
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
SUMMARY Painful neuropathies due to any diseases, cause a lot of morbidity since in most cases they respond poorly to various therapies. It was decided to study the clinical features, electrophysiology and response to a short course of oral prednisolone in H.I.V. patients. Between 1988 and 1992 seven cases of neuropathies presenting primarily as a painful syndrome in Human Immunodeficiency Virus positive patients were seen in Nairobi, Kenya there were five males and two females. Their age ranged from 45 to 57 years. Four patients had their H.I.V. diseases presenting for the first time as a painful neoropathy. They did not have any clinical feature to suggest related acquired Immunodeficiy state. The other three patients were known H.I.V. related acquired immunodeficiency cases (AIDS). Two of these AIDS cases had neurophysiological evidence of diffuse sensory neuropathy of axonal type. In the rest of the patients nerve conduction studies were normal. All patients had been given various analgesics with carbamazephine and amytryptilline without response. None were given narcotic analgesics. All patients were first given placebo for one week followed by Oral prednisolone at 0.6mg/kg daily. There was no response to placebo but there was remarkable resolution of pain within one week of oral prednisolone. Therefore a short course of oral prednisolone is useful in the short term management of painful H.I.V. neuropathy. RESUME Les neuropathies douloureuses liees a certaines maladies sont la cause d’une morbidite importante, et repondent mal a de nombreuses therapies. Il a ete decide d’etudier les caracteristiques cliniques, electrophysiologiques et les reponses a un traitement de courte duree par la prednisolone chez les patients seropositifs pour le VIH. Entre 1988 et 1992, 7 cas de VIH (5 hommes et 2 femmes) presentant une neuropathie douloureuse ont ete suivis a Nairobi, Kenya. Leu age variait entre 45 et 57 ans; chez 4 de ces patients le premier signe de la maladie etait une neuropathie douloureuse; il n’existait aucune caracteristique povant suggerer le stade du sydrome d’immunodeficience acquise (SIDA). Les 3 autres patients etaient connus comme ayant un SIDA; 2 de ces patients avaient une neuropathie sensitive diffuse de type axonal, caracteristique a I’examen neurophysiologique. Les enregistrements des vitesses de conduction etaient normaux chez les autres patients. Tous les patients ont ete traites par des analgesiques associes a la carbamazepine et a l’amytryptilline, mais sans resultat favorable. Aucun n’a pris d’analgesique narcotique. Tous les patients ont d’abord ete traites par placebo pendant une semaine, puis par un traitement oral de prednisolone a la dose de 0,6 mg/kg/jour. Il n’y a pas eu de reponse favorable au placebo, mais une remarquable resolution de la douleur avant la fin de la premiere semaine de traitement oral par la prednisolone. Par consequent, un court traitement oral par la prednisolone est utile a court terme dans la prise en charge de la neuropathie douloreuse du VIH. Keywords : Neuropathy, HIV, Pain, Prednisolone Human Immunodeficiency Virus (H.I.V.) can cause a variety of neuropathies as a complication at different stages in the natural history of the disease (1,2). However a distal symmetrical predominantly sensory axonal neuropathy which is often painful is most commonly associated with late stages of H.I.V. infection. The sensory symptoms may be severe with little, if any, sensory or motor signs. This condition may be so painful that the patient is unable to walk because of burning dysethesias. The pathogenesis is not clear. It may be related to direct H.I.V. infection of the nerve or dorsal root ganglia (4). The treatment of such a neuropathy is symptomatic. The tricyclic antidepressants sometime in combination with flupheazine have been the main drugs given over long periods of time (5,6). However many patients obtain no pain relief with these drugs and only occasionally is complete pain relief achieved. The cardiac and central nervous system side effects of tricyclic antidepressants greatly limit their use over prolonged periods of time especially in elderly patients. Therefore as is generally the case of neuropathic pains the treatment of painful neuropathies in H.I.V. remain unsatisfactory. Most of the research work in H.I.V. is geared to the development of an effective vaccine and more potent anti viral drugs. This is the correct direction of research if the pandemic is to be halted. However as practising neurologists these miserable patients do end up with us and we have to help in putting some sunshine into their bleak life or whatever remains out of it. This study was inspired by an elderly male patient who was otherwise healthy with severe burning pain in the lower limbs and a very painful band-like pain in his epigastrium spreading to the lumbar spine. He had consulted several orthopaedic surgeons and gastroenterologists with several myelograms, barium meals enemas and endoscopies virtually through all his orifices which were all normal, before landing with the author, who did his elisa for H.I.V. which was positive. Various drug regimes did not help him, but his pain resolved within one week of oral prednisolone 40mg O.D. This was tailed off in another three weeks. His pain recurred a year later and he again responded to the same treatment. Corticosteroids have been used with benefit in several H.I.V. – associated conditions. Theses include idiopathic thrombocytopenic purpura (8). aphthous ulceration (9). lymphoid interstitial pheumonitis (10). Pheumocystis carinii pheumonia (11). They have also been used in the treatment of