|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
CLINICAL STUDIES / ETUDES CLINIQUES
USE OF CLASS ALGORITHM IN MENINGIOMA SURGERY IN HOSPITAL OF MALI.
UTILISATION DE L'ALGORITHME CLASS DANS LA CHIRURGIE DES MENINGIOMES A L'HOPITAL DU MALI.
E-Mail Contact - DIALLO Oumar :
tiecourala2003@yahoo.fr
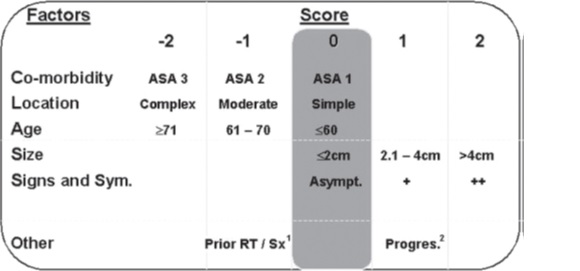
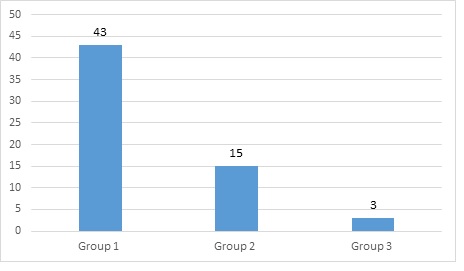
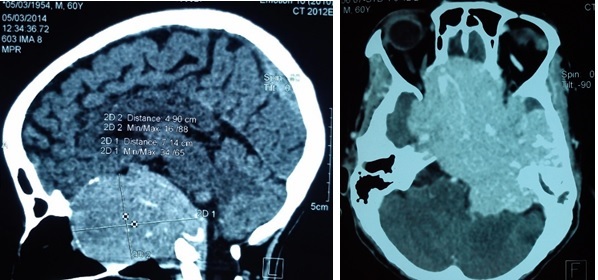
ABSTRACT Background The aim of this study was to assess surgical risk in meningioma surgery using the CLASS scale designed by Joung H. Lee and Burak Sade at Mali Hospital. Method A retrospective study of medical file was performed of all patients operated from intracranial meningioma between 2011 and 2015. We analyzed the surgical outcome using the Glasgow outcome Scale at six weeks. CLASS scale which classified the patient risk at surgery in low, mild and severe according mainly to five criteria: comorbidity, location, age, size, signs and symptoms. Medical and neurological complications were recorded. Results Sixty-one patients were included in this study. Sex distribution was 36 females and 25 males. Mean age was 44.78 years. At six weeks of surgery 77% of patients were good Glasgow Outcome and 23% were bad. We found 16 medical complications in 14 patients and 8 neurological complications in 8 patients. Conclusion The CLASS algorithmic scale is a good mean for patient selection in meningioma surgery because it’s simple, easily reproducible and applicable at all patients independently of age and location of tumor. It may represent a helping tool above all young neurosurgeon. Keywords: Meningioma, CLASS, GOS, Algorithmic, Scale, Prognosis. RESUME Contexte Le but de cette étude était d’évaluer le risque chirurgical dans la chirurgie du méningiome en utilisant l’échelle CLASS conçue par Joung H. Lee et Burak Sade à l’hôpital de Mali. Méthode Une étude rétrospective du dossier médical a été réalisée sur tous les patients opérés d’un méningiome intracrânien entre 2011 et 2015. Nous avons analysé le résultat chirurgical en utilisant l’échelle de résultat de Glasgow à six semaines. L’échelle CLASS qui a classé le risque du patient au moment de l’opération en faible, léger et sévère selon principalement cinq critères : comorbidité, localisation, âge, taille, signes et symptômes. Les complications médicales et neurologiques ont été enregistrées. Résultats Soixante et un patients ont été inclus dans cette étude. La répartition par sexe était de 36 femmes et 25 hommes. L’âge moyen était de 44,78 ans. A six semaines de la chirurgie, 77% des patients avaient un bon résultat de Glasgow et 23% un mauvais. Nous avons trouvé 16 complications médicales chez 14 patients et 8 complications neurologiques chez 8 patients. Conclusion L’échelle algorithmique CLASS est un bon moyen pour la sélection des patients dans la chirurgie des méningiomes car elle est simple, facilement reproductible et applicable à tous les patients indépendamment de l’âge et de la localisation de la tumeur. Elle peut représenter un outil d’aide surtout pour les jeunes neurochirurgiens. Mots-clés : Méningiome, CLASS, GOS, Algorithmique, Échelle, Pronostic. INTRODUCTION The goal of treatment in medicine is that the benefits far outweigh the risks. The risk factors associated with meningioma surgery are: patient’s preoperative comorbidity (C), tumor location (L), patient’s age (A), tumor size (S) and symptoms/signs (S) caused by the tumor. Meningioma surgery is difficult to date in sub-Saharan Africa and surgical results are sometimes very poor, due to the lack of adequate instruments for surgery, anesthesia and radiology. In addition, a history of previous surgery and radiation have been shown to be