REVIEW / MISE AU POINT
FORAMEN MAGNUM MENINGIOMAS: A REPORT OF 10 CASES AND REVIEW OF LITERATURE
LES MENINGIOMES DU TROU OCCIPITAL: A PROPOS DE 10 CAS ET REVUE DE LA LITTERATURE
- Service de Neurochirurgie, Hôpital Ibn Sina, Rabat, Maroc
ABSTRACT
Introduction
Foramen magnum meningiomas are uncommon skull basal meningiomas. Although there has been great development of the anatomical knowledge for this region, several controversies still exist regarding aspects of tumor location, rate of vertebral artery (VA) encasement, rate of tumor recurrence, and surgical approaches. We report a series of patients with foramen magnum meningioma treated in our institution.
Methods
We reviewed 10 consecutive cases of foramen magnum meningioma operated between January 2002 and December 2010 in the neurosurgery department of Avicenne Teaching Hospital.
Results
There were 6 female and 4 male patients (mean age 41.7 ± 6.4 years; range, 32-68 years).
Foramen magnum meningiomas were classified as anterior (1 case), anterolateral (2 cases), and posterolateral (7 cases). Headache and dizziness (90%), and cervico-occipital pain (50%) were the most common presenting symptoms. Eight patients were operated on in the sitting position and 2 patients in the park-bench position due to the presence of a patent foramen ovale. The posterior midline approach was performed in 7 cases, far-lateral approach in 3 cases. Gross total resection was achieved in 70% of patients. Surgical mortality was 0 %.
Conclusion
Foramen magnum meningiomas are challenging tumors in the vicinity of the brainstem, the vertebral artery, and lower cranial nerves. Several surgical approaches are possible, each one with specific indication.
Keywords: Foramen magnum; meningioma; surgical approach.
RESUME
Introduction
Les méningiomes du foramen magnum sont rares. Leur prise en charge chirurgicale dépend du siège, de la taille et de l’extension vers les structures anatomiques de cette région. Nous rapportons une série de patients ayant eu un méningiome du foramen magnum, traités dans notre institution.
Matériel et méthode
Il s’agit d’une étude rétrospective de 2002 à 2010, concernant des patients opérés pour un méningiome du trou occipital.
Résultats
L’âge moyen de la série est de 41,7 ± 6.4 ans avec des extrêmes allant de 32 à 68 ans. Le sex ratio était de 4 hommes pour 6 femmes. La clinique a été dominée par un syndrome d’hypertension intra crânienne (90%) et un syndrome de la charnière cervico-occipitale (90%). Tous les patients ont bénéficié d’un abord chirurgical : sous occipitale médian (7 cas), latéral (3 cas). Huit patients ont été opérés en position assise et 2 en décubitus ventral. L’exérèse chirurgicale a été totale dans 7 cas et subtotale dans 3 cas. L’évolution post opératoire a été satisfaisante, sans complications neurologiques chez 8 patients. Le taux de mortalité est nul pour l’ensemble de cette série.
Conclusion
Les méningiomes du trou occipital constituent un challenge chirurgical pour le neurochirurgien. La voie d’abord doit être choisie en fonction de l’extension de la tumeur.
Mots clés : Trou occipital ; méningiome ; abord chirurgical.
INTRODUCTION
Meningiomas account for 14.3 to 19% of all intracranial tumors and only 1.8 to 3.2% of meningiomas arise at the foramen magnum (FM) level (38, 3). However, meningiomas represent 70% of benign tumors of the FM (11, 12, 13, 15, 33, 40). Because of the complex of anatomy of this area, which includes the brain stem, vertebral artery, and lower cranial nerves, complete resection of FM meningioma is challenging for the neurosurgeons. Despite improved knowledge of the anatomy of this region and development of operative techniques for skull base tumors, controversy still exists regarding the optimal approach for anterior and anterolateral FM meningiomas (5, 6).
This is a retrospective analysis of clinical characteristics and outcomes of surgery, as well as review of literature, in patients with FM meningiomas, at our teaching hospital setting.
