
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
RESUME Buts La hernie discale lombaire est rare chez l’enfant et l’adolescent. Peu d’études ont été consacrées aux sujets de 18-25 ans. Nous avons voulu identifier d’éventuelles particularités de cette pathologie dans cette tranche d’âge à travers un échantillon pris en charge dans notre service. Matériels et méthodes Il s’agissait d’une étude rétrospective portant sur 52 patients colligés à l’hôpital de Grand Yoff et au CHU de Fann du 1er Avril 2004 au 31 Mars 2009. L’échantillon était représenté par des sujets de 18 à 25 ans, qui avaient consultés pour lomboradiculalgie avec mise en évidence au niveau de l’imagerie d’un conflit disco-radiculaire. Le suivi s’étalait de un mois à 48 mois. Résultats L’âge moyen était de 22,8 ans. On notait une prédominance masculine (86,5%). Les militaires représentaient 38,4%. La symptomatologie a été brutale dans 23,1% suite à un traumatisme. Le bilan radiologique retrouvait 6 cas de canal lombaire étroit et 6 cas d’anomalie transitionnelle associés à la hernie discale. On ne notait pas de signes de dégénérescence discale. L’étage L4-L5 était concerné dans 53,8%. Treize patients ont été opérés avec dans 46,2% des cas une disparition complète de la symptomatologie initiale à un an. Conclusion La hernie discale lombaire de l’adulte jeune est favorisée par les professions de force et les traumatismes du rachis lombaire. Le traitement doit être le plus conservateur que possible même si les résultats de la discectomie sont meilleurs que chez l’adulte plus âgé. Mots clés : Hernie discale lombaire – Adulte jeune. SUMMARY Aims The lumbar disc herniation is rare in children and adolescents. Few studies are devoted to the 18-25 years old. We wanted to identify possible features of this disease in this age group through a sample management in our department. Materials and methods This was a retrospective study of 52 patients, collected inGrandYoff hospitalandatFann Hospital from 1st April 2004 to March 31, 2009. The sample was represented by subjects aged between 18 to 25, who had lombo-radicular pain with a disco-radicular conflict in imagery. The follow up ranged from one to 48 months Results The average age was 22.8 years. There was a male predominance (86.5%). The soldiers represented 38.4%. The symptoms were sudden in 23.1% following trauma. Radiological assessment found 6 cases of spinal stenosis and 6 cases of transitional anomaly associated with the herniated disc. No signs of disc degeneration. The L4-L5 level was involved in 53.8%. Thirteen patients were operated and in 46.2% of cases a complete disappearance of the initial symptoms one year. Conclusion Lumbar disc herniationin young adultsis favoredby the professionsof forceand traumaof the lumbar spine. Treatment shouldbe asconservative as possibleeven if the resultsofdiscectomyare better thanolderadults. Key words:lumbar disc herniation-youngadults. INTRODUCTION La hernie discale lombaire est rare chez l’enfant et l’adolescent dominée par les causes traumatiques et l’activité sportive (10, 14, 22). Le traitement est le plus souvent conservateur avec cependant de meilleurs résultats chirurgicaux que chez l’adulte (4, 27). Entre l’adolescence et l’adulte âgé où domine la cause dégénérative, très peu d’études se sont consacrées aux sujets de 18 à 25 ans (15, 25). Nous avons voulu identifier d’éventuelles particularités cliniques, étiologiques et évolutives de cette pathologie dans cette tranche d’âge à travers un échantillon pris en charge dans notre service. MATERIELS ET METHODES Il s’agissait d’une étude rétrospective portant sur 52 patients, colligés à l’hôpital Général de Grand Yoff (HOGGY) et à l’Hôpital de Fann du 1er Avril 2004 au 31 Mars 2009. L’échantillon était représenté par des sujets de 18 à 25 ans, qui avaient consultés pour lomboradiculalgie avec mise en évidence au niveau de l’imagerie d’un conflit disco-radiculaire. Le bilan radiologique était constitué par les radiographies standards du rachis lombaire, le scanner et l’IRM. Le suivi s’étalait de 1 à 48 mois. Nous avons évalué le résultat fonctionnel à un an en classant les patients en 3 groupes en fonction de la reprise du travail : -Une bonne évolution avec disparition complète de la symptomatologie et reprise du poste antérieur. -Un groupe intermédiairerépondant aux critères suivants : lombalgie résiduelle, reprise du travail mais reclassement dans un autre poste. -Une mauvaise évolution avec persistance de la sciatalgie et arrêt plus ou moins prolongé du travail. RESULTATS Pendant la période d’étude, 5672 personnes avaient consulté pour lombalgie ou lomboradiculalgie dont 83 âgés de 18 à 25 ans (1,5%). Il a été diagnostiqué une hernie discale chez 52 patients dans cette tranche d’âge. L’âge moyen était de 22,84 ans. On notait une prédominance masculine (86,5%). Les militaires représentaient 38,4% des professions de nos patients (tableau 1). La symptomatologie a été brutale dans 23,1% suite à un effort ou à un traumatisme et progressive dans 7,7% faite de lombalgie chronique. Les motifs de consultation étaient dominé par la lombalgie (76,9%) et les lomboradiculalgies (46,1%) (tableau 2). La TDM (100% des patients) et l’IRM (44,2%) retrouvaient 2 cas d’arthrose inter apophysaire postérieure étagée, 6 cas de canal lombaire étroit constitutionnel, et 2 cas de spondylolisthésis associés. On ne notait pas de signes de dégénérescence discale (pincement discal, vide discal). On notait dans 6 cas (11,5%) une anomalie transitionnelle. L’étage L4-L5 était concerné dans 53,8%, L5-S1 dans 38,5% cas et L3-L4 dans 7,7% des cas.La hernie discale était médiane dans 53,8%, latérale dans 30,8% cas et exclue dans 15,4%. Un traitement médical a été institué dans tous les cas pendant 2 à12 semaines. Aucun de nos patients n’a bénéficié d’infiltration épidurale. L’indication chirurgicale était posée chez 13 patients (25%) après échec d’un traitement médical de 3 à 6 mois; en cas d’apparition ou d’aggravation secondaire d’un déficit. Ceci représentait 3,2% de l’ensemble des discectomies réalisées pendant cette période. Tous les patients avaient bénéficié d’une discectomie par un abord inter-lamaire. Le taux de suivi de tous les patients était de 76,9%. Pour les patients opérés, l’évolution était satisfaisantedans 6 cas (46,2%), acceptable dans 2 cas (15,4%) et mauvaise dans 2 cas (15,4%). Aucun patient n’a été réopéré. Les autres patients avaient bien répondu au traitement médical et à la kinésithérapie. DISCUSSION Notre échantillon (52 patients) représentait la proportion des 18 -25 ans chez qui a été posé le diagnostic de hernie discale lombaire (1,5%). Ceci est dû à notre stratégie diagnostique qui consistait à ne demander les explorations radiologiques qu’en cas de persistance d’une lomboradiculalgie après un traitement médical initial de 2 semaines. L’échantillon aurait probablement été beaucoup plus important si une TDM lombaire avait été demandée de façon systématique. On notait une prédominance masculine (86,5%) comme Pietila( 16) sur une population de 14 à 25 ans, avec un sexe ratio 1,71/1. Il faut noter cependant que chez les moins de 16 ans, certains auteurs retrouvaient plutôt une prédominance féminine; la prédominance masculine n’apparaitrait qu’au-delà de 17 ans (17, 20). Cette distribution serait due à la croissance plus rapide des filles pendant l’adolescence, ce qui les rendrait plus vulnérable aux microtraumatismes du disque intervertébral que les garçons(24). Plusieurs facteurs ont été évoqués pour expliquer la survenue de cette pathologie chez les adolescents et les enfants. Parmi ces facteurs il faut citer les antécédents familiaux (frères et parents)de hernie discale lombaire (12)et le traumatisme lombaire. Le traumatisme, qu’il soit violent ou fait de microtraumatismes répétés par exemple lors de l’activité sportive est incriminé dans la survenue de la hernie discale dans cette tranche d’âge (2, 10, 17, 20). Il faut aussi citer la surcharge pondérale qui est un facteur reconnu quel que soit l’âge (2, 16). Les professions de force (militaires, chauffeur et maçon qui représentaient près de 85% de notre série) pourraient favoriser la survenue de cette affection. En effet ces professions sollicitent de façon importante le rachis lombaire (1, 26). Dans la population pédiatrique et l’adolescence, les signes cliniques de la hernie discale ne sont pas spécifiques, dominés par le syndrome rachidien avec rareté des signes neurologiques (7, 11, 23). Dans notre série, nous n’avons retrouvé aucune particularité clinique par rapport à l’adulte plus âgé. La stratégie des explorations complémentaires reste généralement à l’appréciation du clinicien et n’est pas codifiée. La bénignité de la hernie discale chez les sujets jeunes autorise à être un peu attentiste, mais le risque de passer à côté d’une affection grave (infectieuse dans notre contexte) plus fréquente à cet âge pourrait amener à recourir rapidement aux explorations radiologiques notamment l’IRM. Il faudrait donc un juste équilibre en s’aidant surtout de la clinique à la recherche systématique des signes associés. Les radiographies standards