
|
|
|
CLINICAL STUDIES / ETUDES CLINIQUES
SEVERE NEUROLOGICAL INVOLVEMENT IN TUBEROUS SCLEROSIS: A REPORT OF TWO CASES AND A REVIEW OF THE AFRICAN LITERATURE
ATTEINTE NEUROLOGIQUE SÉVERE LORS DE LA SCLÉROSE TUBÉREUSE : A PROPOS DE DEUX CAS ET REVUE DE LA LITTERATURE AFRICAINE
E-Mail Contact - LAGUNJU IkeOluwa Abiola :
ilagunju@yahoo.co.uk
ABSTRACT Tuberous sclerosis (TS) is a genetic disorder characterised by the triad of cutaneous lesions, epilepsy and mental retardation. TS is known to have a wide clinical spectrum, with some affected individuals having only the cutaneous manifestations, normal IQ and no seizures, while others are severely affected having intractable seizures and profound mental retardation. A report of two Nigerian children with TS managed at the University College Hospital, Ibadan, Nigeria is presented. Both had severe neurological manifestations of the disease and a sub clinical affectation was found in a first degree relative in one of them. INTRODUCTION Tuberous sclerosis (TS) is a genetic disorder characterised by the triad of cutaneous lesions, epilepsy and mental retardation.13 The first clear description of TS is usually attributed to Bourneville who, in 1880, recognised the pathological features of white tumours or tubers and areas of sclerosis of the cerebral gyri at post-mortem in patients with epilepsy and mental retardation.8 In 1908, Vogt reported the classical triad of TS consisting of mental retardation, seizures and a facial skin eruption, then called adenoma sebaceum.8 The facial eruptions are now called angiofibromas, which more correctly describes the histological features as there is no involvement of the sebaceous glands. Vogt also noted that cardiac and renal tumours can form part of the disease. In 1920, van der Hoever described the small retinal tumours which he called retinal phakomas and he noted that similar lesions do occur in the intestine, thyroid and bone. Other organs which may also be affected by the disease include the liver, the lungs and the spleen.7 The hereditary nature of TS was first reported in 1913 and was studied in 1935. The disease is now known to be dominantly inherited but the majority of cases are due to new mutations. In 1987, the gene locus was discovered on chromosome 9 and in 1992; a second locus was discovered on chromosome 16. 4,5 The disease is now known to be more common than was previously published with an incidence of about 1 in 7,000 worldwide. TS is known to have a wide clinical spectrum, with some affected individuals having only the cutaneous manifestations, normal IQ and no seizures, while some are severely affected having intractable seizures and profound mental retardation. The disease is sometimes inherited from unsuspecting parents who themselves do not have fits or mental retardation. There have been very few reports on TS in Africans.1,2, 6 The first case in the African child was reported in 1967. 1 A report of two cases of TS, managed by the paediatric neurology and neurosurgery units, University College Hospital, Ibadan, Nigeria, is presented. Case 1 CM, a twelve year old girl presented at the Paediatric unit, University College Hospital, Ibadan, Nigeria on account of 6year history of recurrent convulsions and a day history of fever and loss of consciousness. She developed recurrent convulsions at the age of six years. Episodes of convulsions were generalised tonic, clonic in nature, lasted for about 10mins each time, associated with impairment of consciousness, involuntary micturition and usually followed by post ictal sleep. The convulsions occurred both during the day and at night. Frequency of convulsions was about 5 times per month. Her parents had resorted to the use of herbal medications for the treatment of the convulsions because they were financially handicapped and could not afford the cost of orthodox therapy but this did not offer any beneficial effect. The day before presentation at our centre, she developed a high grade fever. The frequency of the convulsions then got worse; she developed prolonged seizures and had had fifteen episodes over a period of nine hours preceding presentation. She became unconscious following the repeated attacks of convulsions. Pregnancy, birth and neonatal periods were uneventful. Her motor milestones were attained within the recognised normal limits, although mother believed