PATIENTS AND METHOD
From January 2002 to December 2010, a total of 10 consecutive adult FM meningiomas patients underwent operation at the neurosurgery department of Avicenne Teaching Hospital, Rabat-Morocco.
Neuroimaging Studies
All patients were evaluated preoperatively with computerised tomography and contrast-enhanced magnetic resonance imaging (MRI). In some patients with large tumors, cerebral angiography was used to evaluate the blood supply to the tumor. Encasement and narrowing of the vertebral artery (VA) were assessed using both MRI scans and cerebral angiography. Three main criteria were used for the classification of the FM meningiomas: the compartment involved, dural attachment, and the relation to the VA. The extent of tumor removal was assessed with postoperative MRI.
Surgical Procedure
Patients were operated upon in the sitting position when there was no contraindication. Electrophysiologic monitoring of the lower cranial nerves, somatosensory evoked potentials, and brainstem auditory evoked potentials were used in all operations.
The posterior midline approach was performed for posterolateral FM meningioma; thus, the lower part of the occipital bone and the posterior arch of the atlas were resected and widened on the side of the tumor. For anterior and anterolateral tumors, a far-lateral approach was chosen. The VA was identified and the posterior arch of C1 was resected as far as lateral mass. C2 laminectomy was carried out when necessary to expose the caudal extent of the tumor in the upper cervical spinal canal. The occipital rim to one third of the occipital condyle, especially the medial margin, was drilled away to expose small anterior tumors or those encasing the VA.
Postoperative Management
Patients were sent to the intensive care unit after the operation and endotracheal intubation was continued for at least 12 hours. After surgery, careful assessment of the caudal cranial nerves is paramount to the patient’s successful recovery. Aspiration precautions should be taken before the patient is allowed oral intake, and the diet is advanced gradually from a dysphagia diet to a regular one as indicated. Intensive pulmonary care, aggressive pulmonary toilet, and antibiotic prophylaxis are used to prevent fatal respiratory complications in patients with deficits of the lower cranial nerves. Patients with a deficit of the glossopharyngeal and vagus nerves may need an aggressive tracheostomy to protect the airway and manage secretions, and also may require a gastric tube.
Patients Follow up
Clinical neurological examination and MRI scans were performed at 6 months and 1 year after surgery. Long-term out-patient follow up data were obtained from patients’ files.
RESULTS
Clinical Data
Four patients were 4 males and 6 were females. The ages ranged from 32 to 68 years (mean: 41.7 ± 6.4 years). Preoperative symptoms and neurologic signs are presented in Table 1. Cervico-occipital pain was present in 50% cases, and one patient had any symptom before admission.
Tumor Characteristics and Surgical Aspects
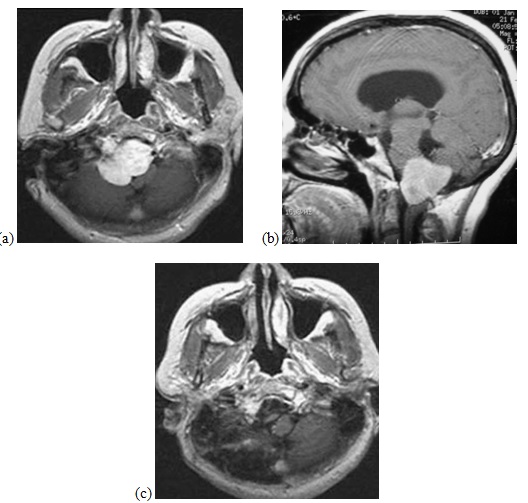
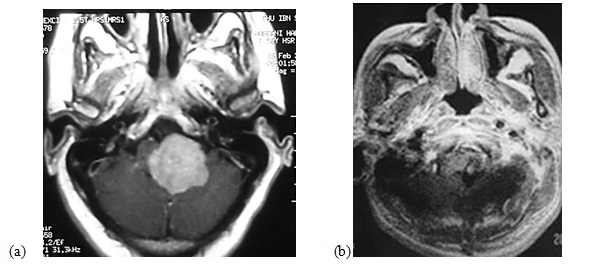
Anterior FM meningioma was found in 1 patient, anterolateral in 2 and posterolateral in 7 (Figures 1, 2). The mean diameter of the tumors on MRI was 3.35 ± 0.85 cm (range, 1.0 to 4.7 cm). The VA was encased in 3 patients. Eight patients were operated upon in the sitting position and 2 in the park-bench position due to the presence of patent foramen ovale. Gross total excision was achieved in all 7 patients who had posterior midline approach (Table 2).
