CLINICAL STUDIES / ETUDES CLINIQUES
MIGRATING RETAINED INTRACRANIAL MISSILES
- Division of Neurosurgery, Groote Schuur Hospital, University of Cape Town, South Africa
E-Mail Contact - BUWEMBO J. D. :
SUMMARY
Five cases of retained, migrating intracranial bullets are presented. The bullet migrated transventricularly in four patients and subdurally in one. In five cases the bullets were safely removed: via craniotomy for the four patients with an intraventricular location and through a borehole for the patient with a subcortical location. One patient presented a year after injury with severe headache, due to the bullet having become a third ventricular foreign body. The difficulties experienced in localising the missile using computerised tomography (CT) due to metallic artefact and the usefulness of air encephalography in one of the cases, are demonstrated. Intra-operative localisation using an image intensifier prior to siting the craniotomy, is essential.
RESUME
Cinq observations de projectiles a migration intracranienne sont rapportees. Les bailes ont migre a travers les ventricules chez quatre patients et en region sous-durale chez le cinquieme. Les 4 balles ayant une localization intraventriculaire ont ete retirees par craniotomie ete travers un trou de trepan pour la balle a localization durale. Un des patients se presenta un an apres le traumatisme avec des cephalees intenses, en raison de la localization du projectile dans le troisieme ventricule. Les difficutes de localization du projectile par tomodensitometrie a cause des artefacts metalliques, et l’utilite de l’encephalographie gazeuse dans un cas, sont soulignees. La localization precise preoperatoire par amplificateur de brillance est essentille avant de realiser la craniotomy.
Keywords : Gunshot wound, craniocerebral wound, intracranial body, retained intracranial missile, migrating missile
INTRODUCTION
Migration of retained intracranial missiles is an uncommon occurrence although a number of patient showing this phenomenon have been reported, especially during the major military conflicts in the last 80 years [1,2,3,4,5,6,7,8]. Krause was probably the first to describe this feature of a retained intracranial missile in 1909 [8]. Vilvandre and Morgan (1916) were the first to demonstrate the movement of intracranial metallic foreign bodies radiographically in two patient.[9]
As a brain abscess may result from indriven bone fragments and other retained foreign bodies, the removal of readily accessible foreign bodies has received most attention, [10,11,12,13].
Wood summarised the diagnostic implications of change in position of retained intracranial metallic foreign bodies and indicated that migration could only occur ^4 when a brain abscess or brain softening would allow a metal fragment to change position, as would an intraventricular or a subdural location.
Between March 1991 and October 1993, five patients with migrating retained intracranial missiles were treated in the Department of Neurosurgery, Groote Schuur Hospital. The unusual occurrence of this phenomenon as well as the safety and usefulness of surgical removal of the retained missiles, have prompted us to publish these cases with a review of the relevant literature.
MATERIAL AND METHOD
The first patient was referred from Namibia to our neurosurgical unit for definitive management. The other four patients came from the suburbs of Cape Town and were treated primarily at our unit. All were injured in interpersonal conflict (See Table 1).
