical tertiary healthcare center aimed at highlighting the lingering high frequency of neurologic emergencies and related deaths with a view to make suggestions on how to improve outcome. Methods: This was a two-year retrospective review of neurologic emergencies and related deaths at the medical emergency department of a Nigerian tertiary hospital. Results: A total of 1302 medical emergency patients comprising 688 (52.8%) males and 614 (47.2%) females were studied. Neurologic diseases were the most frequent medical emergencies, accounting for 21.4% (n=278) of cases. Stroke was the most frequent neurologic emergency accounting for 64.7% (n=180/278) of neurologic emergencies. There were a total of 214 medical emergency deaths of which neurologic diseases accounted for 35.04% (n=75/214). Stroke was also the most frequent cause of all medical emergency deaths accounting for 25.2% (n=54/214) of all medical emergency deaths and 71.1% (n=54/75) of deaths due to neurologic diseases. Conclusions: Neurologic emergencies and its related deaths are high especially death from stroke and this requires urgent attention. Introduction of stroke units has been shown to improve stroke management outcome where they exist, but such units are largely lacking in most tertiary centers in the tropics. It is time for the establishment of such units in these centers given the high number of deaths due to stroke as seen in this study. Key words: Neurologic deaths – Neurologic emergencies – Stroke – Stroke units – Tropics. RESUME: Contexte : Les urgences neurologiques sont fréquentes et souvent leur résultat est défavorable. Il s’agissait d’une étude sur la fréquence des urgences neurologiques et des décès connexes dans le service d’urgences médicales d’un centre de soins tertiaires tropicaux visant à mettre en évidence la fréquence élevée persistante des urgences neurologiques et des décès connexes en vue de faire des suggestions sur la façon d’améliorer les résultats. Méthodes : Il s’est agi d’un examen rétrospectif de deux ans des urgences neurologiques et des décès connexes au service d’urgences médicales d’un hôpital tertiaire nigérian. Résultats : Au total, 1302 patients, dont 688 (52,8 %) hommes et 614 (47,2 %) femmes, ont été étudiés. Les maladies neurologiques étaient les urgences médicales les plus fréquentes, comptant pour 21,4 % (n=278) des cas. L’AVC était l’urgence neurologique la plus fréquente, représentant 64,7 % (n=180/278) des urgences neurologiques. Il y a eu un total de 214 décès d’urgence médicale dont les maladies neurologiques représentaient 35,04 % (n=75/214). L’accident vasculaire cérébral était également la cause la plus fréquente de tous les décès d’urgence médicale, représentant 25,2 % (n=54/214) de tous les décès d’urgence médicale et 71,1 % (n=54/75) de décès attribuables à des maladies neurologiques. Conclusions : Les urgences neurologiques et les décès connexes sont élevés, en particulier les décès causés par un accident vasculaire cérébral, ce qui nécessite une attention urgente. L’introduction d’unités d’AVC a été démontrée pour améliorer les résultats de gestion d’AVC là où elles existent, mais ces unités sont largement absentes dans la plupart des centres tertiaires des tropiques. Il est temps de mettre en place de telles unités dans ces centres étant donné le nombre élevé de décès dus à un accident vasculaire cérébral, comme le montre cette étude. Mots clés: accident vasculaire cérébral – décès neurologiques – unités neurovasculaires – urgences neurologiques – tropiques. INTRODUCTION Neurologic conditions are among the common reasons for presentation to the medical emergency departments and often times the outcome is unfavorable (19,7). Neurological disorders are the leading cause of disability and the second leading cause of death worldwide (5). In 2016, there were 13.7 million new strokes globally, and stroke was the second leading cause of death (5.5 million) and disability-adjusted life years (DALYs; 116.4 million) worldwide (5). Deaths attributable to neurologic disorders can be reduced if patients presenting to the emergency departments are promptly assessed and management commenced by appropriately trained physicians adequately equipped for interventional neurology and incase of stroke patients in organized stroke units. Such organized units are however largely lacking in most tropical hospitals, even in the tertiary health facilities in Nigeria (1). Poor outcome of neurologic emergencies especially stroke led to the establishment of organized stroke units equipped for prompt diagnosis and multidisciplinary care of stroke patients from admission till discharge in developed countries with promising results (2,9,14,21). There are only a few centers in the tropics with functional established stroke units and the need for such neuro-care units cannot be overemphasized given the enormity of deaths due to stroke in these regions. In 2005 neurological disorders constituted 16.8% of the total deaths in lower middle income countries compared with 13.2% of the total deaths in high income countries and this is projected to even rise higher (4). On this background we set out to determine the frequency of neurological emergencies and deaths related to neurological diseases at the medical emergency unit of a tropical tertiary hospital and to highlight the need for urgent interventions. MATERIALS AND METHODS Study Design: This was a two year-retrospective review of patterns and outcome of neurological diseases and related deaths at the emergency department of the Nnamdi Azikiwe University