
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
PATTERN OF INTRACRANIAL TUMOURS IN A TERTIARY HOSPITAL IN GHANA
PATTERN OF INTRACRANIAL TUMOURS IN A TERTIARY HOSPITAL IN GHANA
E-Mail Contact - EKPENE Ubong :
ubongekpene@yahoo.com
ABSTRACT Background Brain tumours are relatively common neurosurgical conditions. Variable patterns have been described in the literature. This study seeks to unravel the pattern of intracranial tumours in Korle Bu Teaching Hospital (KBTH) based on patient demographics, clinical presentation, spatial distribution of tumor and histological findings. Method Study design is retrospective, descriptive. Data was obtained from theatre and ward records of patients treated at the neurosurgery unit of Korle Bu Teaching Hospital between January 2010 to December 2015, and histology reports obtained from the histopathology unit. Patients with intracranial tumours without definitive histological diagnosis were excluded. Histological and demographic patterns of tumours were analyzed with SPSS version 21. Results Preliminary result shows that of the 102 histologically diagnosed brain tumours, out of 335 brain tumour cases seen in the period under review, 58 (56.9%) were females and 44 (43.1%) were males. Glioma were the commonest intracranial tumours – 39(38.2%) followed by Meningioma with 37(36.2%) and pituitary adenoma – 9(8.8%). Astrocytoma was the commonest type of Glioma comprising 30(77%) of the 39 cases. Meningotheliomatous meningioma was the commonest type of meningioma with 11 (29.7%) of 37 cases. Of the 39 Gliomas 17(43.6%) were males and 22(56.4%) were females, while for the Meningioma 17(46%) were males and 20(54%) were females. The commonest symptom was headache (64%) and the commonest tumour location was supratentorial. The crude incidence rate of intracranial tumour in this study was 1.34 per 100,000 population per year. Conclusion Intracranial tumours may be relatively common in Ghana but grossly underdiagnosed due to lack of an efficient national surveillance programme and tumour registry. Gliomas are the commonest. Overall females are more commonly affected than males, including both gliomas and meningiomas. Key words: Histological diagnosis, Intracranial tumours, Korle Bu Teaching Hospital. INTRODUCTION Intracranial tumours include tumours arising from the brain or its surrounding tissues. Intracranial tumours remain a major cause of morbidity and mortality worldwide. The annual, global, age standardized incidence of primary malignant intracranial tumours is approximately 3.7 per 100,000 for males and 2.6 per 100,000 for females.[7] In the US the incidence rate of all primary malignant and non-malignant brain and CNS tumours between 2008 to 2012 was 21.97 cases per 100,000, the rate being higher in females (23.95/100,000 for a total count of 206,565 incident tumours) than males (19.82/100,000 for a total count of 150,271 incident tumour).[2] They are commoner among Caucasians.[5] Gliomas are the commonest group of intracranial neoplasms in both adults and children.[5,12] Gliomas are commoner in males while meningiomas are commoner in females.[5,8] MATERIALS AND METHODS This study is a retrospective, descriptive study based on data obtained from the hospital records of patients with intracranial tumours, diagnosed using Computed Tomography scan and/or Magnetic Resonance Imaging and treated in Korle Bu Teaching Hospital between January 2010 and December 2015. Korle Bu Teaching Hospital is the foremost teaching hospital in Ghana and the third largest teaching hospital in Africa, with a bed capacity of 2000[9]. Majority of the intracranial tumour cases in the country are treated in this hospital, being the national referral centre. An average of 2 new cases of intracranial tumour is seen at the neurosurgical clinic of the hospital every week besides those that present at the emergency room. There are three other centres where very few brain tumour surgeries are done in Ghana. RESULTS A total of 335 patients with intracranial tumours were seen in the period under review out of which 274 had surgical interventions ranging from stereotactic biopsy to open excision biopsy and ventriculoperitoneal shunting. 102 of these had histologically confirmed tumour described according to the WHO classification of Nervous system tumours. The overall gender distribution is shown in Table 1. Table 1: Overall Gender distribution of intracranial tumours seen between 2010 and 2015.