that when compared with her siblings, she attained her milestones later than the others did. She performed poorly in school and had to drop out of school at age ten years because of frequent seizures and poor academic performance. The other siblings were said to be doing well in school. Her mother noticed the “facial skin eruptions” when CM was about two years old but she was not bothered as she also had similar lesions on her face. She was the second of three children in a monogamous family and there was no family history of epilepsy. None of the other two children had similar skin lesions. CM’s mother was noted to have the facial angiofibromas. She is a housewife who had no formal education and had never had any attacks of seizures in her lifetime. On examination at presentation, she was acutely ill, febrile (temperature 39.6OC). She had firm, discreet, dark papules on the nose and the cheeks, having a butterfly distribution (Fig 1). She was not pale, anicteric and had no significant peripheral lymphadenopathy. Neurological examination revealed that she was comatose with a Glasgow coma score (GCS) of 7/15. She had no signs of meningeal irritation. Her pupils were constricted, about 1mm in diameter bilaterally and unresponsive to light. Muscle tone was normal in all her limbs, the deep tendon reflexes were normal and the plantar response was flexor bilaterally. The diagnosis on admission was tuberous sclerosis complicated by status epilepticus and raised intracranial pressure. Differential diagnoses considered were meningitis, cerebral malaria and intracranial tumour. A lumbar puncture was done after mannitol infusion and cerebrospinal fluid examination was normal. Blood film examination revealed malaria parasites and she was placed on intramuscular Artemether injections. The seizures were controlled with intravenous phenobarbitone injection. She was scheduled for computerized tomography scan of the brain but unfortunately, she died before the investigation was carried out. Her clinical condition progressively deteriorated with deepening coma and she died 41 hours after admission. A post mortem examination was carried out. Post mortem examination confirmed the clinical impression of TS. The major visceral abnormalities involved the brain and the kidneys. There were widespread bilateral cortical tubers located in the superior and inferior frontal, temporal and occipital lobes of the brain (Fig 2). Subependymal nodules were found in the lateral ventricles medial to the fornix anteriorly, giving the characteristic “candle dripping appearance” (Fig 3). The subcapsular surfaces of both kidneys showed multiple yellow nodular lesions of varying sizes ranging from 0.3-0.5cm in diameter. Histology of the renal lesions confirmed them to be angiomyolipomas – multiple hamartomatous nodular lesions comprising plump smooth muscle bundles interspersed by variable amount of adipose tissue and thin and thick walled vessels. Case 2 O.O, an eight year old boy presented at the paediatric unit of the University College Hospital, Ibadan, on account of recurrent convulsions since age of 4months and a 6month history of blurring of vision, unsteady gait and head tilt to the left side. He had associated headache and early morning vomiting. Physical examination revealed a child who was small for age, with occipitofrontal circumference of 54.5cm. He had firm, discreet, dark papules (angiofibromas) on the nose and the malar region of the face. He had café au lait spots on the calf and shagreen patches on the right lower back. On neurological examination, he was found to be conscious but was not communicating. He had cranial nerve palsies involving the abducens nerves bilaterally and the right facial nerve. There was associated right spastic hemiparesis. Examination of the other systems was unremarkable. The diagnosis on admission was tuberous sclerosis with an intracranial space occupying lesion. Computerized tomography scan of the brain showed obstructive hydrocephalus and features suggestive of subependymal astrocytoma. He had right frontal craniotomy with total tumour excision. He developed hypertension and respiratory failure after surgery. He was managed in the intensive care unit of the hospital but died a few hours after surgery. Histology of the excised brain tumour showed features consistent with a subependymal giant cell