Outcomes
The mean stay in intensive care unit was 2.5 ± 0.5 days and ranged from 1 to 35 days. Postoperative complications included persistent dysphagia, haematoma, pneumonia, cerebrospinal fluid (CSF) leak and hydrocephalus (requiring ventriculoperitoneal shunt). None died.
DISCUSSION
FM meningiomas are relatively rare. Nine of the patients studied presented with motor deficits, lower cranial nerve involvement and intracranial hypertension. The onset of the clinical signs was mainly insidious. In one case the meningioma was a fortuitous discovery after a benign head trauma. FM meningiomas are uncommon skull base meningiomas. Much has been achieved in the understanding of the anatomy of this region, but controversies still exist regarding aspects of tumor location, rates of VA encasement, rate of tumor recurrence, as well as surgical approaches. Table 3 summarizes the high variability of tumor location, rate of VA encasement, rate of tumor recurrence, and surgical approaches. The incidence of anterior FM meningiomas is 12.5 to 100% (3, 22, 28). Studies show that the demarcation between anterior and lateral FM meningiomas is not always clear and, also, posterior FM meningiomas may be included with anterior or antero lateral lesions in 2.5 to 50% (4-7, 16, 24, 29, 30, 36). The rate of VA encasement may be higher than 59% and the rate of tumor recurrence up to 80% (17, 35). In our series this encasement was present in 3 cases.
Operations for FM meningiomas may be carried out in the sitting or lateral oblique positions (20, 26, 37). Our patients were operated on in the sitting position. This position has the advantage of decompressing the neuraxis upon opening of the posterior bone and dura (14). The disadvantage of this position is risk of air embolism in the sitting position unlike in the lateral oblique position (39). FM meningiomas are undoubtedly challenging tumors, requiring special considerations because of they are located in the vicinity of the brainstem, lower cranial nerves, and VA. Several approaches have been advocated. The goals of surgery include maximizing tumor resection with the minimum morbidity. This is attained by choosing the appropriate approach to allow adequate control of important neurovascular structures, without unnecessary risks (8).
The posterior approach is the best option for posterior FM meningiomas; it is associated with a low morbidity. All patients with posterior FM meningiomas, in our series, had posterior approach.
For lateral and anterior FM meningiomas, the transoral approach has been several drawbacks, especially for intradural lesions, including cerebro-spinal fluid fistula and meningitis (8, 10, 27). The two main surgical approaches reported in the literature are the far-lateral approach (also called posterolateral approach or lateral suboccipital approach), and the extreme-lateral approach (also named anterolateral approach) (23). Both approaches permit drilling of the occipital condyle but provide a different exposure because of the differences in the approach direction.
Another confusing aspect concerns the resection of the occipital condyle for anterior and anterolateral FM meningiomas (1, 8, 11, 21, 29). Arnautovic reported that drilling of the condyle is important for safe and radical tumor resection of anterior FM meningiomas via a transcondylar approach (3). None of the patients in our study had the transcondylar approach. Factors which may increase morbidity include anterior tumor location, tumor size (smaller lesions are more difficult to resect because the surgical corridor is small), tumor invasiveness, extradural extension, VA encasement, absence of arachnoid sheath, and adherences in recurrent lesions (4, 5, 11, 14, 18, 33, 35, 40).
Factors limiting the completeness of resection are adherences to vital structures, VA encasement and invasiveness of the lesion. In our series, the resection was limited by VA artery in one case, and existence of adherence in two cases. In our series, there was subtotal resection in 30%. This rate is comparable to Samii’s and Salas’ series (Table 3). In surgical series in which a high rate of recurrent tumors are included, Simpson grade 1 resection is achieved in 60-75% (3, 33, 35).