significant risk factors. Beneficial factors are difficult to quantify, including the natural history of the disease and the possibility of cure when Simpson grade 1 resection is performed with improvement in neurologic signs. This scale simply assesses the risks and benefits of surgery for a patient with meningioma. Many authors have proposed a grading system to standardize the surgical indication for meningioma and are based primarily on weighing the risks and benefits of surgery. Meixensberger et al. reviewed their results for 385 patients with intracranial meningiomas and analyzed the factors influencing the outcome (9). Among the factors known to the surgeon preoperatively, age, preoperative comorbidity assessed by the ASA (American Society of Anesthesiology) score (10). Thus, Arienta et al. introduced a grading system in 1990 to standardize surgical decision making in elderly patients with intracranial meningioma (1); Sacko et al. proposed the SKALE score for meningioma surgery in the ninth decade of life in 2007 (11), Cohen-Inbar proposed the geriatric scoring system (GSS) in 2010 (4), and Magill et al developed a grading scale to evaluate the surgical outcome between two approaches to tuberculum sellae meningioma (8). Which of these grading systems is most appropriate for meningioma surgery in our hospital? We chose the CLASS algorithmic scale by Joung H Lee et al. because of its simplicity of design and applicability for all patient ages and tumor location (6). According to this scale, benefit factors are ranked from 0 to +2, whereas risk factors are ranked from 0 to -2 (Figure 1). The purpose of this study was to assess surgical risk using the CLASS scale in meningioma surgery designed by Joung H. Lee and Burak Sade, in our institution (Mali Hospital). METHOD We retrospectively evaluated the morbidity and mortality of intracranial meningioma surgery in 61 patients who underwent surgery from 2011 to 2015 in the Department of Neurosurgery, Mali Hospital, University of Sciences, Techniques and Technologies of Bamako. Data were obtained from the patients’ medical records and the surgical outcome was assessed using the Glasgow Outcome Scale at six weeks. Data were collected for the following variables: C: Comorbidity, L: Location, A: Age, S: Size, S: Signs and symptoms. Medical and neurological complications were also recorded. According to the CLASS scale, patients were divided into three groups: Group 1: Low risk or CLASS ≥1; Group 2: Mild risk or CLASS between 0 and -1; Group 3: Severe risk or CLASS ≤-2. Other factors such as previous surgery or previous radiotherapy were not considered in our study. Analysis was performed using Epi Info TM 7.2 to compare each group with the prognosis of surgery. Poor outcome was Glasgow Outcome Scale 1 to 3 at six weeks after surgery. RESULTS Sixty-one patients were included in this study. The gender distribution was 36 women (59%) and 25 men (41%). The mean age was 44.78 years (range 17-80 years). A summary of the patients in each group description is given in Figure 2. For surgical risk, we found 70.5% in group 1 (figure 3, figure 4, and figure 5) and the CLASS score was +4 (C: 0, L: 0, A: 0, S: +2, S: +2). For this group the Glasgow Outcome Scale at six weeks was 4. For group 2, it was 24.6%. For group 3, it was 4.9% (Figure 6, Figure 7). The CLASS score was 0 (C: -2, L: -2, A: 0, S: +2, S: +2) and the Glasgow score was 1 (patient died 3 days after the operation). We found 16 medical complications in 14 patients and 8 neurological complications in 8 patients (Table 2). At six weeks after surgery, 77% of the patients had a good Glasgow score and 23% a poor one. The distribution of each group is in table 1. The mortality in