Teaching Hospital Nnewi between January 2016 and December 2017. The Nnamdi Azikiwe University Teaching Hospital (NAUTH) is a 450 bed tertiary hospital located in Nnewi. Nnewi is in Anambra State in Southeastern Nigeria. Anambra State occupies an area of 4,844 Kmsq and has a population of 4,182,032 according to the 2006 Nigeria population census (10). NAUTH is the largest medical referral center in the state and serves the over four million people in Anambra State and the surrounding Delta, Abia and Imo states. Patients presenting with medical conditions are first seen by emergency care physicians whose major task is initial acute care and triage of patients and subsequent referral to the medical resident on emergency ward call. The neurology unit is invited thereafter to continue or take over management of patients with neurological disorders. Currently there is no existing stroke unit at NAUTH just like most other hospitals in the country, secondary and tertiary alike. Patients All the medical emergencies that presented to the emergency department during the period under review were identified using the emergency registers as well as the nurses’ registers and records. Data extracted from the records included the patients’ demographic data, the clinical diagnosis at time of leaving the emergency unit by any of the following outcome measures; death, admission into the ward, discharges home or discharged against medical advice. Information obtained was entered into a pro forma for analysis. Statistical Analysis Data was analyzed using Statistical Package for the Social Sciences SPSS version 20.0 (SPSS Chicago Inc., Illinois (IL), U.S.A). Relevant percentages, frequencies, means and standard deviation were calculated and findings represented with relevant tables and figures. Ethical approval Ethical approval was obtained from the Nnamdi Azikiwe University Teaching Hospital Nnewi Ethics Committee. Study codes were used to represent each patient and confidentiality maintained. Waiver for individual informed consent was granted by the ethical committee due to the non-experimental nature of the study and its non-invasiveness and the retrospective nature of the research using hospital records. RESULTS: A total of 1550 cases were reviewed but only 1302 cases had sufficient demographic and clinical data to be recruited in the study. There were 688 (52.8%) males and 614 (47.2%) females with a mean age of 50.87±18.22 and age range of 17 to 100 years. Of the 1302 medical cases, 278 cases were neurologic disorders and they comprised of 163 (58.6%) males and 115 (41.4%) females with an age range of 18 to 100 years. Table 1 shows the systemic distribution of the medical cases at the emergency department with neurological diseases and infectious diseases accounting for 21.4% (n=278) and 21.1% (n=275) of medical emergencies respectively. Among neurological diseases cerebrovascular accident (stroke) was the most frequent neurological disease accounting for 64.7% of cases (n=180/278), while cord compression was least accounting for 2.9% (n=8) (Table 2). The percentage of the patients in the different age groups presenting with the three major neurological disorders are shown in table 3. The percentage of those with cerebrovascular disease increased from 14.3% in the age group ≤29 years to 89.1% for those between 60-69 years, while the percentage of patients with meningoencephalitis decreased from 17.9% in age group ≤29 years to 2.0% in age group 60-69 years. The outcome of the medical and neurological emergencies is shown in figure 1. Of the 1302 medical emergencies 859 (66.0%) were admitted; 214 died (16.4%); 184 (14.1%) were discharged while the remaining 45 (3.5%) were cases of discharge against medical advice. Of the 278 neurological emergencies 171 (61.5%) were admitted; 75 died (27.0%); 28 (10.1%) were discharged while the remaining 4 (1.4%) were cases of discharge against medical advice. Of the 75 neurological deaths, 42 (56.0%) were male while 33 (44.0%) were female. Death due to neurological diseases accounted for 5.75% (n=75/1302) of all the medical emergency admissions and 35.04% (n=75/214) of medical emergency deaths during the period. The mean age of the neurological death was 57.01±19.77. The causes of neurological deaths are shown in table 4 with cerebrovascular accident (Stroke) accounting for 71.1% of neurological death (n=54), meningoencephalitis accounting for 11.8% (n= 9) and other causes for the remaining 17.1% (n=37). DISCUSSION: Neurologic emergencies are major causes of morbidity and mortality and have been estimated to increase in the lower and middle income countries (4). This estimate is evidenced in this study as neurologic emergencies were the most common causes of medical emergencies accounting for 21.4% of all medical emergencies. Of these neurologic causes, stroke was a major cause of morbidity accounting for 64.7% of cases. The finding in this study is higher than 14.7% and 10-15% reported in France and Spain respectively (15,3), but lower than 25.7% reported earlier in Calabar, Southern Nigeria and 27.2% reported in Douala, Cameroun (18,13). Though the neurological emergencies reported in this present study is lower than the earlier Calabar report, 64.7% of the neurological diseases in this present study were due to stroke compared to 52.5% reported in Calabar. It is also worth noting the higher percentage of neurologic emergencies reported in Douala might have been accounted for by the inclusion of traumatic causes among the neurological emergencies. The higher rate of stroke among