The rate of complications in the treatment of foramen magnum meningiomas is relatively high, and it is higher for anterior tumors than for posterior ones (3). Complications rate in anterior tumors in our series is 57.14%. Morbidity ensues primarily from deficits of lower cranial nerves, specifically the glossopharyngeal, the vagus, and the hypoglossal. Such complications may lead to aspiration pneumonia as seen in one of our patients. Other important complications are leakage of cerebrospinal fluid and meningitis. In cerebrospinal fluid leak, additional stitches and compressive dressing, and external lumbar drainage may be used. If the leak persists, operative revision may be indicated. In hydrocephalus, a ventriculoperitoneal shunt is indicated as performed in one of our patients (39). Paralysis of the vocal cords early in the postoperative course may be treated by vocal cord medialization, or the cord can be injected with Gelfoam or Teflon. Such treatment protects the airway until the nerve recovers or the patient learns to compensate for the deficit, which may take up to 8 months (3).
It is more difficult to resect recurrent FM meningioma after incomplete resection in the first operation (39). None of the 3 cases in our series with subtotal resection had been reoperated. They had radiotherapy after the first surgery. The tumor remnants always involved important structures that might increase risk of complications after radiotherapy.
Follow-up data were available for all patients, with a mean follow-up of 90.5 ± 8.3 months (range, 1-120 months). There was no mortality in our series.
CONCLUSION
FM meningiomas are challenging tumors in the vicinity of the brainstem, the VA, and lower cranial nerves. Several surgical approaches are possible, each one with specific indications. Postoperative complications can be dramatic and must be anticipated.
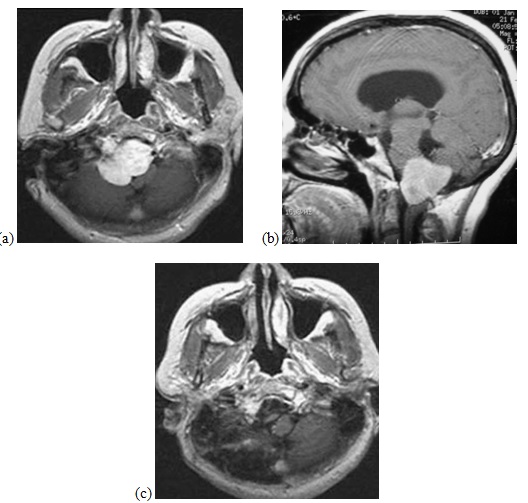
Figure 1 a-c
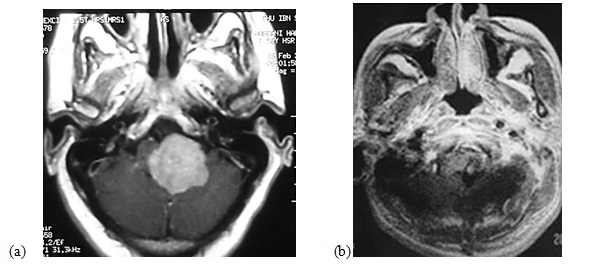
Figure 2
Table 1: Preoperative clinical features in patients with FM meningioma.
| |
Number of patients |
| Asymptomatic |
1 |
| Cervico-occipital pain |
5 |
| Headache and dizziness |
9 |
| Dysphagia |
1 |
| Hoarseness |
2 |
| Paraparesis |
5 |
| Ataxic gait |
5 |
| Hypoaesthesia |
2 |
Table 2: Operative approach and results in patients with FM meningioma.
| |
Anterior |
Anterolateral |
Posterolateral |
| Approach : |
|
|
|
| Posterior midline |
0 |
0 |
7 |
| Far-lateral |
1 |
2 |
0 |
| Degree of resection : |
|
|
|
| Simpson 1 |
0 |
0 |
1 |
| Simpson 2 |
0 |
2 |
4 |
| Simpson 3 |
1 |
0 |
2 |
| Complication : |
|
|
|
| Dysphagia |
1 |
0 |
0 |
| Dyspnea |
0 |
0 |
1 |
| CSF leak |
0 |
0 |
1 |
| Hematoma (tumor bed) |
0 |
1 |
1 |
| Pneumonia |
1 |
0 |
0 |
| Hydrocephalus |
1 |
0 |
0 |
| Mortality |
0 |
0 |
0 |
Table 3: Review ofthe literature of published series of FM meningiomas.
