
|
|
|
SUMMARY We present a case of a growth hormone secreting pituitary adenoma with successive spinal cord metastasis at 6 and 11-year interval following craniotomy and radiotherapy. The lesions were cervical, thoracic and cauda equina and were successfully surgically removed. The MRI and histological findings are discussed and the literature reviewed. Keywords : Pituitary, Metastasis, Spinal RESUME Les auteurs rapportent un cas d’adenome de l’hypophyse secretant avec des metastases medullaires survenues 6 ans et 11 apres la craniotomie et la radiotherapie. Les lesions medullaires cervicales, dorsales et de la queue de cheval ont ete operees avec succes. Les aspects neuroradiologiques, histologiques, et une revue de la litterature font l’objet d’une discussion. INTRODUCTION Subarachnoid dissemination (1,2,3,4) local invasion and haematogenous spread of pituitary adenoma are recognised presentations though it continues to be one of the most benign tumours of the central nervous system (CNS)6. Varied reports have not shown any preponderance to the histological type (7, 8, 9), non-secreting, prolactinomas, and growth hormone secreting tumours. Intracranial deposits have been reported more frequently 2 and have been managed by local excision where feasible, disseminated disease though is notoriously refractory to treatment dopamine agonists. spinal irradiation, interferon and chemotherapeutic agents have all been tried. CASE REPORT 1st Admission 2nd Admission 3rd Admission DISCUSSION Metastatic pituitary tissue with endocrine function is rare. Biochemical cure following complete surgical resection of spinal canal metastasis lias been described once previously as. The same patient has represented 6 years later in his home country Kenya with a histologically begign tumour in the cauda equina. The patient has survived 12 years since the first onset of symptoms and to date has no evidence of intracranial recurrence of tumour. A mean survival time of 5 years (range of 20 days to 12 years) has previously been reported (2). MRI scanning following resection of lesions in his cervical spine in 1994 did not reveal any other macroscopic deposits in the neuro-axis. Correlation between histological type and preponderance to metastasise has been poor 4,5,1 l,l2 several reports like ours show a histologically begign ‘metastatic’ lesions. Metastasis within the neuroaxis is thought to be via Subarachnoid and haematogenous spread. Surgical intervention within the basal cisterns has been implicated in the potential lor subarechnoid dissemination. Lumbar CSF examination confirming the presence of tumour cells has also been used previously 2. A new histological technique, proliferating cell nuclear antigen (PCNA) has been developed to predict local recurrence in adenomas of the pituitary (13) . This has been used lo determine the proliterative potential of a classic pituitary adenoma which 1’netastasiscd intracranially and has been used to predict aggressiveness of the tumour 14 with variable results. The question of radiation to the tumour remnant being carcinogenic to a previous benign tumour has been deemed as uncommon (15). The management of metastatic pituitary adenoma remains poor: dopamine agonists have been used in the treatment of prolactinomas and somatotrophic tumours (16,17). Whole spine radiation in four parts lias also been used to control spinal dissemination (2) with initial reduction of intracranial and spinal tumour size, there was subsequent regrowth of tumour with fatal consequences. CONCLUSION This is the first case reported in the literature of successive intraspinal growth hormone secreting pituitary adenoma adequately treated by surgical excision. We feel that he is also unique in that he has presented to several units in two continents with good cros references. Metastatic pituitary adenoma though are has such a poor prognosis as to whether consideration for spinal CSF cytology, hormone levels, PCNA analysis of the tumour for reactivity should be done to enable us to predict the cases that are likely to progress. 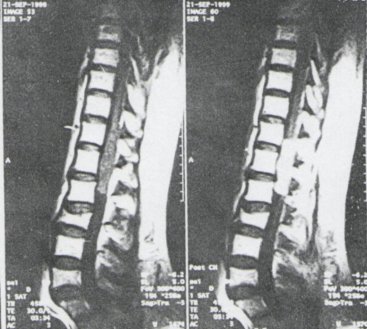 Figure 1