cerebral oedema associated with central nervous system infection by Cryptococcus (12) and Toxoplasma (13). They may have a role in the amelioration of symptoms of mycobacterium avium in intracellulare infection and of terminal disease. However corticosteroids may possibly induce clinical cytomegalovirus disease and may induce progression of Kaposi’s sarcoma. (14). METHODS Patients: Subjects were eligible if they had severe pain enough to seek medical help. Pain was the presenting symptom at that time. At the time of the study they were of good general health no other symptom except pain in the extremities. There was no clinical or laboratory evidence of active infection in any system of the body and no past history of peptic ulcer disease, diabetes or hypertension. None of the patient was on Zidovudine therapy. Each patient underwent a full neurological and general examination. Blood counts, VDRL, ESR, G.T.T. Urea, electrolytes, creatinine, liver function tests, chest xray, serum protein for electrophoresis, T4, T3 TSH, folate B12 levels, cerebrospinal fluid for protein, sugar, cell count and VDRL and nerve conduction studies. Urine examination including culture and sensitivity stool for ova and cysts, chest xray and serum elisa test for H.I.V. were all done. CD counts were not done. Placebo was given in the first week. Prednisolone was given at a dose of 0.6mg/kg daily as a single dose to the nearest 5mg thereafter. This was a single blind placebo controlled trail. Pain ratings using a 100mm visual analogue scale (VAS) of pain were completed twice before the placebo at an interval of 24 hours. This was then repeated at the end of each week for the next five weeks. During the medication period the patients were asked for any new symptoms and symptoms of side effects of the prednisolone. Blood pressure and blood sugar was also checked at each visit. Each pair of VAS ratings was averaged before and after one week of placebo and this average was compared to the mean of VAS ratings one week after prednisolone. Prednisolone was then trailed off in the following three weeks. The mean ratings one week after placebo and one week after prednisolone was compared by two-tailed paired test. RESULTS Seven patients were seen between 1988 to 1992 and they presented primarily with peripheral painful sometimes burning dysethesias. They were five males and two females. Their age ranged from 45 to 57 years with a mean of 52 years. Four of the patients had nothing in the way of clinical features to indicate H.I.V. infection. Three patients had in the past been treated for Acquired immunodeficiency conditions (AIDS) with known positive serology for H.I.V. infection. None of the patients suffered from post herpetic neuralgia. All the tests indicated in the methods section were normal. This included he cerebrospinal fluid studies and nerve conduction studies except in two patients known to have AIDS. These patients had mild axonal diffuse sensory neuropathy. Figure I and II shows the nerve conduction results of these two patients. Figure III shows the mean pain intensity ratings before and after one week of placebo, before and after one week of prednisolone. There was a significant decrease of pain (p = 0.02) one week after prednisolone as compared to placebo. 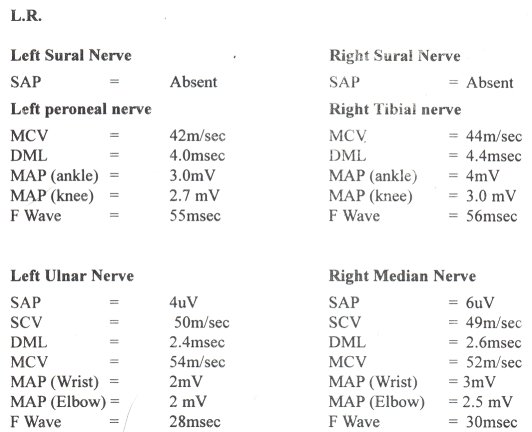 Figure 1 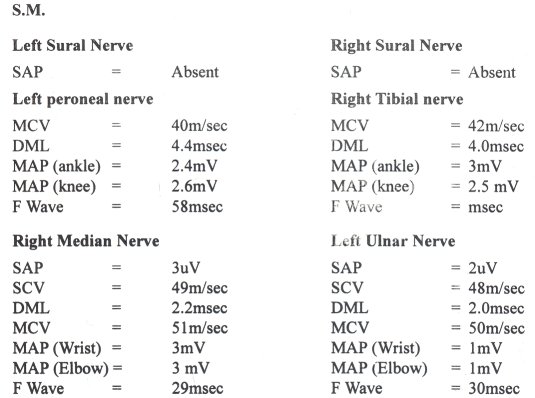 Figure 2  Figure 3 Only one patient complained of ankle swelling during the prednisolone phase. This disappeared on trailing off the prednisolone. No other drug related side effect was recorded during the placebo and prednisolone treatment. There was no symptom or sign to suggest activation of a latent infection. DISCUSSION Although sensory neuropathy which is often painful is associated with late H.I.V. infection, this study shows that it can occur at any stage of H.I.V. even before the patients have gross features of immunodeficiency. It can even be the presenting symptom of the H.I.V. state. Most of these patients had been given tricyclic antidepressants, anticonvulsants, (phenytoin and carbamazepine) fluphenazine or combinations of these drugs before they were referred to the neurology service without pain relief (5,6). None had been given morphine and its analogues. This single blind study shows that prednisolone reduces pain in painful neuropathy associated with H.I.V. when the patients finished their prednisolone course the pain relief was sustained. Therefore cross-over studies could not be done. The effect of prednisolone in relieving pain in these patients could be at several sites. The steroid could reduce the excitability of neural tissue by alteration of the ratios of extracellular to intracellular sodium and intracellular to extracellular potassium, by decreasing the release of arachidonic acid from phospholipids and hence a decrease in prostaglandins which are essential in the mediation of pain in the peripheral nervous system or by its effects on inflammation and its mediators in the peripheral nervous system (7). The later mechanism is thought to be the most important effect of corticosteroids in this study as the therapeutic effect was long lasting even when the corticosteroids was stopped. All the patients received non-steroidal anti-inflammatory drugs prior to this study without pain relief. This study may have observer bias and obviously the number of patients is small. Therefore it would be important to carry out a larger and double blind study or even a multi-centre study to study the effects of steroids in the painful neuropathy of early and mid-stages of H.I.V. Nerve biopsies with electron microscopy and immunohistochemistry would also be essential in a more detailed study.