astrocytoma. At post mortem examination, the major abnormalities were found in the kidneys and the central nervous system. There were cystic nodules on the capsular surfaces of both kidneys, with cysts of varying sizes, ranging from 0.3 to 1 centimetre in widest diameter. Cut sections of the kidneys showed a distorted architecture with a few renal cortical cysts and greyish white nodules, mainly in the cortical region. The brain showed multiple pale, irregular flattened tubers in the cerebral convexities more towards the midline and tubers on the optic chiasma. The lateral ventricules showed irregular projections of the ependymal lining in to the ventricular cavity giving the characteristic “candle-dripping” appearance and associated hydrocephalus. There was intraventricular haemorrhage with extension into the fourth ventricle. The respiratory, cardiovascular, hepatobiliary, endocrine and gastrointestinal systems were normal. DISCUSSION TS belongs to the group of neurocutaneous disorders classified as phakomatoses. The two cases reported in this write up presented with classical features of the disease as previously documented in literature. Although, TS is a genetic disorder, inherited in an autosomal dominant fashion, a few cases are due to new mutations. One of the cases in this report had a first degree relative affected by the disease. It is however worthy of note that, well the patient’s mother had subclinical affectation; our patient had severe manifestations of the disease evidenced by intractable seizures and severe mental retardation. This finding is consistent with known facts about the disease.8,13 TS is known to have a wide clinical spectrum, with some affected individuals having only the cutaneous manifestations, with normal IQ and no seizures, while some others are severely affected having intractable seizures and profound mental retardation. The hallmark cutaneous features of TS include ash-leaf hypopigmented macules, shagreen patches, forehead plaques, facial angiofibromas, ungal and gingival fibromas.11 The two cases in this report both had facial angiofibromas and one of them had shagreen patches on the back. The two cases had the neuropathological features associated with TS. Both had cortical tubers and subependymal nodules and one had a subependymal giant cell astrocytoma. Subependymal giant cell astrocytoma occurs in 6-14% of individuals with TS and is more likely to occur in childhood.10 These can enlarge and cause obstruction to the cerebrospinal fluid pathways, thereby resulting in raised intracranial pressure, focal neurological deficits and deterioration in seizure control. Case 2 also exhibited progressive deterioration of neurological function associated with the intracranial space-occupying lesion. Renal involvement is common in individuals with TS. Renal cysts are common in childhood, while angiomyolipomas typically arise in middle age.12 In this report, the younger child had multiple cysts in the kidney, while the older one had renal angiomyolipomas. There are few reports about TS in African children. Cisse et al2 reviewed 18 cases of TS seen over a ten year period at the University Hospital Centre, Conakry, Guinea. A high incidence of epilepsy was found in the cases studied. Chalabi-Benabdallah3 also reported a high incidence of epilepsy in the 22 Algerian families with TS studied. Pitche et al9 reported 4 cases of TS from Togo; all showed features of neurological involvement, three had associated epilepsy while the fourth case showed features of autism. Neuroimaging studies to precisely identify pathologies in the brain were however not carried out in the study. Severe neurological involvement appears to be a frequent finding in Africans with TS. Due to the protean and age-dependent manifestations of TS, standard diagnostic criteria are usually employed in making a diagnosis.8,13 Both cases in this report satisfied the diagnostic criteria for definite TS. Late presentation to the hospital adversely affected the prognosis in the cases presented. The presentation of TS in African children is consistent with features reported from other parts of the world.  Figure1 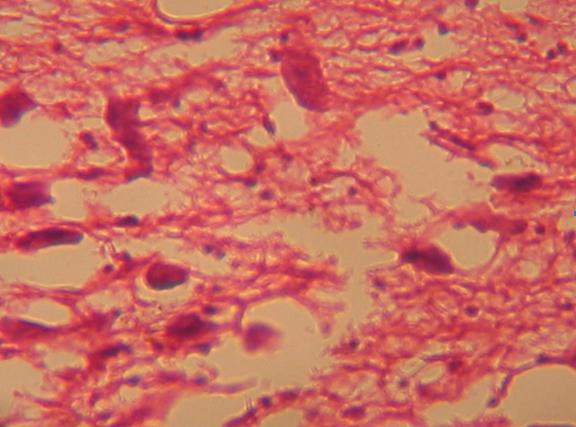 Figure 2  Figure 3 REFERENCES
|
© 2002-2018 African Journal of Neurological Sciences.
All rights reserved. Terms of use.
Tous droits réservés. Termes d'Utilisation.
ISSN: 1992-2647