TABLE 1 : Demographic and Ballistic Characteristics
| Case No. |
Age |
Sex |
Weapon |
Character of Missile |
| 1 |
33 yrs |
M |
Pistol |
Ricocheting bullet |
| 2 |
21 yrs |
M |
Handgun |
Not specified |
| 3 |
15 yrs |
M |
Homemade gun |
Not Specified |
| 4 |
30 yrs |
M |
Unknown |
Stray bullet |
CLINICAL FEATURES
These are summarised in Table 2:
TABLE 2 : Clinical Features
| Case No. |
Entry Wound |
Initial Site of Missile |
Final Site of Missile |
Anatomical Pathology & Signs |
Initial GCS |
Neurol Symptoms |
| 1 |
Left orbit |
R frontal lobe Parafalcine |
occipital pole, R lateral Ventricle |
Fracture base skull frontal base contusion |
E4V5M6 |
CSF rhinorrhoea / Headache / blind L eye |
| 2 |
Left Occip. |
R fronto-pariental (Fig.1a) |
Third ventricle (Figs.1b,2,3) |
R hemis. lacer. & L occip.lacer. |
E4V2M5 |
CORTICAL blindness L hemi. Epilepsy Headache raised ICP |
| 3 |
Forehead to left of midline |
Midline 5cm posterior to crista galli |
Paramedian at occip. horn of R lateral ventricle |
Frontal lacer. |
E4V5M6 |
L homonymous hemianopia |
| 4 |
R frontal |
R frontal lobe |
Third ventricle |
Frontal fracture Frontal lobe lacer. |
E4V5M6 |
Headache |
Abbreviations:
R = Right, Hemis = Hemisphere, Hemi = Hemiparesis, GCS = Glasgow Coma Scale, L = Left Lacer = Laceration, CSF = Cerebrospinal fluid, Occip = Occipital
All the patients had an entrance – but no exit wounds and all were investigated with plain x-rays and CT scanning. Case 2 underwent pneumo-encephalography as the CT scan image had too much artefact from the bullet to allow accurate anatomical localisation of the missile ( Figures 1b & 3). In four patients the missiles traversed the ventricle in their course. In Case 5 the bullet migrated subdurally. Debridement of the entry would and’ dural repair were done, immediately following admission, but no attempt was made at the initial procedure to remove the deep-seated missiles. Case 1 had formal anterior cranial fossa repair to control a copious CSF rhinorrhoea as part of the preliminary procedure.
MANAGEMENT
Patient No 1 had an initial closure of the post-traumatic CSF fistula causing intense CSF rhinorrhoea. For surgical Procedures see Table 3.
TABLE 3 : Definitive Surgical Procedures, Intra-Operative Findings and Injury Surgery Interval
| Case No. |
Definitive Surgical Procedure |
Intra-operative Findings |
Interval between Injury and Missile Removal |
| 1 |
Parieto-occipital Craniotomy |
Coppery discoloration of the choroid plexus which was wrapped around the bullet |
3 weeks |
| 2 |
Transcallosal approach to third ventricle |
Right thalamic atrophy with enlarged foramen of Munro |
12 months |
| 3 |
Right parieto occipital Craniotomy |
Sterile yellowish fluid around bullet |
3 weeks |
| 4 |
Right frontal craniotomy Interhemispheric |
Bullet in third ventricle |
3 weeks |
In all cases the image intensifier was used to locate the bullet’s position after head had been positioned, prior to siting the craniotomy. [15]
In Case 5, skull x-rays which were obtained after the head had been positioned on the operating table, showed that the bullet had not moved from its previous position as had been shown on plain x-rays and CT of the head, and the burrhole was sited accordingly.
Intra-operatively, direct vision was possible in three cases, palpation was used in one case and a metallic probe was helpful in another case. The bullets were safely removed in all five patients.
The postoperative course of our five patients was good, No neurological deficits were seen as a result of the surgery, except for minor right parietal lobe dysfunction in Case 1.
DISCUSSION
Our five patients suffered civilian gunshot wounds which may be important as regards the kind of weapon and ammunition used. Three of the five cases had no impairment of the level of consciousness and this can be ascribed to the relatively low velocity of the bullet. One missile was from a homemade gun. The ricocheting bullet had obviously spent most of its energy before entering the skull. Case 2, whose level of consciousness was impaired, was noted to have extensive hemisphere damage associated with diffuse brain swelling. Case 5 had only a transient loss of consciousness of less than five minutes.
Migration is possible because of gravitational force acting on the bullet which is significantly denser than the surrounding medium, in this case softened brain and cerebrospinal fluid. The effect of gravity is clearly demonstrated by the patients with the third ventricular bullet. For subdural and parenchymal migration to occur, the intracranial pressure must be normal or low because raised pressure impairs the bullet’s movement by compressing the potential pathway.