du rachis sont plus contributives chez les sujets jeunes que chez l’adulte montrant fréquemment des anomalies transitionnelles et les déformations rachidiennes en particuliers la scoliose (10, 16). L’analyse des images TDM et IRM doivent être rigoureuse pour éviter le piège des protrusions discales quasi constantes chez le sujet jeune du fait de la richesse en eau du nucléus (10). Quel que soit l’âge, les niveaux L4-L5 et L5-S1 sont les plus fréquemment touchés (10, 16, 26). Sur le plan topographique, les hernies sont aussi bien médianes que postéro-latérales (10, 26). Les signes de dégénérescence discale sont par contre peu fréquents même s’ils sont présents à histologie (3). Le traitement médical doit être de première intention surtout chez le sujet jeune pour éviter les troubles de la statique rachidienne ultérieure (8, 15, 18, 25) même si la plupart des auteurs rapportent des meilleurs résultats de la discectomie chez les enfants que chez l’adulte (8, 10). Nos patients opérés représentaient 3,2% de l’ensemble des discectomies pendant la période ; ce qui est comparable au chiffre de Pietila (2,3%) (16) dont les caractéristiques de l’échantillon sont proches du nôtre. Chez les adolescents ce taux se situerait entre 0,5 et 7% selon les études (8, 14). Les patients opérés représentaient 25% de notre échantillon. Ce pourcentage est important par rapport à ceux rapportés chez l’adulte plus âgé. Chez les adolescents, ce taux peut atteindre 50 à 60% dans certaines séries (9, 27). La durée moyenne du traitement médical avant l’indication de la chirurgie dans notre série variait entre 3 à 6 mois. Plusieurs tests sont utilisées pour évaluer les résultats de la chirurgie de la hernie discale (1, 5, 25). Nous avons utilisé un critère basé sur la reprise de l’activité professionnelle. Pour les patients opérés, nous avons eu de bons résultats dans 46,2% des cas contre 15,4% de mauvais résultats. Pietila retrouvait 35,1% de bons résultats. Chez l’enfant et l’adolescent ce taux varie entre 88 et 96% (15, 19, 21). Le taux de ré intervention (15%) serait semblable à celui de l’adulte (13, 21). Le temps de suivi moyen des patients opérés (1 an) n’a pas permis d’apprécier les conséquences de la discectomiesur leur statique vertébrale. CONCLUSION La hernie discale du sujet jeune est peu fréquente souvent favorisée par les traumatismes. Il existe des facteurs favorisants tels que la profession ; et la prédisposition génétique rapportée par certains auteurs. Les modalités cliniques se rapprochent de celles de l’adulte âgé. Le traitement doit être le plus conservateur que possible même si les résultats de la discectomie sont meilleurs que chez l’adulte. Tableaux Tableau 1 : répartition des patients selon la profession.
Tableau 2 : les principaux signes cliniques.
Background: Studies have reported sex differences in stroke risk factor, presentation, morbidity and mortality. This study aims to determine the effect of sex on morbidity and 30-day fatality in patients with acute stroke. Methods: Ninety-one patients were recruited for the study. We documented sex differences in stroke presentation, stroke severity on admission and discharge, and 30-day in-hospital fatality. Continuous variables were assessed using the student t-test. While outcome measures were analysed using the logistic regression analysis. Conclusions: Sex differences in outcome exist in this study and women appear to have a poorer stroke outcome, more studies are needed to assess sex differences in response to therapy. Key words: blacks, outcome, sex, stroke. INTRODUCTION Stroke is a leading cause of long-term disability, (1) and the second most common cause of death worldwide, accounting for about 8% of total deaths in developing countries. (5) Men have a higher incidence of stroke, but women appear to have more severe strokes and a higher case fatality. (3) This has lead to an increasing concern for women with stroke with the Go red for women’ campaign, due to the increasing burden and uniqueness of stroke in women. (37, 8, 45, 13, 24, 10) Studies have reported sex-specific differences in stroke aetiology (37, 13, 24), presentations (45, 26, 44), diagnosis (39, 34, 47), treatments (13, 39, 36, 22) and outcomes (8, 13, 43, 19, 12). Reports have shown that women hospitalized for stroke were less likely to be investigated (34, 47), have a carotid endarterectomy (34), or receive thrombolytic therapy. (13, 36, 40) While some studies are in agreement that women have more severe strokes and a lower quality of life than men (39, 43, 24, 38), others are in disagreement. (19, 17, 35) Studies on sex difference in stroke mortality have been variable, some studies reported a higher mortality in women (24, 38, 4, 11), others reported a higher mortality in men (16, 42) and other studies reported no significant sex difference in stroke mortality (8, 19). These varying differences in mortality may be due to patient’s characteristics and how stroke and mortality are defined. (42) Reasons proposed for poorer outcomes in women include, older age and comorbidities; (24, 11) differences in acute stroke management; (8, 13, 34) and poorer functional recovery at rehabilitation. (33) Experimental studies are postulating cellular and pathophysiological basis for these sex differences, (25, 27) which is a subject for further researches. Based on the above observation we sought to determine sex differences in stroke morbidity and mortality, as such differences may provide an opportunity for improved patient care. MATERIALS AND METHODS The study cohort was 91 stroke patients admitted through the accident and emergency unit or the neurology clinic of the University of Maiduguri Teaching Hospital (UMTH), North-eastern Nigeria. Stroke was clinically defined by the WHO criteria as rapidly developing clinical sign of focal and/or global disturbance of cerebral function, with symptoms lasting twenty-four hours or longer or leading to death with no apparent cause other than of vascular origin. (50) During the five year period (2005-2009), two hundred and eighty-five (285) suspected stroke patients were attended to; one hundred and ninety-four patients were excluded from the study. Those excluded from the study were patients who had no computerized tomography (CT) or magnetic resonance (MRI) scan of the brain, those with a diagnosis of subarachnoid haemorrhage, subdural haematoma, those who died within 24hrs of admission and those with a past history of stroke. (Figure 1) All patients had an oral or written consent; consent was interpreted to some subjects into the local dialect for better understanding. History and examination was conducted and documented in the UMTH stroke proforma which included age and educational level. Risk factors for stroke such as hypertension (current blood pressure values 140/95 mmHg or features of long standing hypertension), atrial fibrillation (AF) (electrocardiographic evidence), transient ischaemic attack (TIA), diabetes mellitus (DM), smoking, alcohol consumption and a diagnosis of Human immunodeficiency virus (HIV) infection were recorded, this has been stated in an earlier study. (48) Medications taken by the patients before the stroke were also noted. Level of consciousness evaluated by the Glasgow Coma Score (a GCS < 8 is taken as coma). The distinction between ischaemic and haemorrhagic stroke was determined by CT or MRI. Patients with ischaemic stroke were categorized into; Total anterior circulation stroke (TACS), Partial anterior circulation stroke (PACS), Posterior circulation stroke (POCS) and Lacunar stroke. Stroke severity was assessed using the National Institutes of Health Stroke Scale (NIHSS). Disability and handicap were rated using the modified Rankin scale (mRS) and the Barthel ADL index (BI). These measures were also assessed at the time of discharge as outcome measures. The mRS identifies at a glance stroke disability, the BI assesses activity of daily living, but weighs heavily on motor functions, while the NIHSS provide the most prognostic information. (29) Duration of hospital stay was recorded only for those who survived till time of discharge. Death within 30 days attributable to the stroke was recorded from date of stroke admission. All the above data were categorized based on sex. Statistical Analysis Student’s t-test and the Z-test were used to assess continuous variables. The BI and the mRS were dichotomized for logistic regression analysis. The selected categories were severe stroke on admission (BI < 45 and mRS > 4), Poor ADL Status on discharge (BI < 45), independent on discharge (mRS <1 and BI > 90), and 30-day fatality was evaluated in a logistic regression analyses, controlling for age and clinical variables, these results were expressed as odds ratios (ORs). All statistical data were analyzed using SPSS (version 16.1) software. RESULTS During the five year period 285 patients had a diagnosis of suspected stroke, 194 patients were excluded from the study as shown in Figure 1. Ninety-one patients were registered for the study. All recruited patients were blacks residing in Nigeria. There were 61 men (67%) and 30 women (33%), mean age of 56.2 +11.1 and 55.6 + 12.4 years in men and women respectively. Compared to men, women were less likely to be formally educated (P = 0.024). Table 1 shows stroke subtypes. There was no statistical difference in stroke subtype; as 25 (83.3%) women compared with 48 (78.7%) men had CT evidence of infarction (P=0.812), while 5 (16.7%) women compared with 13 (21.3%) had haemorrhagic stroke (P = 0.812). Lacunar stroke was more common in men (P = 0.048), with no significant difference in other syndromes of ischaemic stroke. Men were more likely to take alcohol (P = 0.027) and to smoke (P = 0.046). There was no significant sex difference in other risk factors when comparing history of hypertension, DM, TIA, AF, HIV infection. Men were more likely to be treated with antihypertensives compared with women (P = 0.036) There was no significant difference in the use of diabetic, antiplatelet and lipid-lowering medications (Table 1). From the logistic regression in Table 2, women were about five times more likely to have severe stroke on admission (BI < 45, OR = 5.30; 95% CI, 1.10 to 25.62 and mRS > 4, OR = 5.38; 95% CI, 1.53 to 18.96), about four times likely to have a poor functional status on discharge ( BI < 45, OR = 4.40; 95% CI, 1.45 to 13.35) and twice as likely to die from stroke within 30 days of admission (OR = 2.19; 95% CI, 0.72 to 6.65). Urinary tract infection (UTI) was commoner in women (P = 0.023), with no major difference in other stroke complications (Figure 2). There was no sex difference in duration of in-hospital stay. (P = 0.168) Table 3, shows the summary of significant differences. DISCUSSIONS These data provide an evidence of differences by sex of stroke presentation and outcomes. This study shows that women were less likely to be educated, to smoke or to take alcohol. Women were however more likely to present in coma, and have to a more severe stroke at presentation. Women were also more likely to be disabled and to be handicapped on discharge. Despite the higher likelihood of men receiving antihypertensive medications prestroke, they still had a higher DBP on admission. This may be a reflection of the general lack of optimal BP control among hypertensives in the African subregion (7, 31). Although, there was no sex difference in hypertension as a risk factor in this study; studies have shown that women were more likely to be hypertensive, (22, 2, 51) though this may not be so in black Africans with stroke. In the study by Andersen et al (2), they reported that hypertension was slightly more prevalent in men below the age of 50 years, after which the prevalence increased in women. Since our patients are younger we may not have similar findings. We found no significant difference in risk factors such as DM, TIA and AF. Findings from other studies showed that women were more likely to have hypertension and AF (8, 13, 38, 11, 16), while men were more likely to have DM and heart disease (11, 16). Our finding of more frequent alcohol intake and smoking concurs with reports from other studies (8, 13, 11). Our study showed that men were more likely to be on antihypertensives prestroke, and no sex difference in the use of lipid lowering, antiplatelets or antidiabetic medications. Our observation is divergent to the studies showing that women were more likely to have treatment of high blood pressure prestroke (31, 9). The study by Smith et al (44) showed that women were more likely to be treated with antihypertensives, and less likely to receive antidiabetic, antithrombotic and lipid-lowering medications during the course of stroke treatment. The study by Khan et al, (22) is also in agreement that women were more likely to receive antihypertensive after a stroke. Report by Bushnell et al (6) on the use of statins showed that there was no sex difference in the use of statins or any statistical interaction between the effects of sex and statin use on the risk of stroke. In our study lacunar strokes were commoner in men; this is congruent with a study by Foster et al (10) and divergent to some studies that reported lacunar strokes occurring more frequently in women with TACS. (44, 39, 35) Women were reported to be older in several studies, (45, 13, 10, 44, 11) but this is not so in our study. The Framingham study (35) observed that women developed stroke an average of 5 years later than men. This difference in our study may be due to the relatively younger age of our cohort, smaller number of women participants and women in our community are less likely to seek medical attention early due to socioeconomic reasons, this may influence poorer outcomes and not reach the hospital alive. (32, 20, 49) The women in this study were less likely to be educated compared to men; it has been shown that level of education influences socioeconomic status. A lower socioeconomic status not only increases the likelihood of having a stroke (20), but also impacts negatively on stroke presentation and care. (52) Although other reports have shown no differences in stroke severity and case fatality rate (10, 17, 35); this study is in agreement with studies done elsewhere indicating that women were more likely have a severe stroke on admission and have worse outcomes after stroke, women were more likely to be disabled and handicapped on discharge, less likely to achieve activities of daily living independence and have a poorer quality of life. (8, 39, 43, 12, 24, 15) An excess of lacunar strokes in this study may contribute to the better outcome in men compared to women. A study by Sacco et al (41) observed that patients with lacunar stroke have a better outcome compared to those with nonlacunar strokes. In keeping with a more severe stroke women were more likely to be comatose at presentation compared to men, as reported by Gall et al (11). Gargano et al (14) showed no sex difference in patients presenting with coma, but asserted that delay in presentation to the emergency room may explain some of the differences in symptoms. Our study showed that women were twice as likely to die within thirty days from a stroke. This is consistent with some reports, (38, 11) but at variance with other studies. (8, 13, 10, 19) There are other studies that have shown lower rates of mortality in younger women than men and higher number in older women where the absolute burden of stroke is greater (24, 4). The higher mortality in women in other studies, were attributed to increasing age, a higher stroke severity and lower quality of care in women compared with men. (38, 4) There was no significant difference in the duration of hospital admission; this is congruent with a study by Zhu et al (53) who reported no sex difference in length of hospital stay. In our study UTI was commoner in women, and is in accordance with other studies. (13, 39) Studies have shown that women were less likely to be investigated or treated with thrombolytics, (8, 13, 39, 47), but it is not universal. It is interesting to note from studies by Kent et al (21) and Sacco et al (40) that women were more likely to benefit from thrombolytic therapy. This may be an area of further research in our environment. Gargano et al (13) in their study explaining why women were less likely to be treated argued that women were older than men and this influences management owing to comorbid conditions. Women are less likely to have surgical interventions like carotid endarterectomy. (34) A study by Tell et al (46) observed that men were more likely to have carotid atherosclerotic disease than women, and may explain why men have higher endarterectomies. Studies have postulated why women are likely to have severe stroke; Women brains are more likely to produce a stronger and more sustained inflammatory response compared to that of men in animal studies, consistent with increased immune responses (25, 27). In an experimental study with rats reported that oestrogen offers some neuroprotection in neuronal injury and this may be lost as women become older, (28) others have postulated the role of parity and increasing parity with increased mortality from both Ischaemic and haemorrhaghic stroke. (30, 18, 23) The small sample size is a limitation of this study. We did not consider sex differences in recognition of stroke symptoms; as this may influence presentation and subsequent care. We also did not consider sex related effect of stroke care. CONCLUSION This study reveals sex differences in stroke presentation and outcome among Nigerians. After adjusting for cofounding variables we observed that women have more severe stroke on admission, and were more likely to be disabled and handicapped on discharge. In keeping with a severe stroke, they were more likely to be in coma on admission. Women were twice more likely to die from a stroke. ACKNOWLEDGEMENTS We acknowledge the contributions of Dr. A. Ahidjo of the radiology department and Dr. AA Gadzama of the Chemical pathology department. 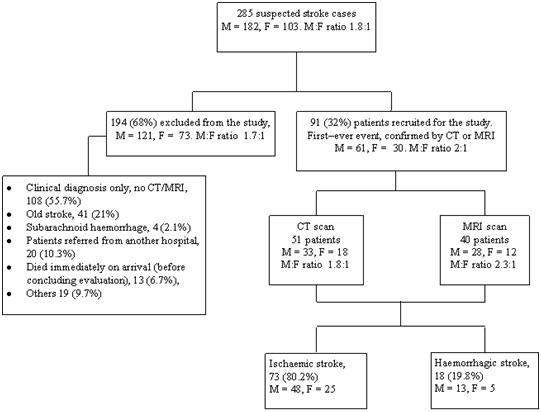 Figure 1. Inclusion and exclusion criteria, diagnosis and type of stroke. (48)
TABLE 1. COMPARISON OF DEMOGRAPHIC AND CLINICAL CHARACTERISTICS OF SUBJECTS BY SEX
