
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
CLINICAL STUDIES / ETUDES CLINIQUES
EPIDEMIOLOGICAL, CLINICAL PROFILE AND PROGNOSIS OF BRAIN TUMORS IN THE NEUROLOGY DEPARTMENT OF THE UNIVERSITY HOSPITAL POINT «G»
PROFIL ÉPIDÉMIO-CLINIQUE ET PRONOSTIC DES TUMEURS CÉRÉBRALES AU SERVICE DE NEUROLOGIE DE L'HOPITAL UNIVERSITAIRE POINT « G »
E-Mail Contact - COULIBALY Thomas :
coulibalythomas@yahoo.fr
ABSTRACT Objective To determine the frequency and clinical course of intracranial tumors in general and glioma in particular at the University Hospital Point G in Mali. Methods We conducted a prospective study from January 2009 to December 2011 in the Neurology Department of the University Hospital Point “G”. We enrolled patient, regardless of age and sex, suffering from a suspected malignant intracerebral tumor evoked on medical imaging and seen in our neurology outpatient visits. Based on the brain imaging results, patients were classified according to the diagnoses evoked. Results Our patients (n=27) were 42.7 years old on average ranging from 10 to 84 years. The sex ratio was 4 males for one female. Motor deficit was the most frequent reason for outpatient visit in 66.7%. In total, eight (8) had glioblastomas, three (3) had metastases, two (2) had lymphomas, one (1) had an astrocytoma and another had a brainstem glioma, representing 2.2% of our hospital admission rate. The median duration between the onset of symptoms and the outpatient visit was 2.1 months [0.1-14.3]. The median length of survival after the diagnostic was 3.33 months [0.93-17.63]. Therefore, four patients out of five benefited from a symptomatic treatment, 13 passed away and two (2) were lost to follow-up during the study period. Conclusion The prognosis of brain tumors mainly glioblastomas was very poor in our cohort. A concerted effort to stimulate brain tumor research is urgently needed to improve the management of these patients in Mali. Key words: Brain tumors, glioblastoma, prognostic, survival, Bamako, Mali RESUME Objectif Déterminer la fréquence et l’évolution clinique des tumeurs intracrâniennes en général et des gliomes en particulier au CHU Point G au Mali. Méthodes Nous avons mené une étude prospective de janvier 2009 à décembre 2011 dans le service de Neurologie du CHU Point « G ». Nous avons recruté lors des consultations ambulatoires, des patients, tout âge et tout sexe confondu, avec une suspicion de tumeur maligne intracérébrale évoquée à l’imagerie médicale. Les patients ont été classés selon les diagnostics évoqués à l’imagerie cérébrale. Résultats Nos patients (n=27) avaient en moyenne 42,7 ans avec des extrêmes de 10 et 84 ans. Le sex-ratio était de quatre hommes pour une femme. Le déficit moteur était le motif de consultation ambulatoire le plus fréquent dans 66,7 %. Nous avons trouvé huit glioblastomes, trois métastases, deux lymphomes, un astrocytome et un gliome du tronc cérébral soit 2,2% de notre taux d’admission à l’hôpital. La durée médiane entre le début des symptômes et la consultation ambulatoire et celle de survie après le diagnostic étaient respectivement de 2,1 mois [0,1-14,3] et de 3,33 mois [0,93-17,63]. Ainsi, quatre patients sur cinq ont bénéficié d’un traitement symptomatique, 13 sont décédés et deux (2) ont été perdus de vue au cours de la période d’étude. Conclusion Le pronostic des tumeurs cérébrales principalement des glioblastomes était très mauvais dans notre cohorte. Un effort concerté pour alimenter davantage d’enquêtes sur les tumeurs cérébrales est nécessaire et urgent pour améliorer la prise en charge de ces patients au Mali. Mots clés : Tumeurs cérébrales, glioblastome, pronostic, survie, Bamako, Mali. INTRODUCTION Brain tumors compass all intracranial neoformations either intracranial or extra-axial (3) with a wide clinical heterogeneity in terms of location, anatomo-pathological aspect, clinical manifestation and prognostic. The most signs that reveal brain tumors are often headache, seizures, and intracranial hypertension, and cognitive impairment, sensory and motor disorders (17). Anatomo-pathology examination remains the gold standard, but cross-sectional imaging, especially brain CT scan and Magnetic Resonance Imaging (MRI) are the imaging modalities of choice (6,11). In developed countries, brain tumors of the central nervous system (CNS) have benefited from a significant therapeutic and diagnostic progress with new medical imaging techniques and molecular biology. The incidence of brain tumors for patients from all age groups has increased