|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
ORIGINAL PAPERS / ARTICLES ORIGINAUX
RADIATION DOSE EMISSION DURING SPINE SURGERY WITH INSTRUMENTATION: RAISING AWARENESS IN SUBSAHARAN AFRICAN SPINE SURGEONS
DOSE D’IRRADIATION EMISE AU COURS DE LA CHIRURGIE RACHIDIENNE AVEC OSTEOSYNTHESE
E-Mail Contact - KONAN Meleine Landry :
Landrix07@gmail.com
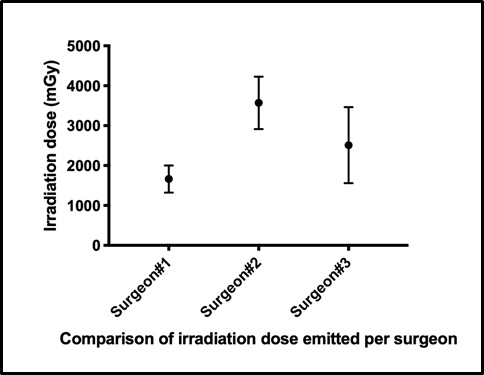
ABSTRACT Introduction Spinal osteosynthesis are procedures requiring accuracy for vertebral identification as well as pedicle screw insertion. For this purpose, fluoroscopy became mandatory equipment in the operating room. However, this imaging tool is a source of X-rays putting the patients and the surgical team at high risk of irradiation. The objective of this paper is to assess the radiation exposure to spine surgeons and discuss the related risks. Method We performed a retrospective study from January 2012 to October 2013 based on 47 spinal procedures in which the radiation doses and the exposure time were recorded in the fluoroscope internal software. Three senior spine surgeons performed the surgeries which involved the cervical segment (n=15), the dorsal segment (n=5) and the lumbar segment (n=27). The spinal instrumentations were from the same manufacturer. Results The average radiation dose per surgery (all segments included) was 2480.12 mGy/cm2 with 21.53 seconds as average exposure time. The highest radiation dose and exposure time were recorded at the thoracic level with 3640mGy/cm2 and 46.8 seconds respectively. There were no relationships between the number of implants inserted and the radiation emitted. Instead the exposure time increased the radiation doses emission. Conclusion This study assessed the radiation emission during routine spine procedures. Although radiation exposures per surgery are relatively small, cumulative doses may be deleterious. The surgical team should be aware of short- and long-term risks. Personal protective equipment with radiation dosimeters must be available for every image guided spine procedure. Keywords: radiation emission, spine surgery, vertebral osteosynthesis RESUME L’ostéosynthèse rachidienne est une procédure nécessitant une précision aussi bien dans l’identification des vertèbres, que pour l’insertion des vis pédiculaires. A cet effet, la fluoroscopie est devenue un équipement indispensable au bloc opératoire. Cependant, cet outil d’imagerie est une source de rayons X exposant les patients et l’équipe chirurgicale à un risque élevé d’irradiation. L’objectif de cet article est d’évaluer l’exposition aux rayonnements des chirurgiens du rachis et de discuter des risques associés. Méthode Nous avons réalisé une étude rétrospective allant de Janvier 2012 à Octobre 2013, menée sur 47 interventions chirurgicales du rachis au cours desquelles les doses d’irradiation et le temps d’exposition aux rayonnements ont été enregistrés dans le logiciel interne du fluoroscope. Trois chirurgiens séniors du rachis ont réalisé les chirurgies qui concernaient le rachis cervical (n = 15), le rachis dorsal (n = 5) et le rachis lombaire (n = 27). Les instruments pour la chirurgie provenaient du même fabricant. Résultats La dose d’irradiation moyenne par chirurgie (tous segments inclus) était de 2480,12 mGy / cm2 avec 21,53 secondes comme temps d’exposition moyen. La dose d’irradiation et le temps d’exposition les plus élevés ont été enregistrés au niveau thoracique avec respectivement 3640 mGy / cm2 et 46,8 secondes. Il n’y avait aucune relation entre le nombre d’implants insérés et l’irradiation. Par contre, le temps d’exposition a augmenté les doses d’irradiation. Conclusion Cette étude a évalué l’émission de rayonnements pendant les chirurgies de routine du rachis. Bien que les expositions aux rayonnements par chirurgie soient relativement faibles, les doses cumulées peuvent être délétères. L’équipe chirurgicale doit être consciente des risques à court et à long terme. Un équipement de protection individuelle avec dosimètres à rayonnement doit être disponible pour chaque chirurgie rachidienne guidée par fluoroscopie. Mots-clés : irradiation, chirurgie