TACS – total anterior circulation stroke, TABLE 2: INDEPENDENT PREDICTORS OF STROKE SEVERITY, DISABILITY AND 30-DAY MORTALITY AMONG FEMALE SEX.
Logistic regression analysis of variables, * P < 0.05 Table 3. Summary of significant differences
NIHSS – National Institutes of Health Stroke Scale.
ABSTRACT Background Epilepsy is characterized by episodic and unpredictable seizure recurrences which are often amenable to medical treatment. Simple and readily available medications can be used to control seizures in epilepsy. However, in many communities in developing countries seizure control among people living with epilepsy is still poor. Method We assessed the patterns of antiepileptic drug use and seizure control among persons living with epilepsy in a suburban community in Southeast Nigeria found in a two phase cross-sectional study. Detailed information on epilepsy treatment, seizure control and patterns of antiepileptic drug use (AED) by those diagnosed with epilepsy was determined by use of a semi-structured interviewer administered questionnaire. Further verification of the type of antiepileptic drugs (AEDs) was done by drug inspection. Result The total of 29 cases of active epilepsy comprising 16 (55.2%) males and 13 (44.8%) females were found. Those receiving AEDs at the time of survey were 7 (24.1%), 11(37.9%) who had previously used AEDs had stopped and the remaining 11 (37.9%) were AEDs naïve. Carbamazepine monotherapy was used by 57.1% (n=4) while phenobarbitone was used by 42.9% (n=3). The antiepileptic drugs were prescribed in all these cases by medical personnel. Over 82% of the persons with active epilepsy found were having more than one seizure per month. Conclusion Active epilepsy was prevalent in this suburban community with only 24.1% (n=7) of them receiving treatment with AEDs. Seizure control was poor even among those receiving AEDs and carbamazepine monotherapy was most commonly used AEDs. Keywords – Active epilepsy – Antiepileptic drugs -Seizure control. INTRODUCTION Epilepsy is one of the world’s most prevalent non-communicable diseases with about 80% of the estimated 50 million people living with epilepsy residing in developing countries (20). Epilepsy is characterized by episodic and unpredictable seizure recurrences and these results in immense psychosocial consequences for sufferers and relatives alike. Despite these consequences, the overall prognosis of epilepsy remains good. Often time epilepsy is amenable to medical management with simple and readily available medications. The goal of treatment is to maintain a normal lifestyle by complete seizure control with minimal side effects. Treatment is with pharmacological and non pharmacological methods. Antiepileptic drug (AED) therapy is the mainstay of treatment for the majority of patients. The selection of an AED is based on efficacy against specific seizure types and the adverse effect profile. Non-pharmacological strategies are primarily reserved for drug-resistant epilepsy. If the seizures are provoked by external factors, for instance sleep deprivation or excessive alcohol, simple avoidance might be sufficient to prevent further attacks. AEDs are highly successful in suppressing seizures in most patients. With correct, early and uninterrupted therapy, up to 75% of patients with epilepsy eventually become seizure free, many of them within 5 years after diagnosis (3) while about 25% of patients may not respond to any kind of therapy (3). AEDs differ in many important aspects including their efficacy against different seizure types, their side-effect profiles, their potential for pharmacokinetic interactions, and their ease of use. Several antiepileptic drugs exist, these include the older antiepileptic drugs generally regarded as ¡°old¡± or ¡°established¡± AEDs (carbamazepine, phenobarbitone, phenytoin, valproic acid, e.t.c) and the newer antiepileptic drugs (vigabatrin, lamotrigine, felbamate, gabapentin, topiramate, e.t.c). Except for a better side effect profile, there are no convincing data to show that newer drugs compared with older ones, achieve superior seizure control (3). Older AEDs have several advantages including long-term experience, lower cost and known efficacy. The AEDs most frequently prescribed in the developing world are phenobarbital and phenytoin, (6) they are the cheapest and are prescribed in 65-85% of cases (6). Initiation of therapy for newly diagnosed patients is with a single antiepileptic drug. Combination therapy is recommended when two successive AEDs given as monotherapy have failed. Agents with a low risk of pharmacokinetic interactions are preferred for combination therapy and success of combination therapy can be improved by paying attention to mechanisms of action and using lower dosages (2). With correct, early and uninterrupted therapy, up to 75% of patients with epilepsy eventually become seizure free, many of them within 5 years after diagnosis (3). About 25% of patients may not respond to any kind of therapy. Antiepileptic drugs (AEDs) are highly successful in suppressing seizures in most patients. MATERIAL AND METHODS Study area: The study was conducted in Ukpo an Igbo speaking community in Southeast Nigeria. Ukpo is the headquarters of Dunukofia Local government area in Anambra State Nigeria. The population of Dunukofia local government according to the 2006 National population census report is 96,517 and it has 20,708 households by ownership status of dwelling units (11). The people of Ukpo are predominantly subsistent farmers and they also trade on farm produce. There are a few civil servants under the school system and the Local government employment. The major religion of the people is Christianity with few who are still adherents of Africa traditional religions. The people are acquainted with orthodox treatment since the establishment of a health clinic in the community in the Eastern region of Nigeria. This together with the advent of Christianity had not succeeded in modifying much of the cultural beliefs and practices about epilepsy. This health clinic came under the management of Nnamdi Azikiwe University Teaching Hospital (NAUTH) in 1997 and it became a centre for medical student training in community medicine and recently has become the epicenter of the Neuro-epidemiology and Community Neurology centre of the Neurology unit of the Department of Medicine, Nnamdi Azikiwe University. In addition there is another health centre and two maternity homes and a handful of patent medicine stores in the community but no pharmacy store. Drugs are sourced from these patent medicine stores or the pharmacy sections of the health centers and from pharmacies in neighboring communities. THE SURVEY The study was a two phase cross-sectional descriptive study. The first phase was preceded by a census of households. Household interviewed were selected using computer generated random numbers. Every member of a selected household was interviewed. A total of 6800 persons from 1700 households in the community were selected and interviewed in the first phase taking into consideration the design effects and epilepsy prevalence. The first phase of the study was a door-to-door using a modified version of the WHO protocol (15) for detecting the presence of neurological diseases in the community which was forth and back translated into the local vernacular of the community. This protocol was validated in the area and found to have a sensitivity of 100% and specificity of 65% for active epilepsy. In the second phase all those identified as possibly having epilepsy were evaluated by neurologists and senior residents in neurology. Epilepsy was diagnosed based on the ILAE guidelines (9) and electroencephalogram (EEG) was done in for 19 (65.5%) of the persons with active epilepsy. Detailed information on epilepsy treatment, seizure control and patterns of antiepileptic drug use was determined by use of a semi-structured interviewer administered questionnaire. Further verification of the type of AEDs was done by drug inspection. Ethical approval for the study was obtained from the Ethical Committee of the Nnamdi Azikiwe University Teaching hospital Nnewi and permission to conduct the study from the Ministry of Health Anambra State, Nigeria. Informed consent was obtained from the traditional ruler and his council, from household heads and adults subjects and from parents or close family relatives of children. All the subjects gave their consent. Parents or close family members acted as proxy for Children and persons unable to understand and respond to the questions during all the phases of the survey. STATISTICAL ANALYSIS Data collected was entered into the research instrument and confidentiality maintained. Data collected was analyzed using Statistical Package for the Social Sciences SPSS version 15 (SPSS Chicago Inc., IL, USA). Prevalence values with their 95% confidence intervals were calculated, relevant percentages, frequencies, means and standard deviation were calculated. Fisher’s exact test was used to compare percentages where necessary. Findings were represented with relevant