Transventricular migration can, however, still occur in the presence of raised intracranial pressure, provided that the ventricles are dilated.
Early migration may occur with brain laceration or cavitation or a location near – or in the ventricle or subdural space.[16] Migration via a white matter tract by a streamlined, intact bullet can also occur early.[17] Late change in the retained missile’s position should signal the possibility of abscess formation but the range of movement in this instance is small, usually no more than rotation.[19] Missile migration does not mean infection as has been thought before.
RADIOLOGY
Plain skull x-rays are useful in demonstrating change in position, but are not sufficient for accurately localising the anatomical site for the purpose of operation. Immediate preoperative localisation is important for safe removal and an image intensifier is helpful in locating the bullet after the head has been positioned, prior to siting the craniotomy.
CT scanning makes accurate localisation of position difficult because the bullet creates a metallic « scatter ». When the nature of the metallic foreign body is unknown, it is unsafe to perform Magnetic Resonance Imaging (MRI) since this can result in harmful migration of in vivo ferro magnetic object. [19] In case 2 where the bullet was located in the third ventricle, accurate localisation of position was achieved using air encephalography. This procedure, which is only rarely indicated since the advent of CT and MRI, may be of diagnostic value in some patients.

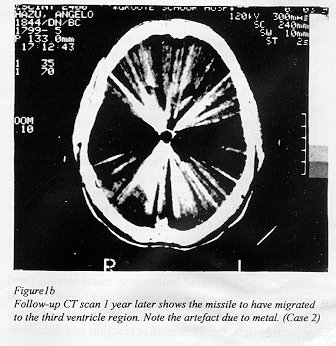
Figure 1b

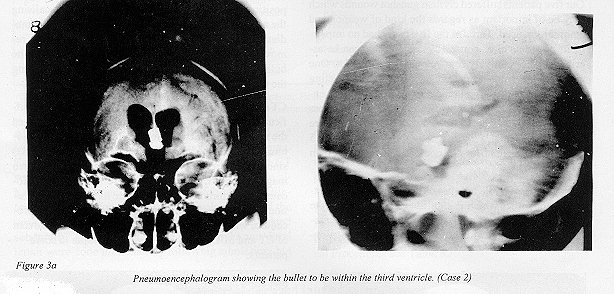
Figure 3a
SURGERY
Removal of intracranial metallic foreign bodies is indicated for several reasons. The possibility of a brain abscess developing makes the removal of the foreign body imperative. A brain abscess has been known to occur as late as 30 years after injury in relation to a deep-seated retained metallic fragment. This should underscore the importance of adequate follow-up. [20]
The location of the bullet in the ventricle may cause acute obstructive hydrocephalus and precipitate an emergency situation and to obviate this, it is safer to remove the bullet electively. Our patient with a bullet in the third ventricle presented with headache and was also shown to have moderate hydrocephalus: both of which resolved after bullet removal.
Copper or nickel plated bullets may cause intense focal inflammation, resulting in necrosis and liquefaction of the surrounding brain which necessitates early removal of such bullets, [21,22]. This intense reaction and discoloration was demonstrated in our first patient within three weeks following injury.
The removal of intracranial missiles via craniotomy is a standard procedure [1,2,3,4,5] and our four cases confirm this. Slow centrifugation of a patient with an intraventricular bullet can cause it to marginalise and to « stick » sub- ependymally, so that its migration stops and it can be removed at craniotomy, [23].
Burrhole removal is possible for a missile that has migrated to a subdural or subcortical location but this requires precise localisation of the missile position. This was achieved in Case 5. Successful stereotactic removal of a small intracerebral pellet was reported by Sugita et al, but this method requires a foreign body which has become fixed,[24].
Ventriculoscopy has been used successfully to remove intraventricular foreign bodies in a number of cases, [25,3].