Table 2: Tumour type and gender distribution
Histological distribution of the tumour is as shown on Table 2. Glioma is commonest with 38.2%, slightly higher than meningioma accounting for 36.2% of tumours seen. Pituitary adenoma and metastatic tumours account for 8.8% and 7.9% respectively. In all the aforementioned tumours females tend to have slight preponderance compared to males, but markedly so in the metastatic group with three-quarter being females. Overall, there were also more female patients with intracranial tumours. Table 3: Histological type and age distribution
Tumour distribution based on intracranial location is shown in Table 4 below.  Figure 1 Table 4: Tumour distribution based on location
The distribution of meningioma based on location is as shown on Figure 1. Convexity meningioma is the commonest making up 15 of 37 cases, followed by sphenoid wing meningioma and parasagittal meningioma with 8 and 6 respectively. 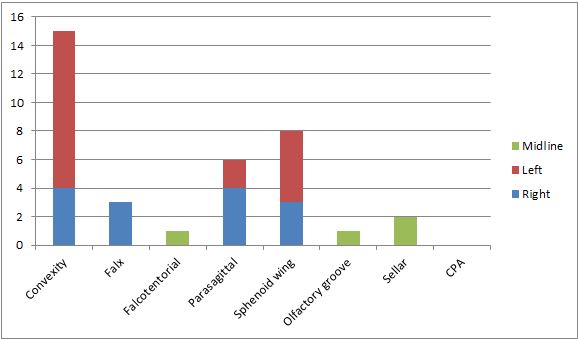 Figure 2 Table 5 below shows the commonest symptoms and signs in these patients with intracranial tumours. The percentages were calculated based on 62 patients with detailed symptomatology. Table 5: Main symptoms and signs
DISCUSSION Intracranial tumours are relatively common neurosurgical conditions and are associated with high morbidity and mortality. Patterns of distribution of these tumours vary across the globe. This study sought to determine the pattern of intracranial tumours in neurosurgical patients with intracranial tumours who presented at Korle Bu Teaching Hospital, Accra, Ghana for treatment between January 2010 and December 2015. 102 histologically diagnosed intracranial tumours out of 335 radiologically diagnosed intracranial tumours were included in the study. Gliomas were the commonest tumour type accounting for 38.2% of intracranial tumours followed closely by meningioma (36.2%). This is in keeping with findings in other studies.[8,11,17,6,13,15,3] Although gliomas are reported to be commoner in females, there was a slight female preponderance in this study, which is similar to an earlier publication in Tema, Ghana by Andrews et al.[1] This may be the true picture or just a reflection of the fact that females tend to seek medical treatment more than men with similar conditions in Ghana. Tuberculoma have been reported to mimmick malignant tumours[14,16,10] but we have not found this to be common among our patients. The limitation of this study is the relatively small sample size, the low histological diagnosis rate and incomplete data in some patients’ records. CONCLUSION Intracranial tumour may be relatively common in Ghana but grossly under diagnosed. The crude incidence rate of intracranial tumour in this study was 1.34 per 100,000 population per year. Glioma was the commonest intracranial tumour in this setting followed by meningioma. Females were more affected by glioma, meningioma, pituitary and metastatic tumours than males. Overall females were more at risk of intracranial tumours than men in this setting. Astrocytoma was the commonest type of Glioma. Meningotheliomatous meningioma was the commonest type of meningioma. Age of patient at diagnosis varied with the tumour with the youngest age affected being 1 year and the oldest age 73 years. Pilocytic astrocytoma was the commonest paediatric tumour, followed by medulloblastoma and ependymoma. The commonest symptom was headache and the commonest tumour location was supratentorial. Convexity meningioma was the commonest location of meningioma. |
© 2002-2018 African Journal of Neurological Sciences.
All rights reserved. Terms of use.
Tous droits réservés. Termes d'Utilisation.
ISSN: 1992-2647