tables. LIMITATIONS The analysis of antiepileptic drug use was restricted to those on AEDs at the time of survey whose drug type and dosage regimen were verifiable. RESULT In the first phase of the study 6800 persons were screened that included 3249 (47.8%) males and 3551 (52.2%) females. Seventy six persons were identified at the first phase as possibly having epilepsy. At the second phase 29 persons were found to have active epilepsy giving a prevalence of 4.3 per 1,000 (95% CI: 2.7 – 5.9). The identifiable seizure types on clinical assessment were generalized seizures 62.1% (n=18) and partial seizures 37.9% (n=11). The patterns of AEDs use is shown in Table 1. At the time of study 24.1% (n=7) of the persons with active epilepsy were receiving AEDs, while 37.9% (n=11) of the persons with active epilepsy who had previously use AEDs had stopped. The remaining 37.9% (n=11) had never been treated with AEDs. AEDs monotherapy was used by all the subjects (100.0%) still receiving AEDs at the time of survey and these were prescribed by medical staffs (medical doctors). Carbamazepine was used by 57.1% (n=4) and phenobarbitone by 42.9% (n=3) of the persons with active epilepsy. The duration of seizures and seizure frequency are shown in Table 2. The mean duration of seizures for patients with active seizure was 6.07 ± 4.6 years. The duration of seizure was 5 years or less for 58.6% (n=17) of the persons with active epilepsy. The seizure frequency was more than one seizure episode per month for 82.8% (n=24) of cases of active epilepsy and less than one seizure episode per month for the remaining 17.2% (n=5). There was no statistically significant difference (P>0.05) in seizure episodes between those on AEDs and those not receiving AEDs (Table 3), this also applied to the difference in seizure types and the type of antiepileptic drug prescribed (Table 4). DISCUSSION Epilepsy one of the most common chronic neurologic diseases the world over is amenable to medical treatment. This study concerned a population sample representative of the Ukpo community in Dunukofia local government area of Anambra state Nigeria. The prevalence rate of 4.3 per 1,000 (95% CI 2.7-5.9) found in this present study was lower than 5.3/1000 and 37/1000 reported by Osuntokun et al (14, 15) in Igbo-ora and Aiyete Southwest Nigeria respectively and 6.2/1000 by Longe and Osuntokun (10) in Udo Southsouth Nigeria. However Osuntokun et al (14) had acknowledged that the existence of health facilities in Igbo-Ora would have contributed to the lower prevalence of epilepsy in Igbo-ora compared to Aiyete which was only 20KM away. The established health care facilities spanning for over more than four decades now in Ukpo might account for the low prevalence in this present study. Furthermore the point in time of this study and difference in the definition of active epilepsy between the present study and that of Osuntokun et al (14) might also be contributory. Simple and readily available medications can be used to control seizures in epilepsy. Up to seventy five percent of patients with epilepsy will eventually become seizure free within 5 years of diagnosis (3) while about 25% of patients may not respond to any kind of therapy (3). In our study the percentage of persons with active epilepsy using antiepileptic drugs at the time of survey was 24.1% (n=7). This is comparable to 27.5% found by Aziz et al (1) in Urban Pakistan. However at Igbo-ora a suburban community that is comparable to Ukpo, Osuntokun et al (14) reported that 4% (n=4/101) were not on AEDs. This was about three decades ago. During door to door surveys the percentage of persons with active epilepsy on AEDs had varied between studies conducted in the developing countries and between communities within the same country. In a community study in Turkey, Aziz et al (1) found that 30% of the epileptic population was on AEDs. The percentage of people living with epilepsy (PWE) on AEDs is less in studies conducted in rural communities. Aziz et al (1) reported 1.9% in rural Pakistan while Dent et al (5) reported 4.2% in a rural community in Southern Tanzania. The AEDs that the patients were using at the time of the study were carbamazepine (57.1%) and phenobarbitone (42.9%). Prior to the study, three persons had used phenytoin. Phenobarbitone and/or phenytoin were used by the persons with epilepsy found by Osuntokun et al (14) at Igbo-ora and Dent et al (5) in Southern Tanzania. Phenobarbitone has been successfully used to treat epilepsy by primary health workers in rural Africa (21). Phenobarbitone is recommended by the World Health Organization (WHO) as the drug of choice for management of seizures in developing countries (8). Previous studies had noted phenobarbitone and phenytoin to be the most often prescribed AEDs in the developing world, the two drugs being the cheapest were prescribed in 65-85% of treated epileptic patients (6). In a study, Ogunniyi et al (12) in a hospital series at Ibadan in 1998 found that phenobarbitone was the single most commonly prescribed antiepileptic agent during that period. The World Health Organization reported carbamazepine as the third most prescribed AED in developing countries and is prescribed for only 5 to 20% of cases (6). However, the use of carbamazepine is gaining acceptance due to its favorable anticonvulsant efficacy and supplementary psychotropic use (13) and this might in part explain the high use of carbamazepine found in our study. This is further supported by a recent finding in a study conducted in Ilorin, Nigeria by Sanya and Musa (17) on private practitioners’ perspective of epilepsy management that 64.8% of the respondents prescribed carbamazepine, while 25.4% and 14.1% prescribed phenobarbitone and phenytoin respectively. Antiepileptic drug monotherapy was used by all the patients in this study who were still on AEDs at the time of survey. This is encouraging as monotherapy should be the aim for most people with epilepsy (19). Optimum seizure control can be obtained with a single drug for between 70% and 80% of patients (18, 19). The frequency of seizure was high among the PWE in our study. The majority of those with active epilepsy (82.8%) had more than one seizure episode per month. There was no statistically significant difference between the episodes of seizures in those using AEDs and those not receiving AEDs at the time of survey. Though the number of persons in this study that were on AEDs was few to make reasonable conclusions, various factors which may be patient related or health care related however, are known to contribute to poor seizure control in epilepsy. The major health care related problem identified in our study was under dosage. The patients in our study on AEDs at the time of the survey were grossly under dosed. The maximum dosages of the drugs were carbamazepine 200mg daily (plain not controlled release formulation) and phenobarbitone 60mg daily despite continuing seizures. Antiepileptic drugs are highly successful in suppressing seizures in most patients and with probable adequate dosing and education of both the patients and health care providers in this community epilepsy control will be improved. Another health care related factor that may have also contributed to the poor seizure control was the choice of antiepileptic drug used. Carbamazepine was used for three patients we found to be having primarily generalized seizure based on clinical assessment using the ILAE guidelines. Self withdrawal from AED therapy was high in our study. We found that 37.9% (n=11) of the persons with active epilepsy had used AEDs previously but had stopped at the time of study. This is higher than 27% reported by Aziz et al (1) in a mixed rural and urban community in Turkey. The major reason found in this study to be responsible for permanently discontinuing AEDs was patients’ dissatisfaction arising from the continuity of the seizures despite the use of AEDs. Other workers have also reported in the past that the majority of patients who permanently discontinue their antiepileptic medication do so of their own accord (4, 7). About one-third (37.9%) of the persons with active epilepsy in our study had never used antiepileptic drugs, this is similar to other reports were up to one-third of the epileptic population were never on medication (16). CONCLUSION Active epilepsy was prevalent in this suburban community in Southeast Nigeria. Among the PWE less than one third were receiving treatment with AEDs. Seizure frequency has high even among those receiving AEDs. More than a quarter of the PWE had never been treated with antiepileptic while more than half of those who were started on antiepileptic drug have discontinued of their own accord despite continuing fits. Table 1 Patterns of Use of Antiepileptic Drugs
(a) Analysis limited to those using AEDs at time of survey because of problems of recall. However three patients with active epilepsy had used phenytoin before the time of survey. Table 2 Seizure duration and control
(a) Seizure frequency the year prior to survey Table 3 Seizure frequency and Antiepileptic drug (AEDs).