SUMMARY Spina Bifida Cystica (SBC) is the commonest of the spinal dysraphic disorders in Africa, like the rest of the world. However, experience and reports in the literature set Africa apart from other areas in certain respects. Thus, SBC is less frequent in African than in Caucasians. African males are more affected than females; in Europe, female patients outnumber males. The European criteria for selecting (or rejecting patients to be actively treated cannot be applied wholesale to Africa where social factors dilute or over-ride those criteria). The disease has unique psychosocial and cultural connotations in Africa where its long term problems are awaiting study. Finally the use of folic acid in its prevention already established in many parts of the world is still crying for adoption in Africa. RESUME La spina bifida kystique est l’anomalie vertebrale la plus courante en Afrique, comme ailleurs dans le monde Cependant, l’experience ainsi que l’analyse de la litterature montrent qu’en Afrique, elle presente certaines particularites: une frequence moindre chez l’africain qe chez le caucasien, une predominance chez les hommes. Les criteres europeens de selection des patients a traiter ne peuvent pas etre appliques globalement a l’Afrique ou les facteurs sociaux modifient ces criteres en les attenuant ou en les exagerant. La maladie a une connotatin culturelie et psychologique propre ou l’etude de ses consequences a long terme n’est pas encore entreprise. En outre, l’utilisation de l’acide folique pour la prevention est deja en place dans de nombreuses regions du monde, mais toujours inexistante en Afrique. Keywords : Spina bifida cystica, Africa Spina bifida cystica (SBC) is one of the congenital lesions which together with spina bifida occulta, anencephaly and encephalocele make up the neural tube defects. A number of genetic and environmental factors conspire to cause neural tube opening leading to spinal dysraphism, one of the most serious developmental disabilities affecting the craniospinal axis. INCIDENCE The reported incidence of SBC in the African is less than 1 per 1000 deliveries. In Durban, South Africa (18) and at the University College Hospital, Ibadan, Nigeria an incidence of 0.46 per 1000 was recorded for SBC among all live births (7). In 1969, Gupta (17) reported an incidence of 0.94 per 1000 total deliveries (live and stillbirths). These figures are much lower than the 3 per 1000 live births encountered in the United Kingdom (14) and the 4 per 1000 among all deliveries in the South Wales (20). It thus appears that SBC is less frequent in the African than in the Caucasian. HOSPITAL PREVALENCE The first reports of central nervous system malformation in Africa were based on the prevalence noted among deliveries in general hospitals in 1966 in Cairo in North Africa (19) and in 1968 in Lagos, Nigeria, West Africa (21). The lesions found in these studies, in order of frequency were anencephaly, hydrocephalus and SBC. With the establishment of neurosurgical and neurological units on the African continent, hospital surveys of large representative series of congenital malformation of the central nervous system started to emerge. In the series from East Africa (34) and from francophone (10) and anglophone (6, 29) West African countries, SBC ranked second to hydrocephalus. In Zimbabwe, SBC was the commonest CNS malformation encountered (22) PATHOLOGY In Africa, like the rest of the world, it is the commonest member of the family of spinal dysraphic disorders which include spina bifida occulta, pseudotail, lumbosacral lipoma and anterior sacral meningocele (4). Many pathological varieties of SBC are known. The simplest form, the meningocele in which the cyst contains only CSF without myelin or nerve roots but with intact skin and in which the patients has intact sphincter and normal limbs, is relatively rare. Meningocele in Africa accounts for between 2 percent (1) and 10 percent of SBC. Myeloceles in which the cyst contains cord and nerve roots, are, by contrast, common. Henry and Michel (18) reported 27 meningoceles and 166 myeloceles in West Africans subdivided myeloceles into myelomeningoceles in which the sac contains nerve roots only and meningomyeloceles in which cord and nerve roots lie in the cyst. Bailey (11) reported the rare case of double meningocele in a Ugandan child; in Malawi we have encountered a patient with lumbosacral SBC as well as a high dorsal spina bifida occulta (5). CLINICAL MANIFESTATIONS Most reports in Africa show male predominance over females in contrast to the Caucasian experience whereby females outnumber males in a ratio of 2 to 1 (32). At Ibadan, Nigeria, the male:female ratio was 1.2 to 1 (7). As in other parts of the world SBC in Africa is a syndrome comprising the cyst, hydrocephalus, sphincter disturbance and neuromuscular imbalance manifesting as varying and various degrees of lower limb deformity. The incidence of preoperative hydrocephalus in Africa varies from 30 to 42 percent (3) as compared to the 80 to 90 percent reported in western literature (35). The difference is probably due to closer patient follow-up and better documentation of cases in centres outside Africa. Nevertheless, like everywhere else, the highest incidence of hydrocephalus occurs in thoracic lesions. Children who came late to hospital (and many do so in Africa) show reduced incidence of hydrocephalus (4). TREATMENT Early closure of SBC within 24 to 48 hours of birth, as practised in many parts of the developed world, is not always possible in Africa due to late presentation in hospitals. As a result, the management of the disease in Africa is bedevilled by cyst infection and subsequent meningitis, late convulsions and mental retardation (9). In children presenting in the first week of life, staphylococcus aureus is the dominant infective organism; in other children presenting late, pseudomonas aeruginosa and coliforms predominate (27). In 1971 Lorber (23) revolutionised the treatment of SBC by suggesting criteria for NOT operating on affected children. The criteria include gross hydrocephalus at birth (maximum head circumference 2cm or more above the 90th percentile in relation to birth weight); severe neuromuscular imbalance leading to paraplegia; thoracolumbar lesions; associated extra – CNS anomalies such as Down’s syndrome and cyanotic heart disease. In Britain, such children who are selected to die, in a form of « active euthanasia » (26), are kept on sedation and given food and water on demand. Inspite of the wide acceptance in paediatric circles all over the world, Lorber’s criteria have some limitations in realistic practice and application within Africa. Firstly, if adopted in Africa, Lorber’s strictures will exclude almost eighty percent of children with SBC from surgery (27). Secondly, the criteria did not take into cognisance the not uncommon situation when parents press for surgical treatment of SBC in their children, even when Lorber’s criteria for rejection are overwhelming (33). Mezue and Eze (27) painted a poignant picture of this social scenario in our African setting where parents will do anything for their child, especially the male, and where a visible unsightly defect, like the cyst of SBC, is believed