between 1970s and 1990s (9,13). In North America, the increase was 1.1% per year from 1985 and 1999. In France, the estimated incidence of brain tumors from the data of the general registers was 9.5 per 100,000 men (15th among all cancers) and 8.6 per 100,000 women (13th among all cancers) in 2000 (12). In Africa, most studies were carried out in medico-surgical departments and did rarely take into account specifically tumors of the central nervous system as an entity (2,15). The prevalence of brain tumors was 6.3% in Cameroon in 2006 (8), 0.31% in Ghana in 2000 (1) and 2.63% in Mali in 2008 (18). However, the absence of a specialized registry as well as the disparity of the healthcare system make it difficult to carry out these studies in Africa. In order to improve the management of patients with this disease, we decided to conduct this study in order to determine the frequency and prognosis of intracranial tumors in Mali. MATERIAL AND METHODS We conducted a descriptive prospective study in the Neurology department of the Point « G » Hospital from January 2009 to December 2011. We included all patients of all ages suffering from an intracerebral tumor evoked by medical imaging and seen in our neurology outpatient visits. Patients who did not perform brain imaging were not included in this study. A senior neurologist examined each of our patients and we obtained an informed consent from each patient. When the tumor was detected, we ordered other work-ups to identify possible metastasis. Therefore, all of our patients underwent Brain CT, which allowed us to classify the patients based on their diagnostic. We inquired and estimated the time spent between the first symptoms experienced by the patient and the first neurology outpatient visit in our department. The date of the first symptoms was considered in most cases to refer to the day of onset of unusual symptoms such as a seizure, motor deficit, unusual headaches and visual and/or sensory disturbances. We also determined the time between the first symptoms or the diagnostic and the passing away of the patient as a length of survival. In other cases, we took the middle of the year or the closest date to the events for which the patient or parents were referred to the hospital. We analyzed the data using Epi info 2000. We used chi2 and Fischer exact test to compare proportions and set the statistical significance threshold at p<0.05. RESULTS From January 1, 2009 to December 31, 2011, we had 1,230 inpatients in the neurology department of the University hospital Point “G” CHU from our outpatient visits. Among these patients, 27 were diagnosed with brain tumors. Patients were males in 66.7% (18/27) and females in 33.3% (9/27). The average age was 39 years-old with extremes of 10 and 84 years-old. Most patients came from outside Bamako, the capital city (Table I). A motor deficit revealed the brain tumor in 48.1% followed by headaches in 25.9%. Patients benefited from surgery in 11% and from symptomatic treatment in 81.5% (Table II). Patients were diagnosed with glioblastoma in 29.6%, meningioma in 22.2% and metastases in 11.1% (Table III). The median time to survival was 3.1 months with extremes of 0.1 months to 112.2 months and patients diagnosed with glioblastoma had the shortest survival time (Table IV). Among all 27 patients, 22 passed away, three were lost to follow-up and two survived during our study period (Table V). DISCUSSION Despite the significant progress made in the field of scientific research, namely molecular biology, diagnostic imaging, operating techniques and technology, development of adjuvant treatments for tumor pathologies, some brain tumors still have a poor prognostic. In our study, the frequency of brain tumors was 2.2% (27/1,230) (Figure 1). Our observed frequency was lower than that reported by Eyenga et al., 6.3% (231/3,667) (8) Chi2=31.0872 p< 0.00001 and by Keita et al., 5% (27/579) (10) Chi2=8.2808 p=004007. Variations in frequency can be explained by the absence of a specialized registry as well as the disparity of the healthcare system and the study type and design. The median age of our patients was 39 years old (Table 1), a result comparable to that reported by Keita et al., (10) and Eyenga et al., who found a mean age of 40.11 years-old and 40.3 years-old, respectively.In our study, motor deficit was the most common reason for outpatient visit with 48.1% (13/27), which was much higher than that reported by Keita et al., with 40.7% (27/579) (10) Chi2=79.1255 p< 0.00001 (Table 2). Epilepsy was