Fisher’s exact test (2-sided) P =1.0 Table 4 Seizure type and type of antiepileptic drug prescribed
Fisher’s exact test (2-sided) P =1.0 Dr DIDIER MUDJIR BALANDAIn memoriam Dr Didier Mudjir Balanda
Le 27 septembre 2012, Didier Mudjir Balanda de son nom complet est décédé. Ce triste jour un collègue et un homme de valeurs nous a quitté. La neurochirurgie congolaise et africaine sont endeuillées. Né le 26 février 1968 à Kinshasa, Didier fait ses études primaires et secondaires à Kinshasa. Il entreprend ensuite des études de médecine à l’Université de Kinshasa où il sort diplômé en 1995. Résident en chirurgie à la Clinique Ngaliema entre 1995 et 2002, il entre en contact avec la neurochirurgie pour laquelle il montre un intérêt et des aptitudes certaines. Il se marie avec une consur, le Dr Rose Tambwe. De leur union naissent trois enfants : Amina, Titine, et David. En 2007, Didier Mudjir rentre à Kinshasa, exerce à la Clinique Ngaliema et reprend avec succès le service de Neurochirurgie. Etant à l’époque l’un des deux seuls neurochirurgiens pour le pays entier, il est consultant dans différents centres hospitaliers. Il prend une part active à différents activités de la WFNS, la AFNS et la PAANS. D’un point de vue humain, le Dr Mudjir Balanda était un homme droit, toujours disponible pour aider son prochain et particulièrement lorsque celui-ci se trouvait être un patient. Didier était très apprécié par ses collègues pour sa gentillesse. Le microcosme neurochirurgical africain perd un de ses jeunes membres très prometteur. Que sa famille et ses patients trouvent ici nos sincères condoléances et encouragements pour la perte de cet être cher et attachant. Pr Jean-Pierre Kalala Okito ABSTRACT Introduction Study Design and Site Objectives Patients and Methods Results Conclusion Key Words: Pituitary tumors, Trans-sphenoidal, Hypophysectomy, Craniotomy INTRODUCTION Pituitary adenomas account for 10 to 15 % of all intracranial tumors and in addition to suprasellar tumors such as craniopharyngiomas, meningiomas, germinomas and low grade gliomas, account for a significant portion of the surgical workload of any neurosurgical practice30. Tumors of the suprasellar region assume importance because of their anatomical proximity to the anterior visual apparatus and neuroendocrine structures (the pituitary gland and hypothalamus) which influences their clinical presentation and progression. Surgical extirpation is the treatment of choice for pituitary adenomas and other types of tumors of the sellar region and clivus. Pituitary and sellar mass lesions presenting with chiasmatic syndrome, ophthalmoplegia, pituitary apoplexia or endocrine derangement can undergo successful surgical removal34. Access to the pituitary may be achieved by craniotomy via subfrontal, pterional and sub-temporal approaches. In addition, the transsphenoidal route is widely accepted as the approach of choice for intrasellar lesions and some centers have also advocated the transsphenoidal route for tumors with subdiaphragmatic origin and subsequent suprasellar extension9. These subdiaphragmatic lesions are thought to be more easily removed by a transsphenoidal approach because the expanded sella provides a widened aperture to the suprasellar compartment and also diaphragmatic protection from pial invasion26. Further, the transsphenoidal approach has a number of variations, including the sublabial transseptal, transnasal endoscopic, endonasal rhinoseptoplastic, and transnasal septal displacement26, 37. However, despite the major advances, reported success rates and low morbidity and mortality, there is a paucity of local data regarding the Kenyan experience and outcomes of this popular procedure. Kenyatta National Hospital is a teaching and referral hospital with a bed capacity of over 2000 patients. Through this centre the majority of neurosurgical referrals are managed. We reviewed the records of patients who were treated for pituitary tumors in the neurosurgical unit. METHODS Following ethical approval, the records of patients who presented to the Kenyatta National Hospital and underwent surgery for pituitary lesions from June 2000 to June 2010 were retrieved and reviewed. Patient biodata, type and duration of symptoms, hormonal profile and management modalities were recorded in a pre-formed questionnaire. A data entry interface was created through which codified data was entered and data analysis carried out using Statistical Package for Social Sciences (SPSS) version 16.0. RESULTS Biodata and Clinical Presentation The mean age was 36.88 (+ 14.689) with a range from 2 years and 6 months to 72 years. Majority of the patients (55%) were aged between 26 and 45 years whereas pediatric patients (aged less than 13 years) and elderly patients (over 61 years) accounted for 5% each (Figure 2). The most common presentation were visual disturbances reported with 57 (87.7%) of the patients having reduction in visual acuity, while 37 (56.9%) had bitemporal hemianopia on confrontational and formal perimetry. Fundoscopy findings were reported for 39 patients with 24 (61.5%) of these being normal and optic atrophy and papilledema being reported for 29% and 9.5% respectively. The right and left eyes were each affected in 8 cases (12.3%) with bilateral involvement in 41 (63.1%) and 8 patients had no ocular involvement. Forty eight patients (73.8%) reported headaches while only 6% and 5% reported vomiting or convulsion respectively. Amenorrhea and primary infertility were the presenting complaint of 11 (16.9%) patients while 14 (21.5%) and 8 (12.3%) had galactorrhea and gynecomastia respectively. Ten patients (15.4%) had acromegalic features of hypergnathia and enlarged hands and feet. In addition, 9 (13.8%) patients had erectile dysfunction, while 4 (6.2%) had atrophic testes with gynoid habitus and female hair distribution (Figure 3). One patient aged two years and six months presented with features of precocious puberty. She had progressive breast development since eight months of age and at presentation was at tanner stage IV with growth of pubic hair from 11 months of age. In addition she experienced monthly mensrual-like flow from 1 year of age and had a post-pubertal uterus on ultrasound. She was however reported to have a normal growth rate. Admission blood pressures were measured and recorded for all the patients and were classified using the World Health Organisation-International Society of Hypertension guidelines. Majority of the patients (65%) had optimal blood pressures while 7.5% and 5% had moderate and severe hypertension (figure 4). Also recorded were admission random blood sugars, of