to be capable of reincarnation if the afflicted child is allowed to die with the cyst unremoved. In parts of Africa, the deformed child is a pariah, unfit to receive the dignity of a naming ceremony (2) or the ritual of circumcision. The tendency therefore is to operate on most or all children, except where there are strong and compelling contraindications (30). Post operative gain is not dramatic. In Nigeria, 40 percent of limb paralysis and urinary incontinence show improvement (30); in South Africa, children with mild to moderate paralysis learn to walk (18). Surgery has even been offered to improve walking through hip stability in children with mid-lumbar myelomenignocele in Cape Town, South Africa (15). Hydrocephalus which occurs in about two thirds of children with SBC poses real problems. Most cases of the associated hydrocephalus tend to arrest spontaneously, but in about 10 percent of cases, clinical hydrocephalus develops after closure of the SBC. Shunting procedures are more often used elsewhere than in Africa. McLone (26) reported that about 90 percent of children with SBC will require shunting procedure for the associated hydrocephalus. Here in Africa, shunt procedure is offered to children with stridor (8) or those with rapidly progressive head enlargement. The treatment of SBC does not, and should not, end with the operative repair of the cyst or placement of shunt for the associated hydrocephalus. The child with SBC puts stains and stresses, on the family and the disease has socio-cultural undertones which has been well orchestrated in the West but only occasionally studied in Africa. One such report from Nigeria (31 ) found that the families of children with SBC had to undertake difficult distant journeys to hospitals, spanning hundreds of kilometres, the commuters being mostly mothers unaccompanied by their husbands or a senior relative. The disease is attributed to witchcraft or the evil spirit cast on mothers during their pregnancy. When the gains of surgery are undramatic, as they often are, or the early hopes of hospital treatment have become stultified, clinic attendance stops. The children are then kept at home, social stigmata to the clan who are considered better dead than alive. These findings from Nigeria, some in fainter, others in bolder relief, apply to most parts of developing Africa. Clearly more information is needed on the long-term problems of the African child with SBC (31). Prevention on neural tube defects appears the best policy of management of SBC in Africa. It has been shown in a United Kingdom medical Research Council Study that 4 mg per day of folic acid prevented about 75 percent of neural tube defects (24, 37). Women planning pregnancy have been advised to take 400 micrograms of folic acid a day (36). They should also eat more folate-rich foodstuffs, such as vegetables like Brussels sprouts, spinach and green beans, fruits like orange and orange juice and some cereals and cereal products (25). Similar recommendations have been made in Hungary (13) and in the United States of America (12). These simple measures, tested and tried and found to be useful, should be more widely adopted in Africa to prevent SBC and its ravages and miseries to the patient, his or her family and the society. CLINICAL ASPECTS OF SEIZURE DISORDERS AT OUAGADOUGOU BURKINA FASO RETROSPECTIVE STUDY OF 532 CASESSUMMARY A retrospective analysis of 532 patients with seizure disorders seen in the Internal Medicine department of Yalgado OUEDRAOGO hospital, Ouagadougou, over a seven years period is presented. The commonest type of epileptic seizure encountered was generalized epilepsy of the tonic-clonic type (61.5%), 35.5% had partial seizures, petit-mal type was seen in only 3%. Possible etiologies has been identified in 29.7% of the cases. Aspects of treatment are briefly discussed. These results are compared with the experiences in other African countries. RESUME A partir d’une serie de 532 observations de patients colligees dans le service de Medicine Interne du CHU de Ougadougou, pendant une periode de 7 ans, les Auteurs decrivent les aspects cliniques des crises epileptiques rencontrees; il s’agit de 108 patients hospitalises (dont 44% d’etat de mal epileptique), et de 424 patients ambulatoires. La repartition des types cliniques de crises. montre une predominance des crises generalisees tonico-cloniques (61,5%); les crises partielles suivent avec 35,5%. Les absences de 1 ‘enfant ne font que 3%. Des etiologies possibles sont identifiees dans 29,7% des cas, dominees par les causes traumatiques et les sequelles d’infection du systeme nerveux central. Le traitement medicamenteux utilise plus souvent le phenobarbital a cause de son cout peu eleve. Keywords : Epilepsy, Burkina Faso INTRODUCTION Epilepsy is one of the commonest neurological disorders world-wide, and it is more common in developing countries than in developed countries. Epilepsy is not well studied in Africa. Most studies on epilepsy in Africa have been based on hospital attending patients. In Burkina Faso, there is no hospital-based study concerning epilepsy up to now. This study was carried out to describe the different clinical aspects of seizure disorders in Burkina Faso. PATIENTS AND METHODS It is a retrospective study in which the medical records of all patients with seizure disorder seen on out-patient and/or in-patient basis, in the department of Internal Medicine of Yalgado OUEDRAOGO Hospital, between October 1, 1987 and December 31, 1994 were reviewed. All the children included in this study were seen on consultation, and subsequently followed in the paediatrics department. A total of 532 patients has been identified. From the medical records of these patients all the available clinical, laboratory, and other informations have been collected and analysed. The classification of seizures was done on the basis of history using the International League Against Epilepsy (ILAE) classification (1981) (10). Electroencephalography results were not available. RESULTS Of the five hundred thirty two patients who have been included in this study: 108 were in-patients and 424 were out-patients. Of these, 87 were children between the age of 0-14 years (46 boys, 41 girls). Of the total number of patients, 68.4% were males and 31.6% were females. The distribution according to the age and sex is presented in Table 1. TABLE 1 Age and Sex distribution of patients.
The distribution according to the clinical type of seizure is presented in Table 2. Generalized seizures of the tonic-clonic type was the commonest type seen (61.5%), followed by secondary generalized seizures (18.8%), and partial complex seizures (10.3%). Petit-mal seizure type was rarely encountered (3%). TABLE 2 Clinical types of seizures
Probable etiologies have been identified in 158 patients. The list of identified etiologies is shown in Table 3. History of the head injury and chronic alcoholism were obtained in 28.5% and 17.7% cases respectively. A history suggestive of central nervous system infection was obtained in 20.2% cases. 9.8% of the patients had antecedent of cerebrovascular accidents. 6.3% of the patients had intracranial space-occupying lesions. TABLE 3 Probable etiologies of seizures in 158 patients.