BIBLIOGRAPHY
- CAMPBELL WP, HOWARD WO, WEARY WB, Gunshot wounds of the brain. Report of two unusual complications: bifrontal pneumocephalus and a loose bullet in the lateral ventricle. Arcch Surg 1942; 44: 789-798.
- CHARLES W, STERNBERGH A, CLARK W, CLARK K. Bullet within the fourth ventricle. J Neurosurg- 1971; 34: 805-807.
- DESCHAMPS GT, MORAN JU. IntracraniaI bullet migration – a sign of brain abscess: Case report. J Trauma 1991; 31: 293-295.
- FURLOW LT, BENDER MB, TEUBER HL. Movable foreign body within the cerebral ventricle. J Neurosurg 1947; 4: 380-386.
- GREENWOOD J. Removal of foreign body (bullet) from the third ventricle. J Neurosurg 1950; 7: 169-172.
- JEFFERSON G. Removal of a rifle bullet from the right lobe of the cerebellum; illustrating the spontaneous movement of a bullet in the brain. Brit J Surg 1918, 5 422-424.
- SMALL JM. Retained intraventricular foreign body. Brit J Surg 1945, 32: 414-418.
- KRAUSE F. Surgery of the brain and spinal cord, 1911; vol. 2:640.
- VILVANDRE G. MORGAN JD. Movements of foreign bodies in the brain. Arch Radiol Electrother 1916: 21: 22-27.
- CAREY M E, YOUNG H, MATHIS JL, FORSYTHE J. A bacteriological study of craniocerebral missile wounds from Vietnam. J. Neurosurg 1971:34: 145-155.
- HAGAN W M. Early complications following penetrating wounds of the brain. J Neurosurg 1971: 132-141.
- HAMMON WM. Analysis of 2187 consecutive penetrating wounds of the brain from Vietnam. J. Neurosurg 1971; 34: 127-131.
- HAMMON WM. Retained intracranial bone fragments: analysis of 42 patients. J.Neurosurg 1971 ;34: 142-144.
- WOOD EH. Diagnostic significance of change in position of metallic foreign bodies in brain abscess. Am J. Roentgenol 1948, 59: 52-58.
- TAARNHOJ P. Gravity instrumental in removing an intracerebral missile. J Neurosurg 1962, 19: 351-352
- BROWN LJ. Unusual pneumoencephalogram following fragment would of the brain. J Neurosurg 1970; 32: 100-102.
- RENGARCHY S. CAREY M, TEMPLER J. The Sinking Bullet. J Neurosurg 1992; 30: 291-294.
- THOMAS GD JR, MORANO JU. Intracranial bullet migration. S sign of brain abscess – case report. Trauma 1991; 31 (2): 293-295.
- POMERANTZ SJ. Craniospinal Magnetic Resonance Imaging, Chapter 3, Saunders & Co, 1989; 47-70.
- DREW JH, FAGER CA. Delayed brain abscess in relation to retained intracranial foreign bodies . J. Neurosurg 1954; 11:3 86-393
- OTT K, TARLOV E, CROWELL R, PAPADAKIS N. Retained intracranial foreign bodies. J Neurosurg 1976; 44: 80-83.
- SIGHTS WP, BYIE RJ. The fate of retained intracere bral shotgun pellets. J Neurosurg 1970; 33: 640-653
- MARKHAM JW, STEIN S, PELLIGRA R, LIPPE P, NOYES J. Use of centrifuge in the treatment of an intraventricuIar metallic foreign body. J Neurosurg 1971; 34: 800-804.
- SUGITA K, DOI T, SATO O, TAKAOKA Y, MUTSUGA N. Successful removal of intracranial air-gun bullet with stereotactic apparatus. J Neurosurg 1969; 30: 177-181.
- DANDY W. The brain. In: Lewis Practice of Surgery. Hagerstown, Md.: Wf Prior Co. Inc, 1932; 12: Chap 1,279-280.