| |
Year |
Nb |
|
FM meningioma location (%) |
|
Recurrence |
VA |
Approach |
Resection % |
|
Permanent |
Mortality |
|
|
Pt |
Anterior |
Lateral |
Posterior |
(%) |
encasement (%) |
|
Total |
Subtotal |
morbidity (%) |
(%) |
| Gilsbach (16) |
1987 |
5 |
|
100 |
|
– |
– |
FL |
100 |
0 |
20 |
0 |
| Guidetti (18) |
1988 |
17 |
82.4 |
|
|
– |
– |
|
100 |
0 |
12 |
11 |
| Sen,Sekhar (35) |
1990 |
5 |
80 |
|
20 |
80 |
– |
EL |
60 |
40 |
60 |
20 |
| Crockard (10) |
1991 |
3 |
100 |
|
|
33 |
33 |
TO |
0 |
66 |
100 |
66 |
| Kratimenos (22) |
1993 |
8 |
100 |
|
|
12.5 |
– |
FL |
87.5 |
12.5 |
0 |
25 |
| Babu (4) |
1994 |
9 |
|
100 |
|
– |
– |
EL |
88.8 |
11.2 |
56 |
11.1 |
| Akalan (2) |
1994 |
8 |
12.5 |
|
87.5 |
– |
– |
PM |
100 |
0 |
0 |
0 |
| Bertanlaffy (6) |
1996 |
19 |
|
100 |
|
– |
– |
FL SO TC |
100 |
0 |
0 |
0 |
| Samii (33) |
1996 |
38 |
|
95 |
5 |
5 |
40 |
PM, LSO |
63.0 |
30 |
5 |
6 |
| George (14) |
1997 |
40 |
45 |
52.5 |
2.5 |
– |
38 |
– |
87.5 |
10.0 |
0 |
7.5 |
| Pirotte (30) |
1998 |
6 |
|
100 |
|
– |
– |
– |
100 |
0 |
17 |
17 |
| Sharma (36) |
1999 |
10 |
50 |
|
50 |
– |
– |
PM, FL |
100 |
0 |
– |
15 |
| Salas (32) |
1999 |
24 |
|
100 |
|
– |
– |
TC/ELJT |
66 |
33 |
– |
0 |
| Arnautovic (3) |
2000 |
18 |
100 |
|
|
11.1 |
– |
TC |
75 |
12.5 |
11.1 |
16.6 |
| Roberti (31) |
2001 |
21 |
|
|
|
– |
– |
EL TC |
76 |
24 |
21.5 |
9.5 |
| Goel (17) |
2001 |
17 |
|
100 |
|
– |
59 |
SO |
82 |
18 |
6 |
0 |
| Nanda (28) |
2002 |
6 |
100 |
|
|
– |
– |
FL |
100 |
0 |
0 |
0 |
| Marin Sanabria (25) |
2002 |
7 |
|
72.5 |
|
– |
– |
TO, SO, TC |
100 |
0 |
5 |
14 |
| Boulton (7) |
2003 |
10 |
60 |
10 |
30 |
– |
– |
– |
90 |
10 |
10 |
0 |
| Pamir (29) |
2004 |
22 |
|
91 |
9 |
– |
40 |
– |
95.5 |
4.5 |
4.5 |
0 |
| Margalit (24) |
2005 |
18 |
|
100 |
|
– |
– |
Lat |
– |
– |
– |
0 |
| Bassiouni (5) |
2006 |
25 |
32 |
57 |
11 |
4 |
43 |
FL |
96 |
4 |
8 |
4 |
| Wu Z (39) |
2009 |
114 |
80 |
24 |
10 |
– |
– |
PM, FL |
86 |
14 |
– |
1,8 |
| Our series |
|
10 |
|
30 |
70 |
0 |
3 |
PM, FL |
70 |
30 |
10 |
0 |
EL externe lateral, FL far lateral/ potero lateral, JT jugular tubercule, mast mastoidectomy, Lat lateral, LSO lateral suboccipital Nb number, PM posterior midline, pt patient, SO suboccipital, TC transcondylar, TO trans oral.