8.9% had advanced HIV infection (AIDS); 6.3% had neurocysticercosis. Besides, past history of febrile convulsions has been noted in 21 patients. Among the 108 hospitalised patients, 48(44.4%) had status epilepticus. In five of these patients this was the initial presenting manifestation. 329 of the patients have been taking their treatment regularly. The drugs prescribed were the following: phenobarbitone, 250 patients (76%), sodium valporate, 42 patients (12.8%); carbamazepine, 32 patients (9.7%); phenytoin, 5 patients (1.5%). Patients with status epilepticus had been treated with diazepam or clonazepam in perfusion. DISCUSSION Apart from the 5 patients with inaugural status epilepticus, the other patients could be considered epileptic patients. In this series a male predominance has been observed with sex ratio 2.6. This is similar to the findings of other studies from Africa (1, 2, 5, 11, 13). The degree of male predominance is less marked in developed countries (10). The possible explanations for this male over representation are the tendency in Africa for males to seek medical attention more readily than females and the migration of men to cities due to economic and social reasons (6, 12). As in other hospital series in Africa (1, 11, 12), in our series the majority of the patients were young. 82.1% of the patients being below 40 years of age and only 6.8% of the patients were above 60 years of age. The pattern of the epilepsy found in this study is similar to what has been reported in the literature from other African countries (4, 5, 11, 12, 13) generalized seizures of the tonic-clonic type being the most frequent type of seizures seen. On the other hand petit-mal epilepsy was rare. The relative rarity of absence seizures in our study and other studies from Africa (5, 13) could be due to under-diagnosis of the disorder because of its relatively subtle clinical features. In this series possible etiologies has been identified in 158 cases. Past history of head injury was the commonest disorder identified accounting for 28.5 % of these cases, followed by sequalae of cerebral infection in 20.2%, and chronic alcoholism (17.7%). It is important to note that 10 patients had clinical evidence of cysticercosis, and their seizures were probably consequences of central nervous system involvement of the cysts. Among the 48 patients with status epilepticus, in 44%, the precipitating factor was cerebral malaria; in the others, the discontinuation of the antiepileptic drugs was the precipitating factor identified. The attitude of the population towards epilepsy and epileptics make treatment and follow-up of the patients difficult. Among the antiepileptic drugs, phenobarbitone is the one which is widely used, because of its reasonable price. PROFESSOR B. OLUWAKAYODE OSUNTOKUN AND HIS NUNC DIMITTISKeywords : Oluwakayode, Osuntokun Professor Benjamin Oluwakayode Osuntokun died in Cambridge, England on September 22 1995 after a protracted illness and was buried in his native Okemesi, Ekiti, Nigeria on October 7, 1995. His death robbed Nigeria of its leading neurologist and one of its icons of modern medicine; Africa of one of the Foundation members of the Pan African Association of Neurological Sciences (PAANS) and the World Federation of Neurology of one of its most prolific writers and productive researchers on tropical neurology. Born in January 1935 Osuntokun started his elementary school education in 1940 at the Holy Trinity School, Ilawe Ekiti, where he was born, and finished it in 1945 at Emmanuel School Ado Ekiti. He entered Christ’s School Ado Ekiti in 1946, the famous and prestigious secondary school which moulded many Nigerians who later won prominence in various walks of life; thereafter, he studied medicine at the University College, Ibadan, then a College of London University. His academic career was a remarkable string of distinctions and honours: he was top of his class at Emmanuel School at Ado Ekiti; in 1951 at Christ’s School he passed the London Matriculation Examination and then the Cambridge School Leaving Certificate Examination with several distinctions and in 1961, he graduated in medicine with the MBBS degrees of London with honours in Pathology and in Obstetrics and Gynaecology. After house jobs at the University College Hospital, Ibadan, and the mandatory stint as Medical Officer in the then Western Nigeria Ministry of Health, Osuntokun went to the Professorial Unit of Harold Scarborough in the Welsh National School of Medicine in Cardiff in 1963 as Senior House Officer to study for the MRCP which he passed in London at his first attempt in 1964. I visited him in Cardiff during his stay there. « One does not seem to get tired studying in this cold climate », he confessed to me with his usual good humour as he lapped up the immense opportunities and congenial academic ambience which the post in Cardiff offered. And after passing the MRCP London, we spent together a memorable and delightful weekend of relaxation, celebration and carousing in Lancaster and visiting parts of Yorkshire. He returned to Ibadan in 1964: eager to join his young family (his first child, a daughter, was born in 1963) and to take up appointment as a Rockefeller Foundation Medical Research Training Fellow in Neurology in 1964 and settle into a career in Ibadan. But he was not quite ready to do so. With his young family and a Smith and Nephew Fellowship in neurology, he returned to the United Kingdom towards the end of 1964 to hone his skill at clinical and experimental neurology. He spent most of the time in Newcastle-upon-Tyne where he came under the tutelage of two giants of neurology: the legendary and avuncular Henry Miller, a raconteur who laced his neurology with wit and wisdom and John Walton, now Lord Walton of Detchant, a man with a penchant for details and depth in neurological knowledge bordering on the encyclopedic. I visited him in Newcastle and was privileged to attend one of their joint neurology – neurosurgery sessions at the Royal Victoria Infirmary at which Mr Hankinson the neurosurgeon was present. Osuntokun spent a short spell at the National Hospital for Nervous Diseases, Queen Square, London before he returned to Nigeria at the end of 1965 and was appointed Lecturer in the University of Ibadan. Thus ensconced in the Department of Medicine under Professor Alexander Brown, Osuntokun started a career in neurology that was to spawn a cornucopia of scientific and scholarly publications, solely and jointly on epilespy, nutritional and toxic neuropathies, cerebrovascular diseases, headaches and pain problems, neoplasms of the nervous system, the neurology of diabetes mellitus and of the hameglobinopathies of Africa. The coda of his neuroscientific research was neuro-epidemiology which engaged his attention in his last days with the same success that attended his foray into neurology in his prime. Preeminent of his work in neuroepidemiology was