which 49 (75%) were normoglycemic and 12.5% each were gucose intolerant and within diabetic range each (Figure 5). Data of the hormonal profile was also retrieved where available. Prolactin levels were recorded for 47 patients with 22 (46.8%) of them having hyperprolactinemia as compared to 21 (44.7%) and 4 (8.5%) having normal and low levels respectively. Majority of the patients were euthyroid (72.4%) while 10.3% and 17.3% were hyperthyroid and hypothyroid respectively. Cortisol levels were recorded for 41 patients of whom 4 had hypercortisolemia levels and 9 had normal with 8 patients having low levels (Table 1). With regards to imaging, all the patients included in the study had a CT scan done while a further 8 (12%) and 5 (7.7%) had an MRI and 4-vessel angiography done respectively. The location of the lesion was described as completely intrasellar 15 (23.1%), sellar with suprasellar extension 40 (61.5%), suprasellar 5 (7.7%) or sellar with supra-, infra- and parasellar extension 5 (7.7%) (Figure 6). Sixty two (95.4%) patients were operated during the study period, of these 28 (45.2%) by the transsphenoidal approach as opposed to 34 (54.85%) by craniotomy. In addition, there were 2 patients who had initially undergone transsphenoidal hypohysectomy who were re-operated transcranially for recurrences at 2 years and 4 years. The three patients who were not operated are included in the table below: The pterional trans-sylvian approach was the most frequent of transcranial hypohysectomies accounting for 17 (50%) of these operations. Further, 15 patients (44.1%) were operated by the subfrontal approach with frontal lobe retraction and two patients were operated via midline trans-callosal approach. With regards to the 28 patients operated trans-sphenoidally, majority 27 (96.4%) were by sub-labial incision with blunt dissection up to the maxilla and nasal crest. Septal mucosa was then stripped up to the vomer which was excised. The ostia of the sphenoid were then identified, the body of sphenoid nibbled and the floor of the sella turcica opened. The tumor was then exposed, biopsied and removed by curette and suction. One 37 year old patient who developed progressive blindness, erectile dysfunction and general weakness for 2 years had a pituitary tumor on CT and MRI with a sellar component, suprasellar extension, sphenoid bone erosion obliterating the sphenoid sinus and extension to both cavernous sinuses. He was scheduled for endonasal endoscopic biopsy as he was a poor anaesthetic risk for general anaesthesia due to persistent hypotension secondary to adrenocortical insufficiency. Fifty (76.9%) of the patients in this series had good functional outcome with marked improvement in visual function, normalised post-operative hormone levels and regression of symptoms while 11 (16.9%) and 4 (6.2%) suffered moderate and severe disability respectively. There was no early post-operative mortality among this cohort. There was no statistically significant difference in outcome between patients of different sex (p=0.058). However, patients’ age was a significant indicator of outcome. Pediatric patients in this series had good functional outcome in comparison to patients above 61 years who developed severe disability (p=0.0029). In addition, the duration of symptoms prior to surgery significantly affected patient outcome (p=0.0018). Majority of the patients (24) who presented within 6 months had good outcome compared to none of the patients who presented after 5 years of symptoms. Findings on fundoscopy had a significant on visual outcome as patients in whom optic atrophy was reported had a higher incidence of blindness and thus severe disability in comparison with those in whom the fundoscopy was normal. Patients who were operated had a higher incidence of good functional outcome as compared to those managed conservatively (p=0.001) irrespective of the type of operation performed (p=0.191). Transient fluid-electrolyte imbalance and diabetes insipidus (DI) was the most common postoperative complication (7.7% of the patients) in the present series. Hypothyroidism occurred in 6.2% of the patients as the second most common complication. In addition 2 patients has recurrences of tumor with clinical and radiological evidence at 2 and 4 years and had to undergo craniotomy and excision. Post-operative rhinorrhea was reported in 6.2% of the patients and was managed conservatively. DISCUSSION Although pituitary tumors are the most commonly encountered intracranial neoplasms, their true incidence has not been established with certainty. In literature, the prevalence of these tumors in autopsy series is reported to be 5-20%7, 27, 32 while most recent series estimate the prevalence of clinically apparent pituitary lesions to comprise approximately 10-15 % of all intracranial lesions10, 18. Improvement in radiographic imaging, biochemical detection of hormonal abnormalities, and microsurgical techniques have raised the number of surgical procedures, and in some series pituitary adenomas represent approximately 25% of surgically resected intracranial neoplasms; however, this may reflect a bias that reflects the interests of the surgeon or institution. In the current study, there is a slight majority of 39 (60%) female as compared to 26 (40%) male patients. Previous studies report that pituitary tumors tend to afflict both sexes equally3, 5, 18. In addition, the mean age was 36.88 years (+ 14.689) with most of the patients (55%) were aged between 26 and 45 years and fewer patients at both extremes of age. There is a wide range of reported mean ages in literature ranging from 39.8 years40 to 50.4 years10. Reported incidence rates demonstrate an increase with age for both clinically apparent and autopsy diagnosis of pituitary tumors. In this regard, autopsy analyses and imaging studies report that more than 30% of people 50 – 60 yr of age harbor clinically undetected tumors 5, 7, 28, 31. Further, it is widely reported that pituitary adenomas are infrequent in childhood accounting for only about 3.5- 8.5% of pituitary adenomas which are diagnosed before the age of 20 yr 23, 33. Childhood tumors exhibit a female preponderance, and it has been suggested that they are smaller, less invasive, and less aggressive than tumors of adults23. Patients with pituitary tumors present with signs and symptoms related to mechanical effects of an expanding tumor within the sella turcica (headaches, visual disturbances and cranial nerve palsies), excessive or impaired hormone production3. The most common presentation in this series, were visual disturbances reported by 57 (87.7%) of the