our study was 23% for all groups. DISCUSSION We retrospectively applied the CLASS score to assess the surgical outcome of our 61 patients because it is simple, easy to apply and not specific for age or location. In our study we found respectively 70.5% in group 1; 24.6% in group 2 and 4.9% in group 3 while Joung H Lee et al (6) found 51.4% in group 2, 36.3% in group 1 and 12.3% in group 3. This discrepancy may be explained by the fact that our sample size was smaller than that of the authors, our patients were relatively young, and the size of the lesion was very large because of the late diagnosis. We also had more patients in group 1 and group 2 and fewer patients in group 3 like the author. Intracranial meningioma occurs most often in elderly patients, and its risk increases progressively with age (7). However, in sub-Saharan Africa, the sociocultural aspect means that elderly patients do not accept surgery or treatment without radiological examination. The Glasgow scale was first used to evaluate patients with traumatic brain injury (14) and we believe that it is applicable to evaluate patients operated on for meningioma. We had 9.83% poor GOS in group 1, 8.20% in group 2, and 4.91% in group 3. All these patients died, which means our overall mortality was 23%. Joung H Lee et al (6) had 1.8% (2/109) in group 1, 3.9% (6/154) in group 2 and 16.2% (6/37) in group 3. Some authors have reported a significant difference in mortality and morbidity between young and elderly patients after meningioma surgery (2). Ane Konglund et al. reported 3.9% as surgical mortality in this series of 168 patients, whereas the mortality rate in this age group of 80-90 years in the general Norwegian population was 37.2% (13). Boviatsis et al. compared elderly patients with younger patients operated on for intracranial meningioma and found that the mortality rate did not differ significantly in the two groups (6.5% and 4.2%, respectively) (3). Medical complications were 18.60% (8/43) in group 1, 53.33% in group 2, and 0% in group 3 because all patients in this group had died, whereas Joung H Lee et al. found 1.8%, 6.5%, and 10.8%, respectively (6). At the same time, neurological complications were 13.95% (4/43) in group 1, 13.33% (2/15) in group 2 and 0% in group 3, while the same authors found 7.3%, 15.6% and 24.3% respectively. This difference can be explained by the level of technology available to us but also by the overall experience of all the providers. Magill et al. in their series of 139 patients found 22 complications in 20 patients including 7 CSF leaks, 6 infections and 9 other complications (8). Ane Konglund et al (12) reported 13.7% of complications but Sacko et al (11) reported 9.4% in their patients in the 1990s. However, series on meningioma surgery in patients over 65 years of age report complication rates of 17.5% to 54.3% (12,5). CONCLUSION The CLASS algorithmic scale is a good tool for patient selection in meningioma surgery because it is simple, easily reproducible and applicable to all patients regardless of age and tumor location. It can be a useful tool especially for young neurosurgeons. DISCLOSURES The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper. All authors have read and approved the manuscript.
 Figure 3: Example of Group 1 CT scan: preoperative axial view (left), coronal view (middle) and postoperative axial view (right).
Table 1: GOS distribution by group.
GOS = Glasgow Outcome scale
Table 2: Medical and neurological complications.
Table 3: Medical and neurological complications by group
REFERENCES
|
© 2002-2018 African Journal of Neurological Sciences.
All rights reserved. Terms of use.
Tous droits réservés. Termes d'Utilisation.
ISSN: 1992-2647