SUMMARY Cerebral hydatidosis is a rare form of hydatid disease of the Central Nervous System accounting for 2 to 3 percent of all cases of hydatid disease. Hydatid disease is a major health problem in certain nomadic communities in Kenya. Treatment is surgical excision of the cyst. A four year old African boy presented with fits, progressive enlargement of the head and right hemiparesis at the Kenyatta National Hospital, Nairobi, Kenya. A computerised tomography (CT) scan of the head showed a large cystic mass in the left parietal area with no associated brain oedema or contrast enhancement. A left parietal craniotomy and total excision of the cystic mass was done. Histology showed laminated wall of cyst of echinococcus granulosus with numerous scolices. Post-operative recovery was good and follow-up has not revealed any evidence of recurrence. Keywords : Cerebral Hydatidosis, Kenya RESUME L’hydatidose cerebrale est observee chez environ 2 a 3% des patients qui presentent une hydatidose. L’hydatidose est un des problemes de sante publique majeur observe au sein de communautes nomades vivant au Kenya. Le traitement est 1’ablation chirurgicale du kyste. Un cas survenu chez un garcon agé de 4 ans ayant des crises d’epilepsies, une macrocephalie et une hemiparesie droile a ete observe a l’Hopital National de Kenyatta a Nairobi. L’examen tomodensitometrique cranien a montre I’existence d’un grand kyste situe dans la region parielale gauche sans oedeme cerebral et sans rehaussement apres injection de produil contraste. Une craniotomie parie’tale gauche a permis 1’excision totale du kyste, avec a l’examen histologique une confirmation de la nature du kyste qui contenait de nombreux scolex. Une regression des signes cliniques est apparue apres 1’intervention sans recidive de l’affection. INTRODUCTION Cerebral hydatidosis is caused by the larval stage of hydatid of the dog tapeworm taenia echinococcus. Hepatic and pulmonary forms of the disease are the most common and account for almost 85% of the cases. CASE REPORT A four year old African male was admitted to the Neurosurgical Unit at Kenyatta National Hospital, Nairobi, Kenya, with a one year history of persistent headache and grandmal seizures. He had previously been admitted and treated in various hospitals elsewhere on several occassions for what was then thought to be attacks of malaria. He was referred to Kenyatta National Hospital from the Kakuma refugee camp where he was On examination, he was found to be sick looking although fully conscious and co-operative. He had marked right side wcakeness with power in the upper and lower limbs reduced to grade 3/5. The deep tendon reflexes were brisk. His head circumference was 56cm. A computerised tomography (CT) scan of the head showed a large cystic mass in the left parietal area, with mass effect. There was no rim enhancement on injection of contrast materia (Fig 1) Blood results were as follows: Liver function tests were as follows: Abdominal ultrasound showed features suggestive of hepatic hydatidosis. Patient was pre-operatively put on albendazole, prepared for surgery and underwent craniotomy under a general anaesthetic. The mass was excised in toto. Histology showed laminated wall of cyst, typical of echinoccocus granulosus with numerous scolices. His post operative recovery was uneventful with good recovery of power on the right side and improvement of his symptoms. DISCUSSION The existence of the hepatic form of hydatid disease was recognised by Hippocrates and Galen in their early writing (2). The first reports of cerebral hydatid disease and vertebral echinococcosis were by Guesnard and Chaussier respectively in 1807 (3). Hepatic and pulmonary forms of the disease arc the most common and account for almost 85 per cent of the cases (4). Cerebral hydatidosis accounts for 2 to 3 per cent of patients. Central nervous system forms of the disease may be cerebral (80 %), cranial (5%) and vertebral (15 %). The ‘usual hostsfor the adult worms are dogs, wolves and foxes. Cattle, sheep and dogs serve as intermediate hosts. In the definite hosts, the scolex attaches to the intestinal