present in 40.7% (11/27) of our patients similar to that reported by Dupont S with 30% (528/1,760) (7) Chi2=1.4564 p=0.227512 to 50% (880/1,760) Chi2=0.9119 p=0.339599. Intracranial hypertension syndrome was in 66.7% (18/27) of our patients. This result was much higher than that reported by Keita et al., with 4.7% (27/579) (Table 2) Chi2=144.2684 p< 0.00001. Glioblastoma represented 29.6% (8/27) of all brain tumor cases including seven men and one woman. Our observed frequency was much lower than that reported by H. Collomb et al. with 51.3% (187/220) (5) Chi2=64.8078 p< 0.00001. Meningiomas were 22.2% (6/27) including five females and one male. Our result was similar to that reported by Eyenga et al., with 24% (880/3667) (8) Chi2=0.0463 p=0.829545, but much lower that reported by Chirimwchirb et al., with 31% (231/297) (4) Chi2=38.8913 p< 0.00001 (Table 3). The overall median and mean time between the onset of symptoms and the first outpatient visit were 3.1 months with the extremes of 0.1 and 112.2 months and 14.57 months, respectively. The overall median survival time was 4.18 months with the extremes of 0.93 and 113.07 months and mean of 15.21 months (Table 4). This result could be explained by the fact that the majority of our patients resided outside Bamako, the capital city where the neurology department is located, but also most of our patients frequented their local community health centers before being referred to the neurology department. Regarding survival, it could be explained by the lack of specific treatment such as surgery, radiotherapy and suitable chemotherapy. Keita et al., have reported an average screening time of 335 ± 19 days with the extremes of 30 and 2,160 days.The median age of patients with glioblastoma was 45.5 years old with the extremes of 40 and 84 years old (Table 5). On average, our patients were younger than those reported by Noël G et al., with 62.1 years old with the extremes of 7 and 82 years old (16) and by Malkoun N et al. with 61 years old with the extremes of 40 and 77 years old (14). This difference could be explained by the fact that the Malian population is younger in general and healthcare is not easily accessible to elderly in Mali. The median time to consultation was 2.6 months and the median time to survival was 3.48 months (Table 5). These delays lasted 68 days on average with the extremes of 3 and 273 days for the appearance of the 1st symptom and the start of non-surgical treatment. A median survival time of 14.3 months reported by Noël G et al., (16). The duration median survival of 12.3 months was reported by Malkoun N et al. (14).Patients with metastases, glioblastomas and lymphomas had the shortest survival times due the malignancy potential and the rapid evolution of these tumors. The limitation of our study was the non-accessibility to more efficient imaging, the non-availability of anatomo-pathological diagnosis and the non-accessibility to certain treatment such as chemotherapy. We also did not focus on the size and the location of the brain tumors since such information is well-described per tumor type (meningioma, glioblastoma, etc…) in the literature. CONCLUSION Brain tumors affected 2.2% of our patients in Mali. Glioblastomas, lymphomas and metastases had the poorest prognostic and the shortest median survival times. Further studies are needed to better characterize these tumors and to improve the current standard of diagnostic and treatment.
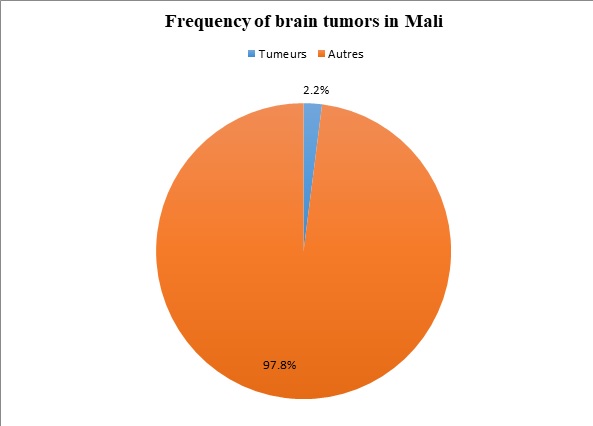 Figure 1. Frequency of brain tumors among all outpatient visits in the department of Neurology at the University Hospital Point G in Bamako, Mali.
Table 1: Socio-economic data of patients with brain tumors in Bamako, Mali.
*The mean age was 39 years old. **Blue collar job (n=1), accountant (n=1), health professional (n=1), student (n=1)
Table 2: Reason for the outpatient visits, clinical presentation and type of treatment of patients in Bamako, Mali.
*Intracranial hypertension syndrome was present n 66.7% (18/27) of our patients.
Table 3: Diagnostic received by patients after the brain CT Scan examination.
Table 4: Mean and median delays between the onset of the symptoms and first outpatient visits as well as the survival time of patients.
Table 5: Gender, average age and outcomes of the follow up per diagnostic for the patients.
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
© 2002-2018 African Journal of Neurological Sciences.
All rights reserved. Terms of use.
Tous droits réservés. Termes d'Utilisation.
ISSN: 1992-2647