the study of community dementia among the Yorubas of Nigeria in comparison with the blacks of United States. In the interest and service of neurology, he visited diverse places in every part of the world and held many appointments. Of particular interest to this paper, he was Foundation Member, Nigeria Society of Neurological Sciences and was Secretary from its inception in 1966 to 1970 and later President from 1983 until his death in 1995. He was also a Foundation Fellow of the Pan African Association of Neurological Sciences (PAANS) which was founded in Nairobi in 1972. In his postgraduate and more mature career, Osuntokun gained a string of postgraduate degrees and professional qualifications: PhD (Ibadan) 1969; MD (London), 1971; FRCP (London) 1974; FMCP (Nigeria) and FWACP, 1976 and DSc (London) 1977. In Nigeria, he was made an Officer of the Federal Republic (OFR) of Nigeria in 1978 and in 1984 he received the highest award of his country, the Nigerian National Merit Award (NNMA) for distinguished contribution at national and international level in the Sciences, Medicine, Literature, Arts and Culture. In addition, in the same year, the University of Maiduguri awarded him DSc (Honoris Causa) and in 1985, shortly after his 50th birthday, two Chieftaincy titles were conferred on him in Ekiti, the district of his origin. In January 1995, he turned 60. On the menu which he served guests at the diamond jubilee was an unusual item: copies of his curriculum vitae in which he detailed his background, professional experience; appointments at national and international level; membership of learned societies; scientific conferences attended from 1964 to 1994; papers presented; guest lectures given;, bric-a-brac of his other attainments and a list year by year of his 321 publications. He titled the booklet « Nunc Dimittis » of Oluwakayode Osuntokun. The publication was the quintessence of diligent detailed documentation, so comprehensive that Osuntokun asked on its front cover, and certainly with some justification, « Need anyone say more? » I doubt if any more, in terms of broad factual details can be added to this « Nunc Dimittis », a salutary lesson to all those aspiring to pen their autobiography to do not too long after the age of 60 years, certainly before the mind starts getting fickle and the memory becoming blurred. Some aspects of the booklets are worthy of comments. His father died aged 66, his most senior brother at 69 and he in his 61st year – all in contrast to Osuntokun’s beloved mother who died at the ripe old age of 90. His religious and spiritual upbringing started much earlier than his mates at school imagined. It started, antenatally, from the miracle of his birth wrought by prayers; it continued in the childhood years which he spent in the compound of the apostolic church: at the age of six years, he was precocious enough to read the native edition of the Bible from cover to cover. One suspects that the regular religious knowledge classes which we all had at Christ’s School Ado Ekiti must have been child’s plays to him! The education in Christ’s School gave its students more than a religious philosophy to prepare them for the battles of life. The school imbued them with a disciplined mind, love of hard work and industry, self-confidence and the grit to meet challenges. Osuntokun was an archetype of that generation. Some of us who made successful careers in the sciences left Christ’s School without physics and chemistry, and like Osuntokun « saw a bunsen burner for the first time » as medical undergraduates. It was from such an unprivileged and unpropitious origin that Osuntokun grew, an apostle of hard work, to attain the pinnacle of his profession. The Nigerian National Merit Award which he gained in 1984 Was his deserving ultimate prize. What was puzzling was the citation that it was for his contribution to psychiatry and sickle cell anaemia (1). True, he wrote a few papers on these subjects but his monumental and enduring contributions were in clinical and investigative neurology. Recognition of merit is the kernel of a prize award; the citation that goes with it, usually the handwork of a committee, may go askew. Such was the ease of Nobel laureate, Egas Moniz of Portugal who was awarded the prize in medicine for his work on frontal leucotomy and not for his more substantial and far reaching introduction of carotid angiography in the diagnosis of neurological disorders. It must be difficult to determine which of Osuntokun’s man publications are more significant and substantial than the others. One can use the yardstick of the frequency of reference to a particular publications recorded in the literature; future study of his booklet can accomplish that task. For now, and from personal knowledge, the two most notable of his writings are numbers 6 and 7 on page 49 of his « Nunc Dimittis », which incidentally were both written in 1968 when Osuntokun was 33 years old, the age when most artists and achievers are at the peak of their productivity. « Congenital pain asymbolia and auditory imperception » (2) was a unique case report, one of his earliest series of « First case in the African » which he published with the Italian academic, Lucio Luzzato, then Professor of Haematology in Ibadan, later at the Hammersmith, London and now in the United States of America and the legendary late Latendu Odeku, the African neurosurgeon. The disease has become a classic and named eponymously after Osuntokun, the first author (3). The flagship of his scientific papers is number 6, « An ataxic neuropathy: a clinical, biochemical and electrophysiological study » which appeared in the journal, Brain (4). He carried out the research reported at Epe, Western Nigeria, near the sea coast where people consumed a monotonous diet of ill processed cassava without supplementation, leading to nutritional deficiency which manifests as an ataxic neuropathy. He mapped out the epidemiology of the disease. Encouraged by is then Head of Department, Professor Alexander Brown and ardently supported by Professor Joseph Edozien of Chemical Pathology, Osuntokun was able to carry out an exhaustive study of the basic science aspects of the neuropathy. Up till that time, the disease attracted as many theories as there were writers and the few investigators who looked beyond the clinical aspects of this neuropathy were at sixes and sevens about its aetiology. Osuntokun found that the disease was due to cyanide intoxication. To him therefore belongs the kudos of unravelling the biochemical basis of what up till the 1960s was a confused clinico-pathological entity. I remember his exultation the day he got the galley proof of the paper from Denis Williams, the Editor of Brain; he was over the moon with sheer boyish excitement. He read and re-read it many times; Odeku and myself also checked it to ensure that it was perfect. With the appearance of that paper in Brain, Osuntokun