REFERENCES
- ABE H. Surgical technic of the foramen magnum tumors. No Shinkei Geka. 1983; 11(4):353-8.
- AKALAN N, SECKIN H, KILIC C, OZGEN T. Benign extramedullary tumors in the foramen magnum region. Clin Neurol Neurosurg. 1994; 96(4):284-289.
- ARNAUTOVIC KI, AL-MEFTY O, HUSAIN M. Ventral foramen magnum meningiomas. J Neurosurg. 2000; 92(Suppl 1):71-80.
- BABU RP, SEKHAR LN, WRIGHT DC. Extreme lateral transcondylar approach: technical improvements and lessons learned. J Neurosurg. 1994; 81:49-59.
- BASSIOUNI H, NTOUKAS V, ASGARI S, SANDALCIOGLU EI, STOLKE D, SEIFERT V. Foramen magnum meningiomas.: clinical outcome after microsurgical resection via a posterolateral suboccipital retrocondylar approach. Neurosurgery. 2006;59:1177-1187.
- BERTALANFFY H, GILSBACH JM, MAYFRANK L, KLEIN HM, KAWASE T, SEEGER W. Microsurgical management of ventral and ventrolateral foramen magnum meningiomas. Acta Neurochir Suppl. 1996;65:82-85.
- BOULTON MR, CUSIMANO MD. Foramen magnum meningiomas: concepts, classifications and nuances. Neurosurg Focus. 2003;14(6):10.
- BRUNEAU M, GEORGE B. Foramen magnum meningiomas: detailed surgical approaches and technical aspects at Lariboisière Hospital and review of the literature. Neurosurg Rev. 2008;31(1):19-32.
- COHEN L. Tumors in the region of the foramen magnum. In: Vinken PJ, Bruyn GW (eds) Handbook of clinical neurology. North Holland, Amsterdam, 1975;719-729.
- CROCKARD HA, SEN CN. The transoral approach for the management of intradural lesions at the craniocervical junction: review of 7 cases. Neurosurgery. 1991;28:88-98.
- GEORGE B, DEMATONS C, COPHIGNON J. Lateral approach to the anterior portion of the foramen magnum. Surg Neurol. 1988;29:484-490.
- GEORGE B. Meningiomas of the foramen magnum. In: Schmidek HH (ed) Meningiomas and their surgical management. Saunders, Philadelphia, 1991;459-470.
- GEORGE B, LOT G. Foramen magnum meningiomas. A review from personal experience of 37 cases and from a cooperative study of 106 cases. Neurosurg Quat. 1995;5:149-167.
- GEORGE B, LOT G, BOISSONNET H. Meningioma of the foramen magnum: a series of 40 cases. Surg Neurol. 1997;47:371-379.
- GEORGE B, LOT G. Surgical approaches to the foramen magnum. In: Robertson JT, Coakham HB, Robertson JH (eds) Cranial base surgery. Churchill Livingstone, New York, 2000;259-279.
- GILSBACH JM, EGGERT HR, SEEGER W. The dorsolateral approach in ventrolateral craniospinal lesions. In: Voth D, von Goethe JW (eds) Diseases in the cranio-cervical junction. Walter de Gruyter, Berlin. 1987;359-364.
- GOEL A, NITTA J, KOBAYASHI S. Supracondylar infrajugular bulb keyhole approach to anterior medullary lesions. In: Kobayashi S, Goel A, Hongo K (eds) Neurosurgery of complex tumors and vascular lesions. Churchill Livingstone, New York, 1997;201-203.
- GUIDETTI B, SPALLONE A. Benign extramedullary tumors of the foramen magnum. Adv Tech Stand Neurosurg. 1988;16:83-120
- IBRAHIM AW, SATTI MB, IBRAHIM EM. Extraspinal meningioma. Case report. J Neurosurg. 1986;64:328-330.
- KENNING TJ, KANWAR VS, QIAN J. A de novo desmoid tumor of the surgical site following foramen magnum meningioma resection in a patient with Gardner’s syndrome: a case report and review of the literature. J Neurooncol. 2009;107-111.