mucosa. becomes the adult worm and releases eggs into the faeces of canines. After ingestion of the egg by man, the capsule is digested and hexacanth oncospherc is released in the jejunum where it penetrates the intestinal mucosa and passes into the portal circulation. Most become entrapped in the small intrahepatic venules while others pass to the lungs, central nervous system, bone and other site (1). The embryo, oncospheres, may be destroyed by normal hosts defense mechanisms or may increase rapidly in size and form unilocular cysts. The cyst wall differentiates into an internal granular layer (endocyst) and an outer cuticular laminated layer surrounded by an outer host adventitial fibrous capsule. The cavity of the cyst contains hydatid fluid, daughter cysts, brood capsules and scolices. Brood capsules arise from the germinal layer of the endocyst. Brood capsules and scolices within the hydatid cyst fluid form the hydatid sand (5). Papilloedema is usually present. Seizures are also common. Definitive diagnosis is dependent upon indentification of the parasite or its body parts in the lesion. Successful operative treatment depends upon complete removal of the unruptured cyst. Attempts should therefore be made to remove the cyst in loto. If rupture of the cyst occurs, irrigation with hypertonic salin should be done (7) to destroy the organisms by osmotic dessication. Prognosis usually depends on location and size of the lesion, presence of single or multiple lesions and the presence of contamination. Fortunately cerebral lesion are usually single and accessible. 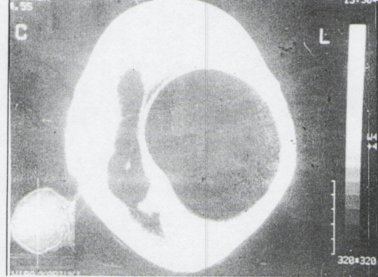 Figure 1
SUMMARY Ventrieulo-periloneal shunt placement is a common operation in the Neurosurgical unit at the Kenyatta National Hospital, Nairobi. The common complications of shunt surgery are infection and obstruction. A case of acute appendicitis following vcntriculoperitoneal shunt placement in a patient with hydrocephalus secondary to an intracranial tumour treated at the Kenyatta National Hospital is presented. Although other intra-abdominal complications such as gut perforation, peritonitis and trans-recta] migration of the peritoneal shunt tip are commonly seen in the unit, acute appendicitis in a patient with ventriculoperitoneal shunt has not been previously reported. While this association may have been incidental it is also possible that the presence of the peritoneal shunt precipitated the attack of acute appendicitis. Kewywords : Hydrocephalus, VP Shunt, Acute Appendicitis RESUME Les derivations ventriculo-peritoneales sont couramment effectuees dans Ie service de Neurochirurgie de l’hopital National Kenyatta a Nairobi. Les complications habituelles d’une telle chirurgie, sont d’ordre infectieux et concernent l’obstruction de la valve. Un cas d’appendicite aigue consecutif a la mise en place d’une telle valve chez un patient ayant une hydrocephalie secondaire a une tumeur intracranienne traitée dans cet hopital est rapporte ici. Les complications abdominales hahiluellement observees sont des perforations aigues, des peritonites ou des migrations transrectales du materiel de prothese mis en place; une appendicite aigue n’a jamais ete constatee. Il est possible qu’il s’agisse simplement d’une association mais il est possible aussi que la presence d’un tel materiel peritoneal ait favorise la survenue d’une appendicile aigue. INTRODUCTION Hydrocephalus is a condition of multiple aetiology in which cerebrospinal fluid (csf) produced in the ventricles of the brain is not absorbed in a normal fashion. This causes enlargement of ventricular system which generally results in intra-cranial hypertension or increase in head size in children. In the paediatric age group, the diagnosis is based on measurement of head circumference, ultra-sound and computed tomography scanning which shows ventriculomegally. Management is placement of shunt diversion system (generally from the ventricles to the abdominal cavity). Die common complications are infection and obstruction requiring reoperation (1). This surgical approach is still standard today. Appendicitis is an inflammation