patients with reduction in visual acuity. Chang10 reported that in an American population, over one half of patients presented with visual disturbance while other studies have reported a prevalence rate of up to 90%19, 39. The classic bitemporal field loss is found in chiasmatic compression and was described by 37 (56.9%) of the patients. These patients frequently complain of bumping into objects on one or both sides of the contracted visual field, reflecting both unilateral and bitemporal field loss. However, early compression may lead to upper quadrantic defects secondary to inferior chiasmal fiber compression. Central vision may be affected by direct compression of the intracranial optic nerve. This may present as a blurring of vision or scotomatous central field defects. This is more common in individuals with a “post-fixed” chiasm – an anatomical variation where the chiasm is situated further back, thus exposing more optic nerve to the compressive effects of an expanding adenoma 25. If compression has been longstanding, fundoscopy may reveal optic atrophy which was observed in 10% of the current population. In our study, 50 (87.7%) the patients had improved visual function following surgery. The reported results in literature of visual outcome after surgical management of pituitary and sellar tumors vary considerably among studies, with improvement rates ranging from 36 to 80% 2, 4, 20, 21, 24, 25. The choice for transphenoidal approach as opposed to craniotomy is determined by a number of factors including degree of suprasellar extension, cavernous sinus invasion, tumor consistency, brain invasion and cerebral edema as well as encasement of the optic apparatus41. Tumors with significant suprasellar extension, especially through the plane of the hypothalamus and floor of the third ventricle, have been correlated with significantly worse postoperative outcomes 14, 35. As such, particular features of suprasellar extension that mandate additional consideration prior to an operation are intraventricular extension, displacement or edema of the hypothalamus, displacement/compression of the proximal branches of the ACA, and involvement of the perforating arteries off the ICA and ACA1, 15, 17, 38. Firm tumor consistency creates an inherent limitation in the ability to completely deliver the suprasellar tumor component via any transsphenoidal approach. Tumor consistency remains one of the most important, yet elusive, factors in the consideration of an trans-sphenoidal versus open craniotomy for skull base tumors. If a tumor’s consistency is known to be fibrotic ahead of time (as in some cases of reoperation), thus making it less amenable to suction, dissection and gross total resection, this should provide added support for consideration of an open approach. On the contrary, a primarily cystic or hemorrhagic appearance on MR imaging, especially a fluid-fluid level, can often lend support to selecting a less invasive approach for sellar region tumors 16. In the future, a priori knowledge of tumor consistency may lend major support to the selection of a skull base approach from above versus below and warrants further research. CONCLUSION In conclusion, key advances have been made to improve the ability to safely treat patients with larger and increasingly complex tumors of the anterior and middle skull base since the re-emergence of the transsphenoidal approach. Nevertheless, patient selection remains of paramount importance in guiding the decision to perform a particular surgical approach for a given tumor, and it remains clear that, for the time being, some patients with large sellar and parasellar region tumors are better served by performing one of many variations of an open craniotomy (such as a pterional, frontoorbital, subfrontal, or interhemispheric approach)8. This study highlights the experience and outcomes following pituitary surgery in a Kenyan referral hospital. It demonstrates that good surgical outcomes can be achieved by both the trans-sphenoidal and craniotomy approaches based on the indications and tumor characteristics. There is a need to carry out a prospective study with closer assessment of hormonal profile and response to surgery as well as perioperative management and longer follow-up for outcome. It however, demonstrates the current clinical status and lays a foundation for further inquiry of this subject that is central to neurosurgical practice. 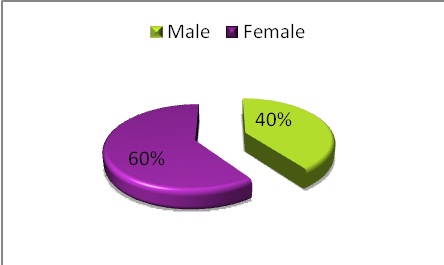 Figure 1: Illustration of the patient distribution by sex 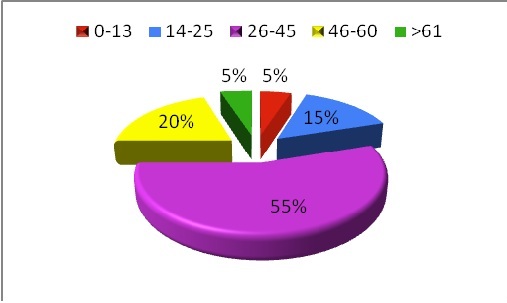 Figure 2: A pie chart demonstrating the distribution by age of patients with pituitary tumors managed at the neurosurgical unit. The majority of the patients were aged between 26-45 years. 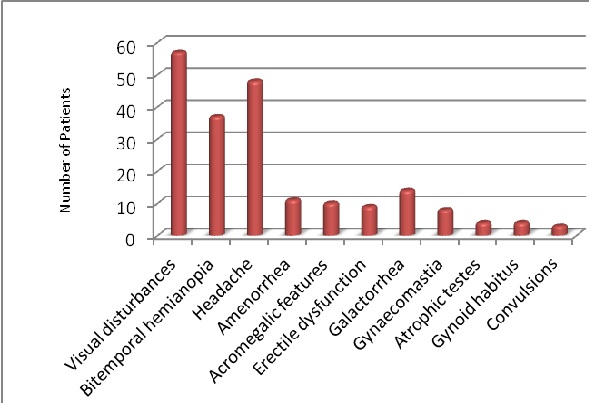 Figure 3: A bar graph showing the frequency of common presentations of patients with pituitary lesions 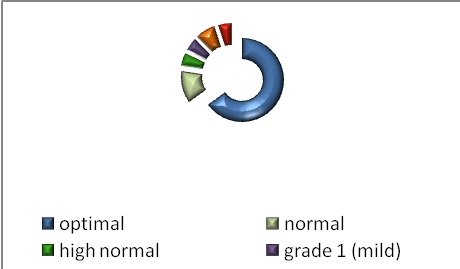 Figure 4: An illustration of the distribution of admission Blood Pressure accoring to the World Health Organisation-International Society of Hypertension guidelines. Grades 1, 2 and 3 refer to the severity of hypertension 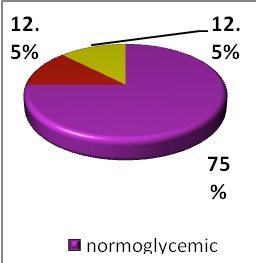 Figure 5: A pie chart representing the proportions of with the various blood sugar levels. Where normoglycemic refers to random blood sugars ¡Ü6.9mmol/L, glucose intolerance (7-11 mmol/L) and diabetes (¡Ý11.1 mmol/L). 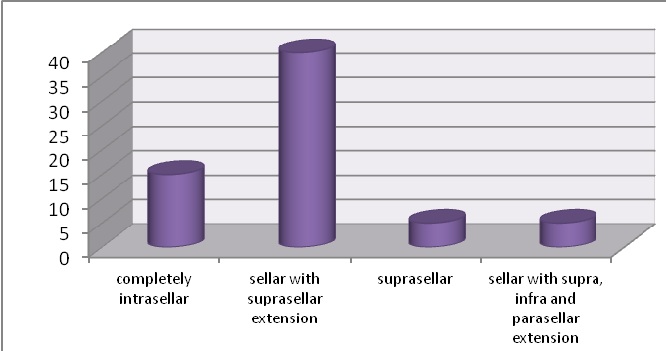 Figure 6: Location of pituitary lesions as seen on CT scan
Articles récents
Commentaires récents
Archives
CatégoriesMéta |
© 2002-2018 African Journal of Neurological Sciences.
All rights reserved. Terms of use.
Tous droits réservés. Termes d'Utilisation.
ISSN: 1992-2647
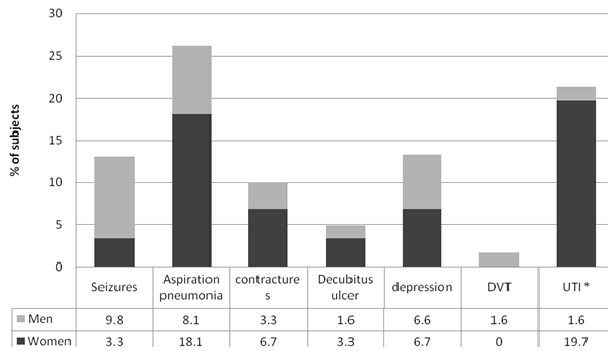 Figure 2. Stroke complications. Stacked bars are percentages of subjects with complications comparing sex groups. Asterisk * indicates P < 0.05.[/caption]
Figure 2. Stroke complications. Stacked bars are percentages of subjects with complications comparing sex groups. Asterisk * indicates P < 0.05.[/caption]





 #gallery-3 {
margin: auto;
}
#gallery-3 .gallery-item {
float: left;
margin-top: 10px;
text-align: center;
width: 33%;
}
#gallery-3 img {
border: 2px solid #cfcfcf;
}
#gallery-3 .gallery-caption {
margin-left: 0;
}
/* see gallery_shortcode() in wp-includes/media.php */
#gallery-3 {
margin: auto;
}
#gallery-3 .gallery-item {
float: left;
margin-top: 10px;
text-align: center;
width: 33%;
}
#gallery-3 img {
border: 2px solid #cfcfcf;
}
#gallery-3 .gallery-caption {
margin-left: 0;
}
/* see gallery_shortcode() in wp-includes/media.php */