immediately became a name to conjure with in tropical neurology. An editorial on Ataxic Tropical Neuropathy appeared in the British Medical Journal in September 1969. In the same month, he presented his work at the World Federation of Neurology Conference in New York. I remember him standing on the podium to be introduced to the New York audience as the authority on the biochemistry of ataxic neuropathy, then the latest phenomenon in tropical neurology. It was certainly his finest hour. A Thesis in 2 volumes of 449 pages which came out in 1969 on Chronic cyanide intoxication and a degenerative neuropathy in Nigeria earned him the PhD degree of the University of Ibadan. In 1971 that seminal paper in Brain earned Osuntokun the Sir Langley Memorial Prize of the School of Tropical Medicine, Surgery, Hygiene, Sanitation, Entomology and Parasitology for the year 1968 to 1971. On the whole, he produced 34 papers on his famous neuropathy in his life time. Recipients of copies of his « Nunc Dimittis » marvelled at the prodigious attainments which his life incarnated. Olufemi Illori, one of his classmates at Christ’s School complimented him on his achievements, wondering if Osuntokun had not burnt out himself in the process. Hippocrates, acknowledged father of medicine, had in 406 BC, defended Osuntokun in one of his famous aphorisms in which he exclaimed Ars longa Vita Brevis (Art is long life is short), a sentiment redolent of Osuntokun’s own observation that « Excellence lasts for ever ». Although Osuntokun in his life time interacted with many Nigeria’s moguls, he opened the list of his alter egos with Fola Alade. By that gesture, Osuntokun took us back to Christ’s School Ado Ekiti and the halcyon days we passed there. Alade, Osuntokun, myself and a few others belonged to the Francis Adeagbo Boys Club where Prefect Adeagbo took us under his wings and protected us from the buffeting and hectoring of the tyrannical, terrifying senior boys of those days. The « Adeagbo boys » grew up together, playing hard, working hard, getting involved in this and that and constantly striving for excellence in all we did. Soccer was Osuntokun’s best game at school, a sport which brought to the fore his gregarious spirit whenever he was in the company of his football colleagues in the School First Eleven team shown in Fig. 1. Standing in that picture and first on the left is Stephen Faloye, inside left forward and master dribbler from Akure. He was the first of the many Faloyes from Akure to play football for Christ’s School. Vincent Faloye the bespectaled goalkeeper and William Faloye (standing second from left in Fig. 2) played for the school in 1952. 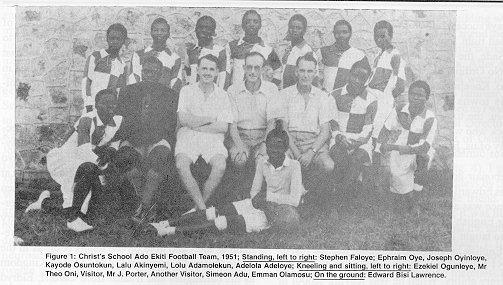 Figure 1 Next to Stephen Faloye was Ephraim Oye who put his facility as the fastest sprinter in the school in 1951 to goo use as a midfield player. Then came Joseph Oyinloye, the thickset ponderous right full back with oak-like legs and a barrel chest. In the centre of the line up was Osuntokun, the centre forward and striker of considerable skill and success. His forte was unleashing terrific shots from just outside the penalty area. His trademark was a scarf tied round his neck and he christened himself Orlando Terror to intimidate the goalkeepers. On his left was Lalu Akinyemi, the fleet-looted outside left whose role model was Titus Okere, Nigeria’s golden boy and outside left of the 1940’s. Next was Lolu Adamolekun, the rather diminutive left full back, a nuisance to his opponents, quick to defending with both feet and given to irritating strikers by his funny noises and unprintable close-ranged utterances. I stood next to him in the picture, the inside forward, having earned my place in the 1951 School Team by successfully captaining Dallimore House Junior Team in 1950 to a resounding Cup victory as a prolific striker and centre forward. I captained the School Team in 1952, sitting second from the left on the right hand of the Principal, Rev. Mason in Fig. 2. 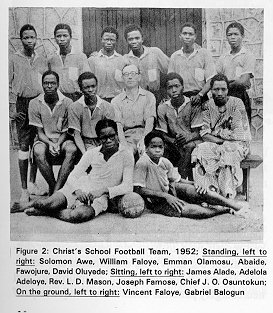 Figure 2 Kneeling and sitting in Fig. 1, first from the left was Ezekiel Ogunleye, one of the half backs. He was resting his body on our Games Master, the late Mr Theo Oni, one time First Master and de facto Deputy Principal of Christ’s School when, as he figuratively and proudly put it « he decided the fate of school boys and teachers alike ». Mr John Porter was fourth from the left. He was Acting Principal for three turbulent months in 1951 when as Rev. Mason later observed, « he ran Christ’s School like a battleship ». Two Europeans who helped to coach us sat on either side of Mr Porter. Then came Simeon Adu, captain of the School Team in 1951, and the outside right forward. His mercurial and sometimes volatile temperament inevitably coloured his game; he left nobody in doubt that he was the captain and to be obeyed. When he was in his element, Adu was an unstoppable attacker, tearing through any defence like a hurricane and drilling the ball past goalkeepers with his characteristic fierce low carpet drives. He always successfully converted penalties with his big broad right foot. Adu was the father of the famous Sade, the singer and artist famed for the album « No Ordinary Love » featuring Sweetest Like a Taboo. Kneeling and resting against Simeon Adu was his towns mate from Ikere-Ekiti, Emman Olamosu, the tough, tenacious and tactical centre halfback who was to be in the School Team longer than any of us, having started from Form III. The debonair goalkeeper, sitting stylishly with the ball was Edward Bisi Lawrence. Lithe and agile, Bisi Lawrence was as good at goalkeeping as he was at writing English essays. He was the School Librarian who taught Ben Oluwole and myself the magic of the English language. Osuntokun, like the rest of the 1951 Senior Class, respected Bisi Lawrence for his literary ability. When he was leaving school in 1951, Lawrence gave me a penguin book on which he inscribed the words of Goethe, the German philosopher, on the aristocracy of knowledge, power and wealth. I never saw Bisi Lawrence again since then, but read his regular essays in the Nigerian Vanguard. He did an article on Christ’s School about ten years ago in which he referred to the Osuntokun Academic Dynasty headed by the late Minister, Chief Osuntokun, our Games Master in 1952 (Fig. 2). It is appropriate that pre-eminent on the list of Osuntokun’s « greatest teachers » are Rev. (later Canon) Leslie Donald Mason, Principal of Christ’s School from 1948 and Chief Joseph Osuntokun, his senior brother and our geographer teacher. Like Paul of Tarsus, Archdeacon Henry Dallimore « planted » Christ’s School, Ado Ekiti, but it was Rev. Mason, gentleman school master from Igbobi, and Master of Arts in Classics who, like Apollos of Alexandria, « watered » the school and transformed it to a modern famous school and one of the best in Nigeria. Chief Joseph Osuntokun saw his junior brother, Kayode, settled