medical emergencies in this study may be attributable to the increasing frequency of risk factors for strokes like hypertension, diabetes mellitus, and adoption of western lifestyles by Nigerians, in addition to the increasing stress in the society. A comparison of our study with that of Ekanem et al. (18) in Calabar indicates a similar frequency of meningoencephalitis in both studies accounting for 11.2% and 11.3% of cases respectively. However, seizure disorders were more frequent in our study accounting for 9.3% of cases compared to 0.7% reported in Calabar (18). Primary headache accounted for only 1.1% of neurological emergencies in our study; this is within 0.6 to 2.8% reported in other studies (6,11,12). The mean age of the patients with neurologic disease in this study is 55.00 ± 18.65 years with a male to female ratio of 1:1.4. This is higher than the mean age of patients in an Indian study with a mean age of 37.4±19 years (20) but comparable to the mean ages found in Spain and France which were 59 years and 56.9±21years respectively (19, 2). These countries have different sociocultural backgrounds, life expectancy and differing neurologic disease that bring them to the emergency rooms. The reason for the similarity with findings in Europe is not immediately obvious but the increasing adoption of western lifestyle by Nigerian communities may be contributory. What is more significant however, is that these neurologic emergencies are affecting the working population of the community and diseases like stroke leave the sufferers with disabilities and make them economically unproductive. Age dynamics is clearly noted to play a role in the different causes of neurologic diseases in this study. Age has been strongly associated with stroke and this is highlighted in this study with stroke occurring more in the patients aged 40 years and above with a peak among the 60-69 age group. Seizure disorders were more prevalent in those <29 years while meningoencephalitis was found mainly in the middle age group of 30-49 years. Meningoencephalitis ranked as the second most common cause of neurologic emergency in this present study, a finding similar to an earlier Nigerian study (18). However, reports in the 1990s in Africa put infectious causes as the most frequent causes of emergency room admission (8). This change may buttress the fact that as infections are being controlled through adequate preventive measures and prompt use of antibiotics, non-communicable diseases like hypertension, diabetes mellitus and obesity which are the risk factors for stroke on the other hand are on the increase. Infections were more in the younger age groups in this study which may also not be unrelated to their engagements in risky health behaviors that make them more vulnerable to meningoencephalitis and HIV infections. Death due to neurological disorders accounted for 35.04% of the medical admission deaths while stroke alone accounted for 71.1% of neurologic disease related deaths and 25.2% (n=54/214) of medical emergency deaths during the period under review. The rate of 35.04% obtained in this present study is higher than 5.21% obtained for all non-trauma causes of emergency room death reported by Ugare et al. (22) in Calabar. In the Calabar study cardiovascular diseases which includes stroke accounted for about a quarter (25.0%) of non-trauma causes of emergency room deaths. It is also worth noting that though the above study was published in 2012 it was a retrospective report of deaths at the emergency room between 2005 and 2007 a decade earlier than our report. This higher rate obtained in our study may be indicative of the increasing death rates associated with neurologic emergencies in the tropics. Similarly, 25.2% (54/214) of all medical emergency deaths in this present study were due to stroke which is higher than 17.4% reported in southwest Nigeria (16). Studies on death in emergency departments in Nigeria has shown high mortality from stroke, though most of the studies grouped stroke with cardiovascular diseases thereby preventing direct comparison (17,22). CONCLUSIONS: Neurologic emergencies and related deaths are on the increase especially death from stroke and this requires urgent attention. Introduction of stroke units has been shown to improve stroke management outcome where they exist and such units are largely lacking in most tertiary centers in the tropics. It is time for the establishment of such units in these centers given the predicted and actual high number of deaths due to stroke as seen in this study. When such services are available with adequate policies and patients education stroke outcome will hopefully improve in the tropics. CONFLICT OF INTEREST None declared.
Table1: The distribution of causes of medical emergencies according to systems
GIT (Gastroenterology). Others include: toxicity (6); psychiatry (10); musculoskeletal (7); dermatology (1)
Table 2: Causes of Neurological emergencies
Others: Peripheral neuropathy (2); delirium (1); Rabies (1); Parkinson’s disease (1) Multiple sclerosis (1). HTN: hypertension; RVD: retroviral disease; GBS: Guillain Barre Syndrome; SOL: space occupying lesion.
Table 3: Age distribution of the major neurological diseases.
*Actual number of patients is in parenthesis. a The total number of patients in each age group
Table 4: Causes of Neurological death
 DAMA (Discharged against medical advice) REFERENCES
|
© 2002-2018 African Journal of Neurological Sciences.
All rights reserved. Terms of use.
Tous droits réservés. Termes d'Utilisation.
ISSN: 1992-2647