du rachis, ostéosynthèse vertébrale INTRODUCTION Ionizing radiation is increasingly being used for diagnostic and therapeutic procedures in surgical centers. Its use has expanded exponentially in surgery with the development of modern era techniques. Continuous exposure to low dose radiation may lead to stochastic effects, involving either cancer development in exposed individuals owing to mutation of somatic cells or heritable disease in their offspring owing to mutation of reproductive (germ) cells (18). Findings on these considerable health risks led to a steady reduction of the annual occupational threshold recommendation by the International Commission on Radiological Protection (ICRP) to an effective dose of 20 mSv averaged over 5 years with no single year having more than 50 mSv exposure (12). However, some reports demonstrate increased level of chromosomal abnormalities in medical workers exposed to low dose of radiation within recommended limits (2,20). This is of great concern to spine surgeons, as available data suggests that spine surgery comprises an increasing proportion of neurosurgical practice (3,6). Moreover, compared to other procedures necessitating fluoroscopy, dosimetry readings in spinal surgery are up to 12 times greater than in non-spine procedures (14). A survey by Wagner et al demonstrated that members of the scoliosis research society reported a 12% incidence of cancer. Additionally, they appeared to have a 25-fold higher incidence of thyroid cancers than to the general male population (19). This is especially more alarming in a limited resource setting, where adequate protective measures are not always respected. This was stressed by Mastrangelo et al in a retrospective study they conducted in a small Italian hospital, where radiation protection practice was poor, which revealed a cancer incidence of 29% (9 in 31) in orthopaedic surgeons exposed to medical radiation compared to 4% (7 in 158) in unexposed orthopaedic surgeons (10). To the best of our knowledge, there is no study investigating fluoroscopy related radiation exposure of spine surgeons in West Africa. The aim of this study was to fill this gap in literature, to raise awareness of spine surgeons on the aforementioned risk and discuss the prevention methods. MATERIALS AND METHODS Study design We performed a retrospective analysis of spine surgeries with vertebral osteosynthesis achieved at a single institution namely the Department of Neurosurgery of Yopougon – Abidjan Teaching Hospital. Forty-seven surgeries were performed by 3 senior neurosurgeons from January 2012 to October 2013. These procedures involved 15 cervical cases, 5 lumbar cases and 27 lumbar cases. We hypothesized that the irradiation doses were significantly different per spinal procedures and per surgeons. Moreover, we hypothesized that the irradiation doses increased according to the number of pedicle screws implanted. Dosimetry and data collection From the operative room register, we collected clinical data such as the surgical procedure and number of implants. The implants used came from only one manufacturer. Next, we retrieved radiation data from the software of the C- arm OmniscopStephanix ®. We collected the exposure time (seconds), irradiation doses (milliGray), cumulated doses per spine procedure and per surgeon. The raw clinical data is attached in the supplemental materials. Statistical analysis Statistical analyses and graphics were performed using GraphPad Prism 8.0 software; p<0.05 was considered statistically significant. The results were expressed as the mean +/- standard deviation. Comparisons among spine levels were performed using the analysis of variance ANOVA follow by Tukey’s multiple comparison test for comparison among the different groups. Pearson’s correlation test was used to demonstrate the correlation between radiation dose emission and number pedicle screws implanted. A linear regression test was performed to assess the relationship between the exposure time and the radiation doses emitted. RESULTS Irradiation dose emission Irradiation doses emitted during surgeries were statistically