into school in 1946 and 1947 before the Chief left Nigeria in September 1947 for Sierra Leone where he spent three academic years to gain the Bachelor of Arts of Durham in record time and added the Diploma of Public Administration as the icing on the cake of his academic success. We were all delighted when the Chief returned to Christ’s School in 1950 as the Geography master for the senior classes of the school. He was a walking Dudley Stamp, a textbook of world geography which he knew almost by heart as we realised when he taught us the geography of the maritime provinces of Canada. We saw from a distance many visitors to the house of our Geography master during the last illness of their father David Osuntokun. He died in 1951 and Kayode shared his grief with me in a poignant poem he wrote in praise of his father. After leaving Ado Ekiti, lawn tennis supplanted soccer as Osuntokun’s favourite sport. One of his playmates who became very close to him was Bayo Akinnola, a Chief of Ondo who was the best man at the grand ceremony on December 15 1962 when Kayode married Dr Olabopo Cameron-Cole, his eternal wife who in the reincarnation, he « will marry again and again and again. » Osuntokun was to remain as alert and able on the tennis court as in the clinic, both in Nigeria and in the United Kingdom as his colleagues and friends from Cardiff, Eldryd Parry and Keith Peters commented in the obituary notice in the Independent of UK of September 30, 1995 (5). Another Ondo close colleague of Osuntokun was Professor Oladipo Akinkugbe whom he succeeded not only as Head of Medicine at Ibadan in 1971 but also as Dean of Medicine in 1974. Akinkugbe, the gentle giant of renal medicine used his dulcet voice and subtle diplomacy to great decisive and manipulative effect in the administration of Faculty of Medicine. It was from him that Osuntokun learnt a lot of finesse in Health Administration that his 1984 Nigeria National Merit Award specially cited and recognised. I last saw Kayode in 1994 at the University of Ibadan post office where we met to collect letters. That venue has become the meeting point for retired employees of the University of Ibadan, many of who have their private letter boxes in the University post office. At our last meeting, we talked about a few things – retirement days; our travels; our families and the death of my father in March 1992. Then we parted, with the promise of meeting again, soon, before resumption of our peregrinations. My last visit to the University College Hospital (UCH) Ibadan took me twenty five years down memory lane to those days when Odeku, Osuntokun and myself used to have our neuroscientific chitchat about our individual assignments and corporate efforts in the definition of neurology and neurosurgery patterns. Osuntokun’s unique ways of announcing his arrival at the hospital was to whistle my name. Nobody else did – or does – that: it is a singular gesture of friendship that I miss. The meetings were held usually in Odeku’s office when inter alia he filled us in on American neurological surgery and the works of Edgar Kahn and Richard Schneider of Michigan. Naturally, our riposte was to talk of neurology and neurosurgery in the United Kingdom: Osuntokun on the works of Henry Miller, John Walton and others of Newcastle-upon-Tyne and I about Valentine Logue, Lindsay Symon and Wylie McKissock of Queen Square London. If Olufemi Williams of Pathology was in his office, on the ground floor of the hospital, he told us his neuropathology news on our patients. Thus, the Sunday meeting was always a learning and lively neuroscientific camaraderie, the genesis of the twelve papers the four of us presented in January 1972 at the Nairobi Symposium on « Tumours of the Nervous System in the African » (6) which Renato Ruberti of Nairobi hosted and after which PAANS was formed (Fig. 3). 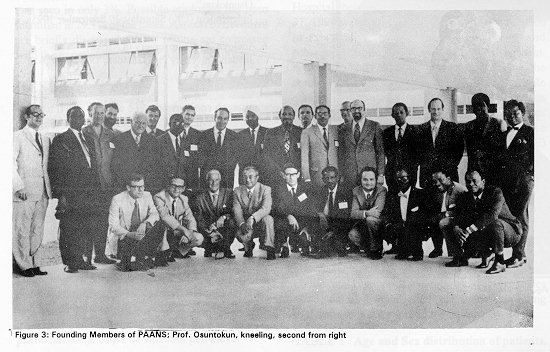 Figure 3 In January 1996, UCH Ibadan was different. The few cars parked in the Consultant park were mostly departmental cars laden with dust of disuse. The first floor of the annex where I had my office was unusually quiet – there were no consultants around doing their paper work. With the entire building wrapped up in such an eerie calm, I could not spend too much time in my office, chock-a-block with books, journals, papers and some memorabilia. After achieving pretty little or nothing, I left and went down to the ground floor. Still, there was no familiar face to see along the Pathology corridor. Then as I was nearing the office of the Chief Medical Director, on a poster to my right was the picture of Osuntokun, life-sized, almost real, in his academic robe and smiling his usual relaxed smile (Fig. 4). I stopped dead, jolted from my absent-mindedness by the sudden appearance of an old and close friend. It was the poster that carried his obituary; it was his farewell and parting shot. It was then that the telephone call I received in Malawi from Professor T. Ige Ade Grillo of Cambridge on September 23 1995 about the death of Osuntokun assumed a merciless reality. I felt a lump in my throat as it dawned on me that Kayode Osuntokun had truly died and passed away. I have had playmates  Figure 4
The paper entitled « The Surgery of Meningiomas: a review of 215 cases » by R.F. Ruberti, Nairobi, Kenya which appeared in a recent issue of « The African Journal of Neurological Sciences », (volime 14, January 1995, pages 10 – 13) makes fascinating reading and represents an invaluable contribution to our knowledge of meningiomas seen in our part of the world of neurosurgery. At a personal level, Professor Ruberti deserves special commendation for his efforts and congratulations on forty years of sustained, active and productive service in the demanding field of neurological surgery in Italy and Africa. His present series compares favourably with those giant past masters of the neurological art such as Cushing, Olivecrona and Zulch as shown in his Table 2 and The review is based on materials collected from fifteen years of practice in Padua, Italy and of a quarter of a century in Nairobi, Kenya. Readers will be better informed if the author can separate the Italian material from that of Africa and subject both the concise clear analysis he has presented for his corporate experience from the cities of Padua and Nairobi. That accomplished, his work can become an authoritative addition to the literature and useful reference on meningiomas in Italy as well as in Africa. Such a contribution will be particularly appreciated and relevant in Africa, where hitherto the extant publications on meningiomas are generally few and relatively old and some made up of inadequatly studied, isolated case reports. Adeloye, 1989.
Articles récents
Commentaires récents
Archives
CatégoriesMéta |
© 2002-2018 African Journal of Neurological Sciences.
All rights reserved. Terms of use.
Tous droits réservés. Termes d'Utilisation.
ISSN: 1992-2647