- KIM KS, WEINBERG PE. Foramen magnum meningioma. Surg Neurol. 1982;17(4):287-289.
- KRATIMENOS GP, CROCKARD HA. The far lateral approach for ventrally placed foramen magnum and upper cervical spine tumours. Br J Neurosurg. 1993;7(2):129-140.
- LANZINO G, PAOLINI S, SPETZLER RF. Far-lateral approach to the craniocervical junction. Neurosurgery. 2005;57:367-371.
- MARGALIT NS, LESSER JB, SINGER M, SEN C. Lateral approach to anterolateral tumors at the foramen magnum: factors determining surgical procedure. Neurosurgery. 2005;56:324-336.
- MARIN SANABRIA EA, EHARA K, TAMAKI N. Surgical experience with skull base approaches for foramen magnum meningioma. Neurol Med Chir (Tokyo). 2002;42:472-480.
- MENEZES AH. Surgical approaches: postoperative care and complications: posterolateral-far lateral transcondylar approach to the ventral foramen magnum and upper cervical spinal canal. Childs Nerv Syst. 2008;24(10):1203-7.
- MILLER E, CROCKARD HA. Transoral transclival removal of anteriorly placed meningiomas at the foramen magnum. Neurosurgery. 1987;20:966-968.
- NANDA A, VINCENT DA, VANNEMREDDY PSSV, BASKAYA MK, CHANDA A. Far-lateral approach to intradural lesions of the foramen magnum without resection of the occipital condyle. J Neurosurg. 2002;96:302-309.
- PAMIR MN, KILIC T, OZDUMAN K, TURE U. Experience of a single institution treating foramen magnum meningiomas. J Clin Neuroscience. 2004;11(8):863-867.
- PIROTTE B, DAVID P, NOTERMAN J, BROTCHI J. Lower clivus and foramen magnum anterolateral meningiomas: surgical strategy. Neurol Res. 1998;20:577-584.
- ROBERTI F, SEKHAR LN, KALAVAKONDA C, WRIGHT DC. POSTERIOR fossa meningiomas: surgical experience in 161 cases. Surg Neurol. 2001;56:8-21.
- SALAS E, SEKHAR LN, ZIYAL IM, CAPUTY AJ, WRIGHT DC. Variations of the extreme-lateral craniocervical approach: anatomical study and clinical analysis of 69 patients. J Neurosurg Spine. 1999;90(2):206-219.
- SAMII M, KLEKAMP J, CARWALHO G. Surgical results for meningioma of the craniocervical junction. Neurosurgery. 1996;39:1086-1094.
- SARTOR K, FLIEDNER E, PFINGST E. Angiographic demonstration of cervical extradural meningioma. Neuroradiology. 1977;14:147-149.
- SEN CN, SEKHAR LN. An extreme lateral approach to intradural lesions of the cervical spine and foramen magnum. Neurosurgery. 1990;27:197-204.
- SHARMA BS, GUPTA SK, KHOSLA VK, MATHURIYA SN, KHANDELWAL N, PATHAK A et al. Midline and far lateral approaches to foramen magnum lesions. Neurol India. 1999;47:268-271.
- TSAO GJ, TSANG MW, MOBLEY BC, CHENG WW. Foramen magnum meningioma: dysphagia of atypical etiology. J Gen Intern Med. 2008;23(2):206-209.
- WARA WM, SHELINE GE, NEWMAN H, TOWNSEND JJ, BOLDREY EB. Radiation therapy of meningiomas. Am J Roentgenol. Radium Ther Nucl Med. 1975;123:453-458.
- WU Z, HAO S, ZHANG J, ZHANG L, JIA G, TANG J, XIAO X, WANG L, WANG Z. Foramen magnum meningiomas: experiences in 114 patients at a single institute over 15 years. Surg Neurol. 2009;72:376-382.
- YASARGIL MG, MORTARA RW, CURCIC M. Meningiomas of basal posterior fossa. In: Krayenbuhl U (ed) Advances and technical standards in neurosurgery, vol. 7. Springer, Berlin. 1980,3-115.