different among the surgeons (p =0.0334, One-way ANOVA). The surgeon 1 had significantly less irradiation per procedure (Figure 1) and was reported to have performed more cervical procedures (Table1). Indeed, the cervical spine procedures had the least radiation doses emitted with a mean dose of 1348 milli-Gray as compared with thoracic and lumbar procedures with 3115 mGy and 2987 mGy respectively (Figure 2a). However, the differences observed were not significative (p=0.07, One-way ANOVA). Exposure time We found a significant difference in exposure time between the vertebral segments (p=0.022, One Way ANOVA). The highest exposure time was encountered in thoracic procedures with a mean time of 46.8 seconds followed by lumbar and cervical segments with 20.92 s and 14.63 s respectively (Figure 2b). On Tukey’s multiple comparison test, there were a significant different between the thoracic and cervical segment (p=0.0167) and between thoracic and lumbar segment (p=0.0498). Relation irradiation dose- exposure time – number of implants To investigate the relationship between irradiation dose- exposure time and number of inserted implants, we performed a linear regression analysis between irradiation dose – exposure time and irradiation dose – number of implants. We found no correlation between the irradiation dose emitted per surgery and number of inserted implants, R=0.1247 (Figure 3a). However, the linear regression test showed a relationship between irradiation dose and exposure time, R2 = 0.6423(Figure 3b). DISCUSSION Spine surgeries are procedures involving accuracy in vertebra identification and implants insertion. For this purpose, image guided surgery is mandated. Fluoroscopy is the most common imaging method used. Although compelling articles investigated the irradiation exposure in the neurosurgical theatre, no studies have been performed in West Africa. Yet, spine surgeries with fixation are the top one procedure in our practice. Hence, this study stands to raise awareness about irradiation exposure and its associated risks among west African neurosurgeons. The radiation data was collected retrospectively. The surgeons were not aware to reduce the Hawthorne effect. Therefore, our data closely reflected the current practice. In this study, we investigated the radiation dose emitted per spinal segment and per surgeon as a proxy for radiation exposure. Indeed, accurate measurement of radiation is done by body dosimeters which express the dose in Sievert. The thoracic level procedures recorded the highest dose. We believed that the ribs and lungs opacities hindered the identification of thoracic vertebra. These findings are similar to those of Bratschitsch et al as they measured high value of radiation on patients thoracic region during fluoroscopy guided procedures (5). However, there is a correlation between body mass index and radiation exposure during fluoroscopy guided spinal surgery (8). This variable was not included in our study. The lumbar procedures were the most common, in accordance with the available evidence in the literature. Perisinakis K et al reported that an average pedicle screw insertion procedure requires 1.2 minutes and 2.1 minutes of fluoroscopic exposure along the anterior-posterior and lateral projection, resulting in a dose area product of 2320 mGy cm2 and 5680 mGy cm2, respectively. This is greater than the irradiation doses observed during this study (13). This may be related to their long exposure time. This finding is further stressed by the statistically significant positive correlation between the exposure time and measured radiation dose we observed. Notwithstanding this, there is a wide variation in reported mean values of fluoroscopic screening time per pedicle screw insertion procedure, ranging from 1min to 6.3min (7,15). This difference may be related to the number of screws per procedure and the technique of fluoroscopy manipulation and screw insertion. Handling the fluoroscope during spine surgery exposes the surgeon to radiation. Though the radiation doses are often less than the annual recommended threshold, it still raises concern