of the appendix and a common cause of acute abdomen. It occurs at any age but is commonest in the younger age group. The classic history is the onset of central abdominal pain. Often associated with vomiting which localizes to the right iliac fossa. Examination may show a distressed patient who is febrile, has a coated tongue with foetor oris and has abdominal tenderness to palpation which is maximal in the right iliac fossa. This is usually associated with guarding and rebound tenderness may be present. A full blood count may show a raised white cell count with a neutrophilia. (3). CASE REPORT A 24 year old African male was admitted to the Neurosurgical unit at Kenyatta National Hospital. Nairobi, Kenya, with a foLir month history of headache, vomiting and blurred vision. Fundoscopy revealed bilateral papilloedcma. His level of consciousness was normal and his memory was not impaired. A part from a slurred speech he had no other neurological defits. A CT scan of the head confirmed a tumour in the pineal region with associated hydrocephalus (figl). DISCUSSION VP shunt placement has the highest incidence of complications of all neurosurgical procedures. Common complications ofVP shunting are obstruction, infection, exit from peritoneal cavity and perforation of viscus. (I). Shunt procedures may be necessary in a patient with an inoperable pinealoma who has ventriculomegally (4). Acute appendicitis is a common cause of an acute abdomen, ll can occur at any age but is commonest in the younger age group. The classic history is the onset of central abdominal pain, often associated with vomiting, which localizes to the right iliac fossa. Common differential diagnosis include pelvic inflammatory disease, mesenteric lymphadenitis, gastroenteritis, Yersinia enterocolitis, urinary tract infection, renal colic, ectopic pregnancy, panacrcatitis, divcrticulitis, mittelschmerz, perforated duodenal ulcer and cholecystitis. Rarer differential diagnosis include Meckel’s diverticulitis, torsion of ovarian cyst and small bowel obstruction. Acute appendicitis following VP shunt surgery is unusual. Other infra abdominal complications such as ascites, intestinal perforation with peritonitis and pscudocyst formation have been reported after VP shunting (1). A disturbance in the blood brain barrier (BBB) seen in patients with intracranial tumours may lead to elevation of csf protein and failure of peritoneal absorption of csf after shunt placement and ascites. Peritoneal metastases may also play a role in the development of ascites associated with medulloblastomas and pineoblastomas. (5). The incidence of shunt infections ranges from 2-27%. The lumen of the appendix may be blocked by a piece of stool, swallowed foreign body or intramural swelling from an infection, resulting in swelling of the whole appendix which becomes prone to infection by bacteria. If the infected appendix is not removed an abscess may form and eventually burst or perforate. Anaerobes which are normal flora of the large bowel, are commonly associated with acute appendicitis. Facilitating pathologic process which may lead to anaerobic infections are compromised vascular system, trauma, tissue destruction and antecedent infections resulting in necrosis. (3). The common pathogen are Bacteroides, Fusobacterium, Anaerobic cocci and Peptostreptococcus. The association between VP shunt placement and acute appendicitis in this patient may have been incidental, However, a low grade shunt infection may cause infection and swelling of the appendix and lead to acute appendicitis. A shunt tube within the peritoneal cavity pressing on the appendix may compromise the vascular system of the appendix and lead to anerobic infection within the appendix and appendicitis. Both these factors may probably have played a role in the development acute appendicitis in this patient. 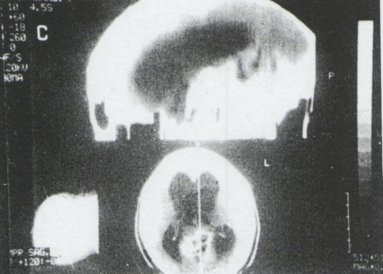 Figure 1
Articles récents
Commentaires récents
Archives
CatégoriesMéta |
© 2002-2018 African Journal of Neurological Sciences.
All rights reserved. Terms of use.
Tous droits réservés. Termes d'Utilisation.
ISSN: 1992-2647