as significant health risk has been correlated to lifetime long radiation exposure, with the highest doses in spine surgeries. The organs sensitive to radiation with substantially different susceptibilities include the gonad, bone marrow, breast, cornea, gastrointestinal tract, lung, and thyroid (4). Available evidence suggests that the surgeon’s dominant hand receives the highest radiation dose. This may be because unlike the sensitive organs which receive low intensity scattered radiation, a surgeon’s hand receives additionally direct radiation due to its proximity to the X-ray source during fluoroscopy (5,9). The primary source of radiation dose to a surgeon’s sensitive organs is secondary radiation such as scatter radiation from patients, which depends on parameters like body surface and weight (17). However, scattered radiation doses decrease as distance from the patient increases during the use of C-arm fluoroscopy (5,9,17). Radiation exposure can be decreased by lead protection (3-10,13-15,17,19). Ahn Y et al demonstrated the protective effect of a lead collar and lead apron, reducing radiation dose by 96.9% on thyroid region, and 94.2% on breast and gonad region (1). This was also demonstrated by Synowitz et al, in a study where they assessed radiation exposure of two surgeons who performed the same number of vertebroplasty procedures in 30 patients but differed in their left-hand protection. Their study revealed a significant increase in radiation exposure without protection (17). In some facilities in low- and middle-income countries like those in which this study was conducted, lead shielding to protect the hands, the thyroid and lead glasses for eyes protection are often not available, increasing radiation exposure and decreasing the number of interventions before exceeding the annual occupational exposure limits. Using lead shielding to protect the hands might allow an individual surgeon to perform up to 1000 or more procedures per year within safe limits instead of 300 without protection (17). Also, personal dosimeters for evaluation of radiation doses are not readily available. In this setting, active measures of reducing exposure are mandatory for spine surgeons to reduce the occupational hazard related to fluoroscopy guided spine surgeries. This goal could be achieved by acting on various aspects of fluoroscopy technique, surgical technique and whenever possible predominant use of navigation technology which provides the opportunity of a significant work life dose reduction for the surgeon (5,9,11,16). These methods to minimizing radiation exposure are summarized in table 3. Study limitations: The main limitation of this study was the quantification of radiation method. Due to the study design and the unavailability of dosimeters, we were not able to measure radiation exposure on specific areas on the surgeon and the other operating room personnel (assisting surgeon, anesthesiologist, sterile nurse, radiology technologist). CONCLUSION Spine surgeries assisted by fluoroscopy exposes patients and surgical teams to irradiation. Although irradiation exposures per surgery are relatively small, cumulative doses may be deleterious. The surgical team should be aware of short- and long-term risks. Adequate measures should be taken to reduce radiation exposure, by using effective personal protective equipment with safe fluoroscopy and surgical technique during image guided spine procedures. Conflict of interest None declared
Table1: Surgical procedures and irradiation data per surgeon
Table 2: Method for minimizing radiation exposure
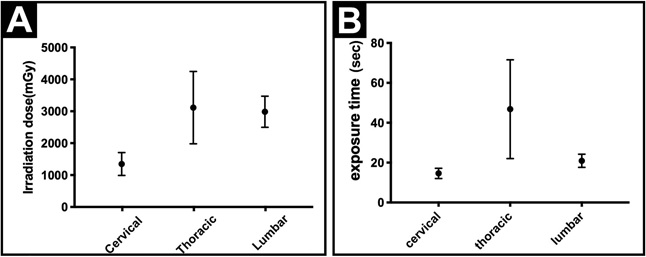 Figure 2: Comparison of irradiation doses per spine procedures
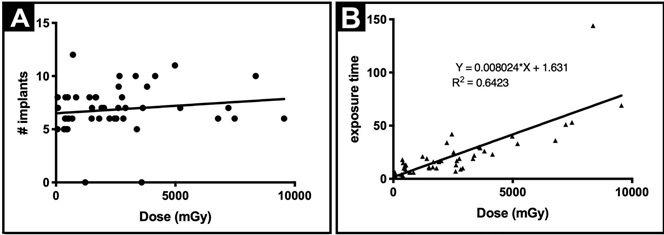 Figure 3: Studies of the association between the radiation doses with the number of implants and the exposure time.
Supplementary data: Summary of the clinical and irradiation data
REFERENCES
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
© 2002-2018 African Journal of Neurological Sciences.
All rights reserved. Terms of use.
Tous droits réservés. Termes d'Utilisation.
ISSN: 1992-2647